Prednisone: What You Need to Know About Steroid Use, Side Effects, and Safety
When you hear prednisone, a synthetic corticosteroid used to reduce inflammation and suppress the immune system. Also known as corticosteroid, it's one of the most commonly prescribed drugs for conditions like asthma, rheumatoid arthritis, and lupus. But prednisone isn’t a simple fix—it’s a tool with serious trade-offs. Many people take it for weeks or months without realizing how deeply it affects their body, from their eyes to their bones.
The real danger isn’t just the drug itself, but how quietly it damages you. Long-term steroid use can silently raise eye pressure, leading to steroid glaucoma, a form of glaucoma triggered by corticosteroids that can cause irreversible vision loss. It can also cloud the lens of your eye, causing steroid-induced cataracts, a type of cataract that develops faster in people on prolonged steroid therapy. These aren’t rare side effects—they’re common enough that doctors should be checking your eyes every 3 to 6 months if you’re on prednisone for more than a few weeks. And it’s not just your eyes. Prednisone leaches calcium from your bones, increasing fracture risk, especially in older adults or those taking it for over a year. That’s why bone density scans and calcium supplements often go hand-in-hand with long-term steroid treatment.
What makes prednisone tricky is that it’s often necessary. Stopping it suddenly can trigger adrenal crisis—your body can’t make enough natural steroids after being flooded with synthetic ones. That’s why tapering matters. But many people don’t know how to manage it. They might skip doses because they feel better, or they keep taking it long after the condition is under control. The real skill isn’t just in prescribing it, but in knowing when to stop, how to replace its effects safely, and how to monitor for damage before it’s too late.
Below, you’ll find real, practical advice from posts that dig into exactly these issues: how prednisone affects your vision, what alternatives exist, how to protect your bones, and why some people need to avoid it altogether. These aren’t theoretical guides—they’re based on patient experiences, clinical data, and what actually works in everyday care.
Published on Feb 21
3 Comments
Corticosteroids like prednisone offer fast relief for inflammation but carry serious long-term risks. Learn when they help, when they hurt, and how to use them safely.
Published on Dec 4
9 Comments
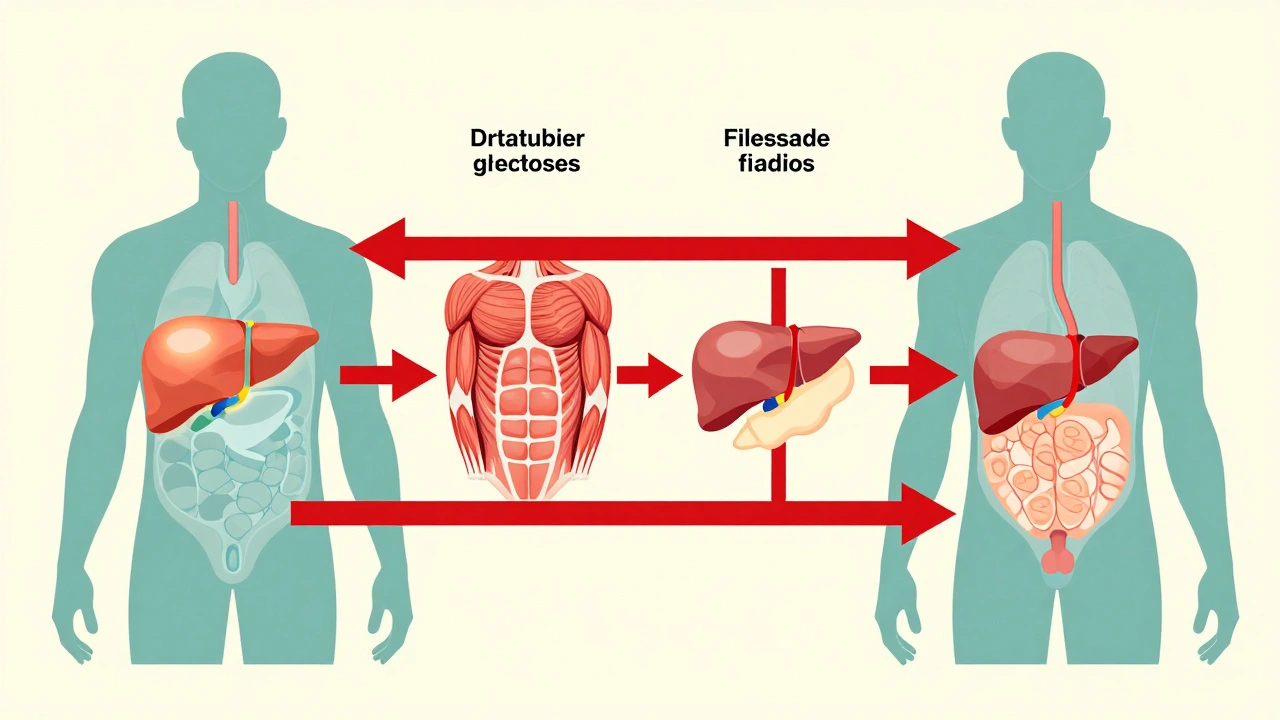
Corticosteroids like prednisone can cause sudden high blood sugar, even in people without diabetes. Learn how steroids trigger hyperglycemia, who’s at risk, and how to manage it safely with insulin, monitoring, and timely adjustments.