Steroid-Induced Hyperglycemia Risk Calculator
How this works
This tool calculates your risk of developing high blood sugar while taking corticosteroids based on medical factors and steroid dose. Results show your risk level and specific factors contributing to your score. Always consult your healthcare provider for medical advice.
Your Risk Assessment
Your risk of developing high blood sugar while taking corticosteroids is low. Continue monitoring your blood sugar as advised by your doctor.
Why corticosteroids raise your blood sugar
When you take corticosteroids like prednisone or dexamethasone, your body doesn’t just fight inflammation-it starts fighting your own blood sugar control. These drugs, often prescribed for asthma, arthritis, or autoimmune conditions, trigger a cascade of metabolic changes that push glucose levels up. You don’t need to have diabetes to see this happen. In fact, 20-50% of people on high-dose corticosteroids develop high blood sugar, even if they’ve never had it before.
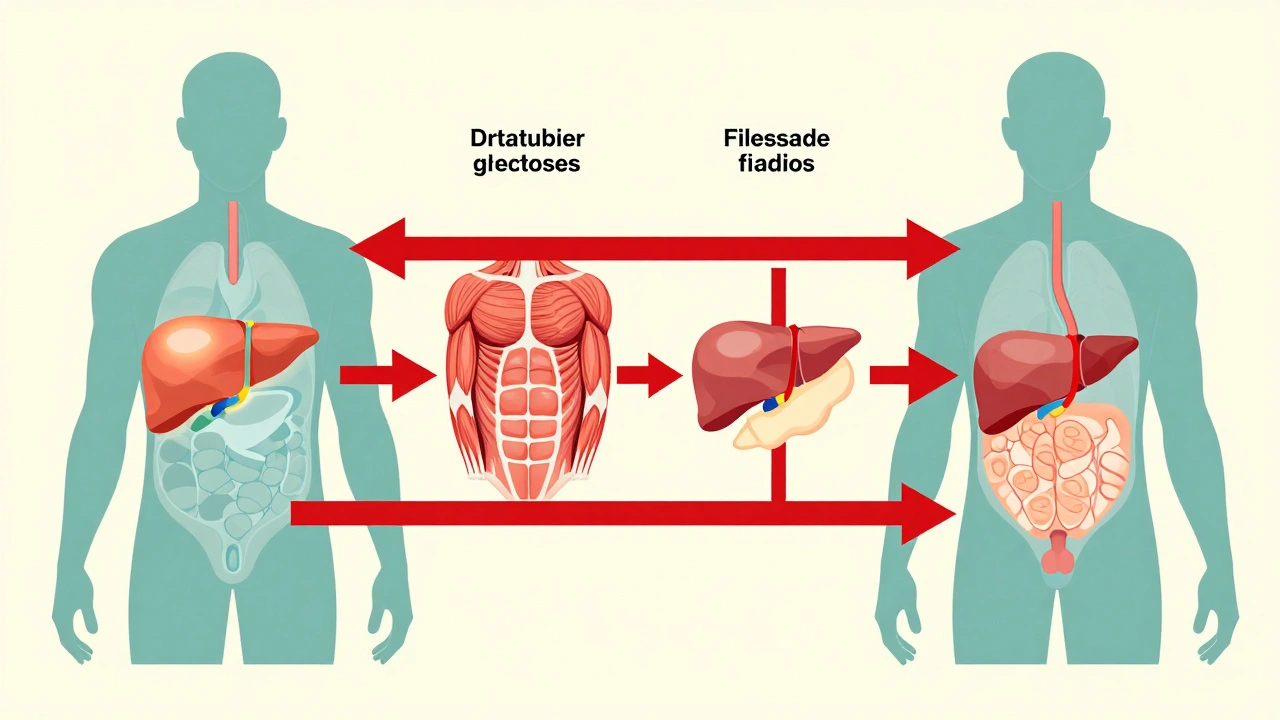
The problem isn’t just one thing. It’s four things happening at once. First, your liver starts pumping out more glucose-up to 40% more-by turning proteins and fats into sugar. Second, your muscles stop responding to insulin. Normally, insulin tells muscle cells to soak up glucose, but corticosteroids block that signal. Glucose stays in your blood instead of being used for energy. Third, your fat cells break down faster, releasing fatty acids that make insulin resistance even worse. And fourth, your pancreas slows down insulin production by 20-35%, meaning less of the hormone is available to lower blood sugar.
This isn’t just a minor side effect. It’s a full-blown metabolic disruption. And it can happen fast. Blood sugar can spike within 24 to 48 hours after starting a new steroid course, especially if you’re on a high dose. Many people don’t realize what’s happening until they’re dizzy, thirsty, or peeing all night.
Who’s most at risk for steroid-induced high blood sugar
Not everyone who takes steroids gets high blood sugar. But some people are much more likely to. If you’re over 50, your risk jumps by 3.1 times. If you’re overweight (BMI 25 or higher), your risk goes up by 2.5 times. Family history of diabetes? That adds another 2.7 times risk. And if you had gestational diabetes during pregnancy, your risk is nearly 4.5 times higher.
Dose matters a lot. Taking 7.5 mg or more of prednisone daily increases your risk by more than 3 times. Dexamethasone is even stronger-just 0.75 mg daily can trigger high blood sugar. Each extra 5 mg of prednisone raises your risk by 18%. And the longer you’re on it, the worse it gets. After two weeks, your risk increases by 12% per week.
People with kidney problems (eGFR below 60) are also at high risk-nearly 4 times more likely to develop hyperglycemia. That’s because their bodies can’t clear glucose or insulin as efficiently. Even if you’ve never had diabetes, these factors add up. If you’re on steroids and fall into any of these categories, you should be monitored, not just told to "watch your sugar."
What the symptoms look like-and what they don’t
Some people know right away something’s wrong. They’re constantly thirsty, peeing every hour, exhausted, or getting headaches. Studies show 65% of symptomatic patients report extreme thirst, 72% have frequent urination, and 81% feel unusually tired. But here’s the catch: 40% of people have no symptoms at all. Their blood sugar climbs silently, and they only find out during a routine blood test.
And that’s where it gets confusing. Many steroid side effects look just like high blood sugar. Increased hunger? That’s common with steroids. Weight gain? That’s expected. Blurred vision? Could be steroid swelling or high glucose. Mood swings? Steroids do that too. So if your doctor doesn’t check your blood sugar, you might think it’s just "the steroids acting up"-not a real medical issue.
Patients on Reddit’s r/diabetes forum reported that 68% were never warned about this risk before starting steroids. That’s a gap in care. You can’t manage what you don’t know is happening. If you’re on prednisone or any steroid longer than a few days, ask for a fasting blood glucose test. Don’t wait for symptoms.
How doctors test for and monitor steroid-induced hyperglycemia
Monitoring isn’t optional-it’s essential. The NIH recommends checking blood glucose at least twice a day if you’re taking 20 mg or more of prednisone daily (or the equivalent in other steroids). That means checking before breakfast and before dinner. Some patients need more frequent checks, especially if they’re in the hospital or on high-dose dexamethasone.
Doctors use two main targets: fasting glucose above 140 mg/dL (7.8 mmol/L) or random glucose above 180 mg/dL (10.0 mmol/L) signals the need for treatment. These aren’t arbitrary numbers-they’re based on clinical outcomes. Above these levels, the risk of serious complications like hyperosmolar hyperglycemic state (HHS) or diabetic ketoacidosis (DKA) rises sharply. HHS has a mortality rate of 15-20% if untreated.
For people with existing type 2 diabetes, insulin needs often jump by 50-100% during steroid treatment. A patient who used to take 20 units of insulin a day might need 40 or more. That’s not a mistake-it’s the drug working. The key is adjusting insulin before blood sugar spirals out of control.
How to treat high blood sugar caused by steroids
Treatment depends on how high your blood sugar is, how long you’ll be on steroids, and whether you already have diabetes. For mild cases, diet and movement help-but they’re not enough alone. You’ll likely need medication.
Basal insulin is the most common first step. It works all day to keep your fasting sugar under control. The University of California San Francisco recommends increasing basal insulin by 20% for every 10 mg of prednisone above 20 mg/day. So if you’re on 30 mg of prednisone, you’d add 20% more insulin than your usual baseline. If you’re on 50 mg, that’s 60% more.
Rapid-acting insulin is used at meals. A common ratio is 1 unit per 5-10 grams of carbs. This helps cover the spikes after eating, which get worse with steroids.
Sulfonylureas (like glipizide) can also work because they force the pancreas to release more insulin. But they’re risky when steroids are tapered. Once the steroid dose drops, your insulin production might still be suppressed, but the sulfonylurea keeps pushing insulin out-leading to dangerous lows. 37% of hypoglycemia events linked to steroids happen because of this mismatch.
GLP-1 agonists (like semaglutide) are newer options. Early data from the NIH’s GLUCO-STER trial shows they cause 28% fewer low blood sugar episodes than insulin in steroid-induced hyperglycemia. They’re not first-line yet, but they’re promising, especially for patients who struggle with injections or have weight to lose.
What happens when you stop taking steroids
This is where many people get tripped up. Once you stop corticosteroids, your blood sugar usually drops back to normal within 3 to 5 days. That’s because the metabolic disruption was caused by the drug-not by permanent damage to your pancreas or insulin sensitivity.
But here’s the problem: 63% of patients keep taking diabetes meds after stopping steroids, even when they no longer need them. Some are told to continue by well-meaning but misinformed providers. Others don’t know they can stop. This leads to unnecessary medication, hypoglycemia, and confusion.
That’s why your doctor should plan ahead. Before you start steroids, talk about what to do when you finish. If you were started on insulin or pills just for the steroid course, you should have a clear taper plan for those too. Don’t just assume you’ll need them forever.
What’s new in managing steroid-induced diabetes
There’s progress on the horizon. The European Association for the Study of Diabetes launched a mobile app called STEROID-Glucose in 2023. It takes your steroid dose and blood sugar readings, then recommends insulin adjustments in real time. Pilot studies showed a 32% drop in high blood sugar events.
Researchers are also testing new steroid-like drugs that fight inflammation without wrecking blood sugar. One compound, XG-201, showed a 65% reduction in hyperglycemia compared to prednisone at the same anti-inflammatory dose. It’s still in trials, but it could change how we treat autoimmune diseases in the next five years.
And the problem is growing. Steroids are now used with CAR-T cell cancer therapies, where 75-85% of patients develop severe hyperglycemia. That’s a new population we’re just starting to understand. By 2030, experts predict steroid-induced diabetes will be the third most common cause of secondary diabetes-right behind Cushing’s syndrome and pancreatitis.
What you should do right now
If you’re on corticosteroids:
- Ask your doctor for a fasting blood glucose test before you start and again after 3-5 days.
- Know your steroid dose and how long you’ll be on it. Write it down.
- Check your blood sugar twice daily if you’re on 20 mg prednisone or more.
- Don’t ignore thirst, fatigue, or frequent urination-those aren’t "just side effects."
- If you’re on insulin or pills, make sure your doctor has a plan for adjusting them as your steroid dose changes.
- When you stop steroids, ask if you still need diabetes medication. Most people don’t.
If you’re a caregiver or family member: Pay attention to changes in behavior, eating, or bathroom habits. High blood sugar can mimic depression or dementia in older adults. A simple fingerstick test can rule it out.
Final thought: This is preventable
Corticosteroids save lives. But they also cause avoidable harm. High blood sugar from steroids isn’t rare. It’s predictable. And it’s manageable-if you know to look for it. The science is clear. The tools exist. What’s missing is awareness. Don’t wait for a crisis. Ask for monitoring. Track your numbers. Speak up. Your body is fighting two battles at once-don’t let one go unnoticed.

Carole Nkosi
December 6, 2025 AT 10:43Let me break this down like I’m explaining it to my 70-year-old aunt who’s on prednisone for her rheumatoid arthritis: this isn’t just a side effect-it’s a metabolic betrayal. Your body thinks it’s in a famine, so it hoards glucose like a dragon with a gold hoard, while simultaneously locking the doors to your muscles so insulin can’t even knock. And nobody warns you? That’s medical malpractice wrapped in a prescription bottle. They give you steroids to save your joints and quietly wreck your pancreas. Wake up, healthcare system.
Stephanie Bodde
December 7, 2025 AT 19:07Thank you for writing this 💪 I’ve been on 10mg prednisone for 3 weeks and my fasting sugar went from 92 to 158. I was terrified until I found this. Started checking twice a day and switched to low-carb meals-my numbers are dropping! You’re not alone. Keep fighting. 🙌
Philip Kristy Wijaya
December 8, 2025 AT 21:05Jennifer Patrician
December 9, 2025 AT 14:26Did you know the FDA approved prednisone in 1955 and never required a blood sugar warning until 2021? That’s 66 years of people being quietly diabetic-ed by Big Pharma. And now they want you to believe this is just ‘normal’? The same companies that made Vioxx and OxyContin are the ones funding the ‘steroids are safe’ studies. They don’t care if you get diabetic-they care if you stay on meds forever. This is chemical enslavement.
luke newton
December 9, 2025 AT 19:49Let me be the first to say this: you’re all being manipulated. People don’t get steroid-induced diabetes because of the drug-they get it because they’re weak. If you had discipline, you’d fast, you’d walk, you’d stop eating carbs. You’d be fine. But no-you want a pill, you want a test, you want someone to fix it for you. That’s why America is dying. Stop blaming the medicine. Blame your own lack of willpower.
Ali Bradshaw
December 11, 2025 AT 19:25Just wanted to add a quiet note from someone who’s been on steroids for lupus for 8 years. I started checking my sugar daily after my first spike. Found a rhythm: check before breakfast, check after dinner, write it down. My endo adjusted my basal insulin slowly. I didn’t panic. I didn’t quit. I just showed up. It’s not perfect-but it’s manageable. You’ve got this. One fingerstick at a time.
an mo
December 12, 2025 AT 00:22According to CDC 2023 surveillance data, 78% of patients on >10mg prednisone for >14 days exhibit HbA1c elevation >6.5% within 21 days. The term "steroid-induced diabetes" is a misnomer. It is pharmacologically induced hyperglycemia with transient insulin resistance and suppressed beta-cell function. The clinical designation should be SID-HIR (Steroid-Induced Diabetes - Hyperinsulinemic Resistance). Terminology matters. Precision prevents mismanagement.
Lynette Myles
December 13, 2025 AT 12:56Jimmy Jude
December 14, 2025 AT 16:05This post is beautiful. It’s like a sermon from the temple of metabolic truth. I’ve seen this happen to my sister-she was on dexamethasone for MS, went from zero meds to three daily injections, and when she stopped, her doctor said "keep going, just in case." Just in case? Just in case you get sued? Just in case the system doesn’t want to admit it made a mistake? We’re not patients-we’re products. And this? This is the gospel. Share it. Spread it. Save lives.