Upper GI Bleeding Prevention: Key Strategies and Medications That Work
When it comes to upper GI bleeding prevention, the process of reducing the risk of life-threatening bleeding in the upper digestive tract, often caused by ulcers, inflammation, or medication side effects. Also known as upper gastrointestinal hemorrhage prevention, it’s not just about treating symptoms—it’s about stopping the problem before it starts. Many people don’t realize that everyday choices—like taking ibuprofen for a headache or skipping treatment for heartburn—can quietly raise their risk. Upper GI bleeding isn’t rare. It lands tens of thousands in hospitals every year, and most cases are preventable.
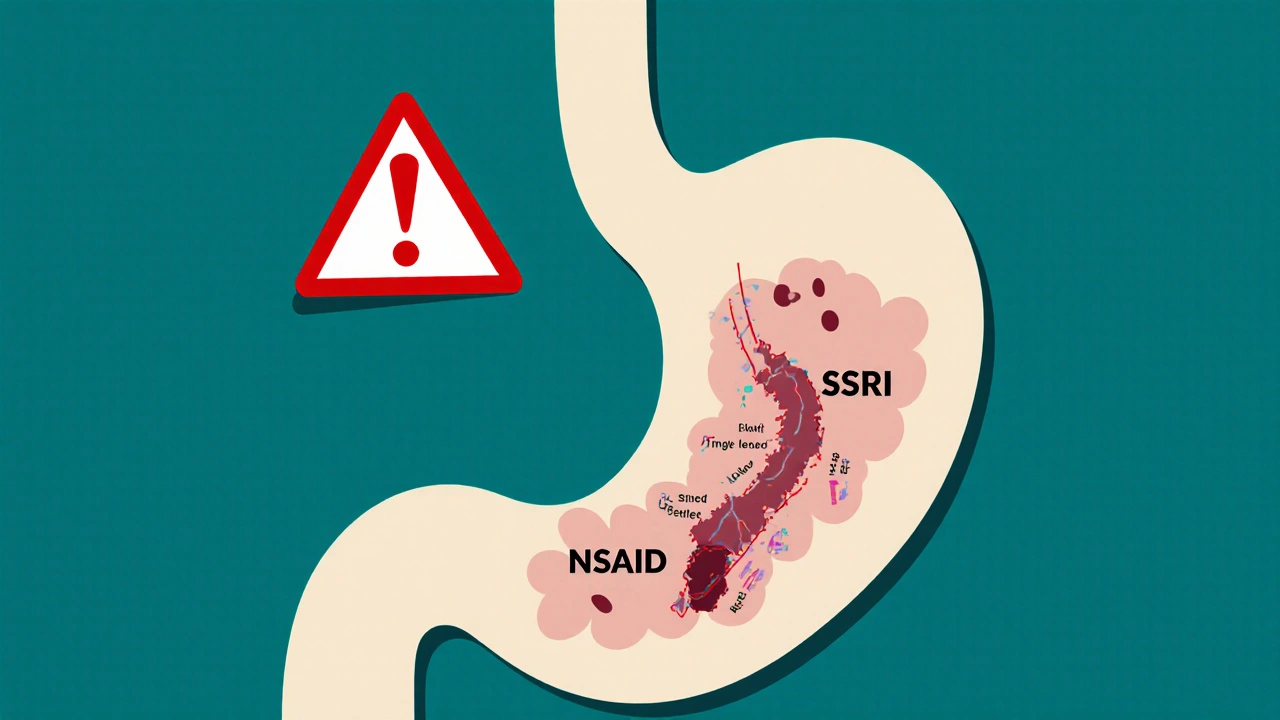
The biggest culprits? peptic ulcers, open sores in the stomach or duodenum, often caused by H. pylori bacteria or long-term NSAID use. Also known as stomach ulcers, they’re the leading cause of upper GI bleeding. Then there’s NSAIDs, nonsteroidal anti-inflammatory drugs like aspirin, ibuprofen, and naproxen that irritate the stomach lining and block protective prostaglandins. Also known as painkillers, they’re everywhere—from medicine cabinets to daily routines. And let’s not forget H. pylori, a bacteria that lives in the stomach of nearly half the world’s population and can silently damage the mucosal barrier. Also known as Helicobacter pylori, it’s responsible for up to 80% of ulcers. These three are the core trio you need to manage if you want to avoid bleeding.
Prevention isn’t guesswork. It’s simple, repeatable steps. If you’re on daily NSAIDs for arthritis or back pain, talk to your doctor about switching to acetaminophen or adding a proton pump inhibitor, a class of drugs like omeprazole or esomeprazole that shut down stomach acid production to protect the lining. Also known as PPIs, they’re the gold standard for ulcer prevention in high-risk patients. If you’ve had an ulcer before, testing for H. pylori isn’t optional—it’s critical. Erase the bacteria, and you cut your recurrence risk by more than half. Even if you don’t have symptoms, chronic heartburn or unexplained nausea could be early warning signs. Don’t wait for vomiting blood to take action.
It’s not just about pills. Lifestyle changes matter too. Smoking doubles your bleeding risk. Alcohol doesn’t just hurt your liver—it erodes your stomach lining. Stress won’t cause an ulcer, but it can make one bleed faster. Eating regular meals, avoiding late-night snacks, and cutting back on spicy foods aren’t just old wives’ tales—they’re backed by clinical data. And if you’re over 60, on blood thinners, or have kidney disease, your risk profile changes. You need a personalized plan, not a generic one.
The posts below cover exactly these topics. You’ll find real comparisons between drugs like meloxicam and PPIs, how chronic inflammation plays into ulcer risk, and how to safely manage medications like Diltiazem or Precose if you’re already at risk. No fluff. No theory. Just what works for people who’ve been there. Whether you’re managing your own health or helping someone else, these guides give you the tools to act before the next bleed happens.
Published on Oct 30
8 Comments
Combining SSRIs and NSAIDs can raise your risk of dangerous GI bleeding by 75%. Learn why this happens, who’s most at risk, and how to protect yourself with safer pain relief and proven prevention strategies.