GI Bleeding Risk Calculator
Assess Your Risk
Enter your details to determine your risk level and receive personalized safety recommendations.
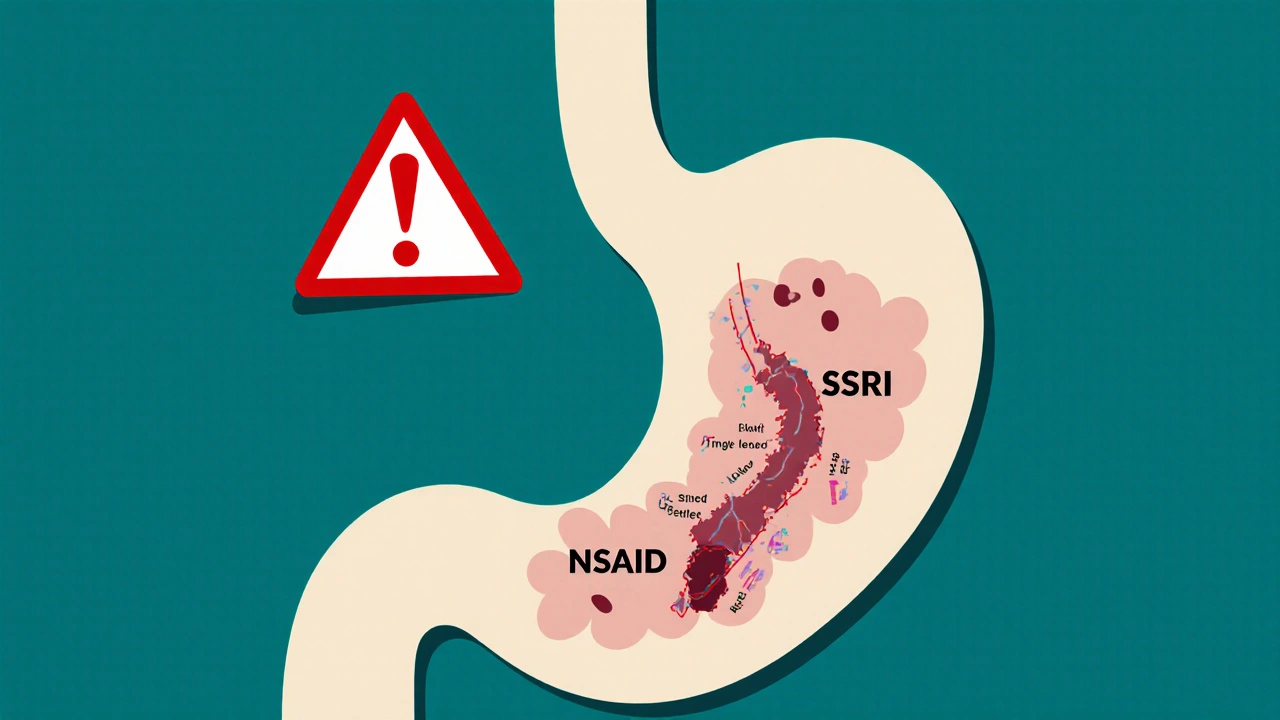
It’s not rare to take an SSRI for depression or anxiety and an NSAID for aching knees or chronic headaches. Millions of people do it every day. But here’s something most don’t know: combining these two common drugs can sharply increase your risk of a dangerous gastrointestinal bleed - one that might land you in the hospital with black, tarry stools, vomiting blood, or sudden dizziness from internal blood loss.
Why This Combination Is Riskier Than You Think
SSRIs like sertraline, fluoxetine, and citalopram work by boosting serotonin in the brain. But serotonin isn’t just a mood chemical - it’s also critical for blood clotting. Platelets, the cells that seal up cuts in your blood vessels, need serotonin to stick together and stop bleeding. SSRIs block serotonin from being taken back up into platelets, leaving them less able to do their job. This means even a small scratch in your stomach lining can turn into a slow, unnoticed bleed. NSAIDs like ibuprofen, naproxen, and diclofenac work differently but just as dangerously. They shut down enzymes (COX-1) that make protective mucus and blood flow in your stomach lining. Without that shield, stomach acid eats away at your tissue. Over time, this can cause ulcers. When you add an SSRI on top, you’re not just damaging the lining - you’re also disabling your body’s ability to stop the bleeding. The result? A dangerous synergy. Studies show that taking both together increases your risk of upper GI bleeding by 75% compared to taking either alone. That’s not a small bump. That’s a major jump. For someone over 65 with a past ulcer, the risk can be even higher - sometimes more than triple.Not All SSRIs or NSAIDs Are Equal
You might assume all SSRIs carry the same risk. They mostly do. But some data suggests escitalopram might be slightly less likely to interfere with platelets than fluvoxamine or paroxetine - though the difference is small enough that you shouldn’t rely on it for safety. NSAIDs vary a lot more. Naproxen and diclofenac are the worst offenders for stomach damage. Ibuprofen is a bit safer - but still risky when paired with an SSRI. Celecoxib, a COX-2 selective NSAID, stands out. It doesn’t hit COX-1 as hard, so it causes far less mucosal damage. Studies show its bleeding risk is nearly the same as taking a placebo. For someone needing long-term pain relief and an SSRI, celecoxib is the best NSAID option. But here’s the catch: celecoxib isn’t cheap, and it’s not always covered by insurance. Plus, it’s not risk-free for your heart. So it’s not a magic bullet - just the safest NSAID option for your stomach.Who’s Most at Risk?
This isn’t a problem for everyone. But certain people are sitting on a ticking time bomb:- People over 65
- Those with a history of peptic ulcers or GI bleeding
- Patients on blood thinners like warfarin or aspirin (even low-dose)
- People taking corticosteroids (like prednisone)
- Those with H. pylori infection - a common stomach bacteria that worsens ulcers
What Doctors Often Miss
A 2021 survey of over 1,200 primary care doctors found that only 38.7% routinely check for this interaction. Even fewer - just 22.3% - prescribe protective meds when both drugs are needed. Why? Because it’s easy to overlook. Depression and arthritis are common. Prescribing an SSRI and an NSAID feels routine. But this interaction is one of the most underrecognized dangers in primary care. Patients rarely bring it up. And unless a doctor specifically asks about over-the-counter pain meds, they won’t know you’re taking ibuprofen daily for back pain. Reddit threads and patient forums are full of stories like this: someone on sertraline starts taking Advil for a bad shoulder. A few weeks later, they’re vomiting dark blood. ER visit. Endoscopy. Diagnosis: bleeding ulcer. They didn’t know the two drugs could do this.How to Prevent It - Step by Step
If you’re on both an SSRI and an NSAID, here’s what you need to do:- Ask yourself: Do I really need the NSAID? Can you switch to acetaminophen (Tylenol)? It doesn’t hurt your stomach lining or affect platelets. For many types of pain - headaches, muscle aches, joint stiffness - it works just as well without the bleeding risk.
- If you must keep the NSAID, pick the safest one. Celecoxib is the top choice. If that’s not available or affordable, ibuprofen is the next best. Avoid naproxen, diclofenac, and piroxicam.
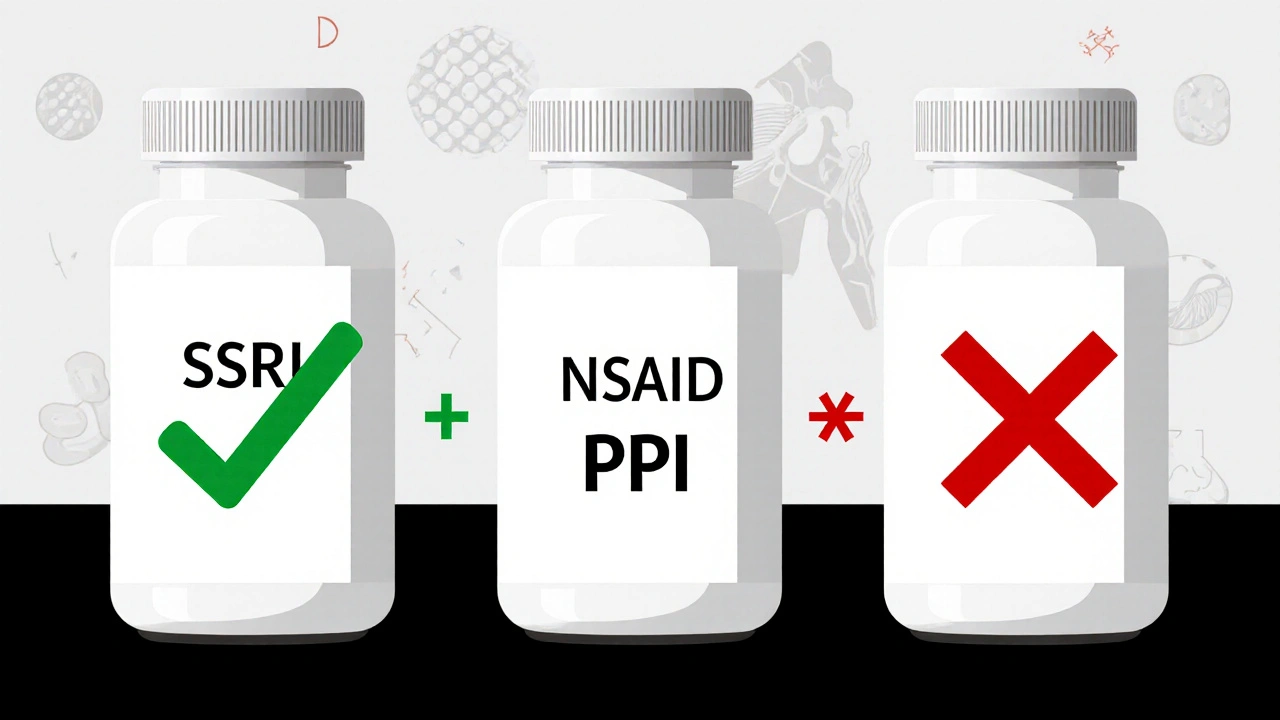
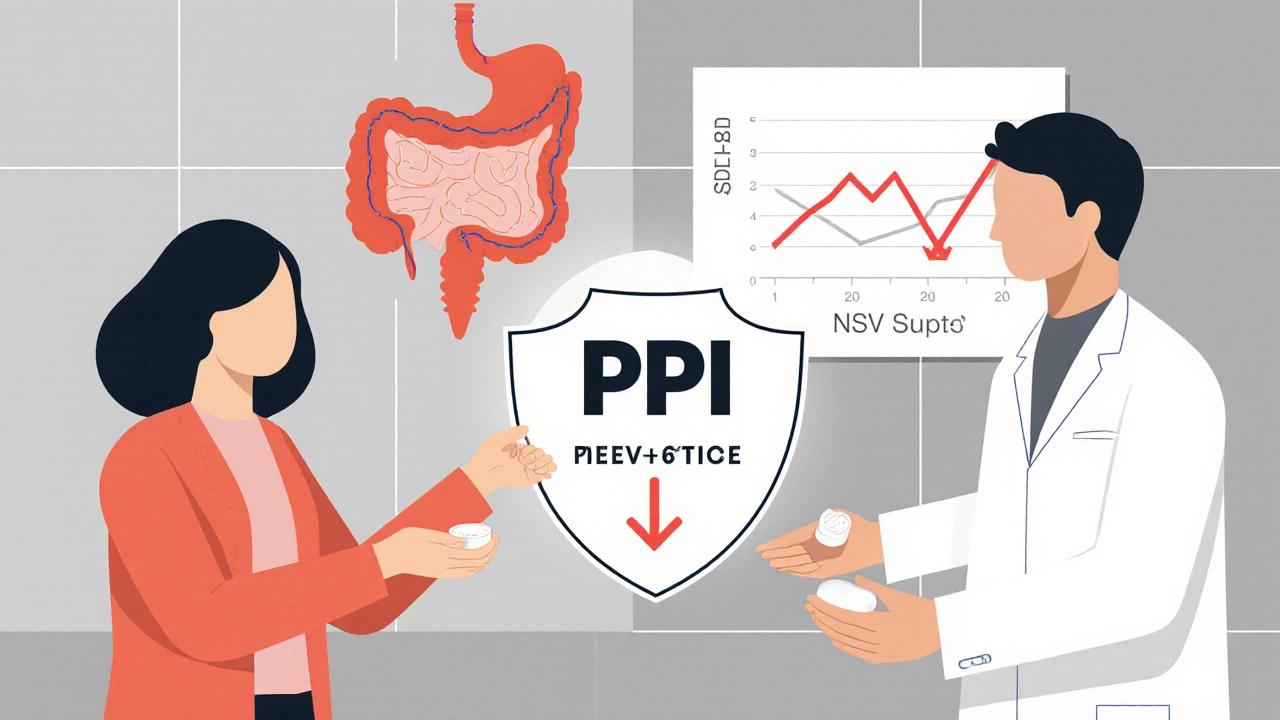
- Take a proton pump inhibitor (PPI) every day. Omeprazole 20mg, esomeprazole 20mg, or pantoprazole 40mg daily is the standard. This isn’t optional. Studies show PPIs cut the extra bleeding risk from this combo by 70%. That’s the difference between a 1 in 20 chance and a 1 in 70 chance of bleeding.
- Get tested for H. pylori. If you have this infection, it’s a major ulcer trigger. Eradicating it with antibiotics can reduce your bleeding risk by half.
- Monitor for warning signs. Black, sticky stools. Vomiting that looks like coffee grounds. Unexplained fatigue or dizziness. Sudden abdominal pain. These aren’t normal. Call your doctor immediately.
What If I Can’t Stop Either Drug?
Some people need both. A patient with severe depression and rheumatoid arthritis can’t just quit either. In those cases, the solution isn’t stopping - it’s protecting. A patient on Reddit shared that after switching from naproxen to celecoxib and adding omeprazole, they went 18 months without any GI issues. That’s possible. It’s not luck. It’s strategy. Your doctor should be using tools like the ACG Upper GI Risk Calculator - which factors in age, past ulcers, H. pylori status, and other meds - to decide if you need a PPI. If they haven’t run this assessment, ask them to.What’s Changing in 2025?
Hospitals and clinics are catching on. Since 2019, major systems like Cleveland Clinic and Mayo Clinic have added automated alerts in their electronic records. When a doctor tries to prescribe an SSRI and an NSAID together, the system pops up a warning. Since then, hospital admissions for GI bleeds in dual-therapy patients have dropped by 42%. New research is pushing this further. A 2023 study introduced a genetic test that checks for CYP2C19 mutations - which affect how fast you metabolize both SSRIs and PPIs. If you’re a slow metabolizer, you might need a higher PPI dose. If you’re a fast one, you might need a different drug. A new dual-release pill - ibuprofen with omeprazole built in - is in late-stage trials. If approved, it could make protection automatic. But until then, you need to be your own advocate.Bottom Line: Don’t Assume It’s Safe
This isn’t a hypothetical risk. It’s real, measurable, and preventable. Over 9 million Americans are taking this dangerous combo right now. The FDA and European regulators have added warnings to drug labels since 2019-2020. Yet most patients still aren’t warned. If you’re on an SSRI and taking any NSAID - even occasional ibuprofen - talk to your doctor. Ask: "Am I at risk for bleeding? Should I be on a PPI? Is there a safer painkiller I can use?" This isn’t about fear. It’s about awareness. You don’t need to stop your meds. You just need to protect your stomach.Can I take ibuprofen with an SSRI if I’m young and healthy?
Even if you’re young and healthy, combining ibuprofen with an SSRI still raises your risk of GI bleeding by about 75%. That risk might be low in absolute terms - say, 1 in 100 per year - but it’s still higher than it needs to be. The safest move is to use acetaminophen instead, or take a daily proton pump inhibitor like omeprazole if you must keep both.
Is it safe to take aspirin with an SSRI?
No. Low-dose aspirin also interferes with platelet function, just like NSAIDs. When combined with an SSRI, the risk of GI bleeding increases even more - up to 12-fold in some studies. If you’re on aspirin for heart protection and need an antidepressant, talk to your doctor about alternatives to NSAIDs and always use a PPI.
How long should I take a PPI if I’m on both drugs?
If you’re taking both an SSRI and an NSAID long-term, you should take a PPI daily for as long as you’re on both. Stopping the PPI while continuing the drugs puts you right back at high risk. If you stop the NSAID, you can usually stop the PPI after 4-8 weeks, unless you have a history of ulcers.
Can I switch to a different antidepressant to avoid this risk?
Yes. Bupropion (Wellbutrin) is an antidepressant that doesn’t affect platelets or serotonin reuptake in the same way. It’s a good alternative if you need to avoid GI bleeding risk. Mirtazapine and vortioxetine are also lower-risk options. But switching antidepressants isn’t always easy - talk to your doctor about whether it’s right for your mental health needs.
Do I need a colonoscopy if I’m on both drugs?
No, not unless you have symptoms like bleeding, pain, or weight loss. The risk is for upper GI bleeding - stomach and duodenum - not the colon. An endoscopy (not a colonoscopy) is the test used to check for ulcers or bleeding in the upper tract. Routine screening isn’t recommended unless you’re high-risk or have warning signs.
Are herbal supplements like turmeric or ginger safe with SSRIs and NSAIDs?
Some herbs can make bleeding risk worse. Turmeric, ginger, garlic, ginkgo, and fish oil all have mild blood-thinning effects. If you’re already on an SSRI and NSAID, adding these supplements can push your risk even higher. Always tell your doctor about everything you’re taking - including vitamins and herbal products.

Janet Carnell Lorenz
November 1, 2025 AT 13:28Just found out my doc prescribed me ibuprofen with sertraline and never mentioned this. Holy crap. I’ve been taking it for months for my back. Going to switch to Tylenol tomorrow and ask for omeprazole. So glad I read this.
Michael Kerford
November 3, 2025 AT 07:28People are dying because they didn’t read the fine print. Honestly, if you’re too lazy to look up drug interactions, don’t be surprised when your stomach starts bleeding. This isn’t rocket science.
Geoff Colbourne
November 4, 2025 AT 23:18OMG I knew this was a thing but no one talks about it! My cousin went to the ER last year with black poop and they found a bleeding ulcer-turns out he was on naproxen and Lexapro for 3 years. He didn’t even know NSAIDs could do this. And now he’s on celecoxib and omeprazole but his insurance won’t cover celecoxib so he’s stuck with $300/month bills. This is a scam. Big Pharma doesn’t want you to know about cheap alternatives. They profit off ER visits. I’m telling everyone I know.
Daniel Taibleson
November 5, 2025 AT 06:24This is an exceptionally well-researched and clinically relevant summary. The data on the 75% increased risk is robust, and the recommendation to prioritize celecoxib with PPI co-therapy for high-risk patients aligns with current ACG guidelines. I would only add that the interaction is dose-dependent-daily NSAID use carries significantly higher risk than occasional use. For patients requiring infrequent analgesia, acetaminophen remains the gold standard alternative. Thank you for highlighting this underrecognized public health issue.
Jamie Gassman
November 6, 2025 AT 01:51They don’t want you to know this. The FDA has known since 2019. The AMA’s been silent. Your doctor? They’re paid by pharma reps who push SSRIs and NSAIDs like candy. That ‘automated alert’ in hospitals? It’s a Band-Aid. The real problem is the $1.2 trillion a year GI bleed industry-hospitals, endoscopists, PPI manufacturers-they all profit from your ignorance. I’ve seen the emails. They call it ‘The Silent Profit Pipeline.’ If you’re on both drugs, you’re not just at risk-you’re being exploited. Wake up. This isn’t medicine. It’s a financial model.
Julisa Theodore
November 7, 2025 AT 19:14So… we’re supposed to be scared of ibuprofen now? Like, what’s next? Breathing is dangerous? I mean, if you’re gonna live in fear of every pill you take, you might as well just go live in a cave and eat moss. I take ibuprofen when my knee acts up. I take sertraline when I feel like crying over a commercial. They’re both just… tools. Maybe we should just stop taking meds altogether and pray to the moon? 🌙
Lenard Trevino
November 8, 2025 AT 09:08Okay, so let me get this straight-because I’m on Zoloft and I take Advil every Sunday after my CrossFit session, I’m basically playing Russian roulette with my stomach lining? I’ve been doing this for five years. I’ve never thrown up coffee grounds. I’ve never had black poop. I feel fine. So why are we acting like this is some kind of death sentence? I get the stats, I really do. But humans aren’t just numbers. I’ve got a 32-year-old body, no ulcers, no H. pylori, no warfarin, no steroids. So why am I being told I need a daily proton pump inhibitor like I’m 80 and on dialysis? This feels like medical overkill. I’m not saying ignore it-I’m saying don’t turn every healthy person into a pill-popping zombie because of a 1% risk. I’ll stick with Tylenol on weekends and keep my stomach happy. End of story.
Paul Maxben
November 8, 2025 AT 15:31u/JanetCarnellLorenz u/DanielTaibleson u/JulisaTheodore u/LenardTrevino u/JamieGassman u/GeoffColbourne u/MichaelKerford u/PaulMaxben - y’all are all missing the point. This isn’t about ibuprofen or SSRIs. This is about how medicine stopped being about healing and started being about profit. The fact that you even need a PPI to take two common meds? That’s not medicine. That’s a scam. And the docs who don’t warn you? They’re complicit. I’m not saying stop taking your meds-I’m saying stop trusting the system. Go herbal. Go acupuncture. Go cold showers. Your body’s smarter than your pharmacy. And if you’re still on this, you’re already too late. #WakeUp