Steroid-Induced Diabetes: Causes, Risks, and What You Can Do
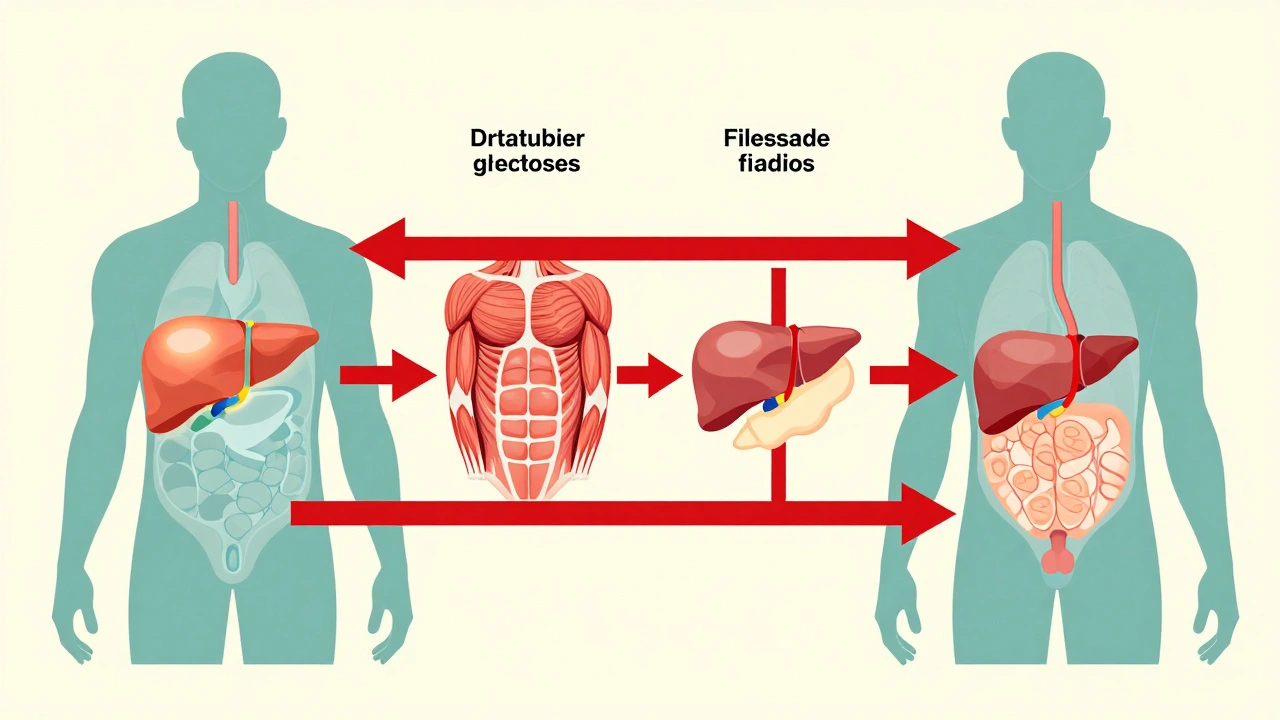
When you take steroid-induced diabetes, a form of high blood sugar triggered by corticosteroid medications. Also known as glucocorticoid-induced hyperglycemia, it isn’t type 1 or type 2 diabetes—but it behaves like one. This isn’t rare. People on long-term prednisone, dexamethasone, or other steroids for asthma, arthritis, or autoimmune conditions often see their blood sugar climb without warning. It happens because these drugs mess with how your body uses insulin. They make your liver dump more glucose into your bloodstream and block insulin from doing its job. The result? High blood sugar—even if you’ve never had diabetes before.
This isn’t just about numbers on a screen. corticosteroids, powerful anti-inflammatory drugs used for decades in medicine are lifesavers for many. But they’re also silent troublemakers for your metabolism. Studies show up to 30% of people on daily steroids for more than a month develop elevated blood sugar. The risk goes up with higher doses, longer use, and if you’re already overweight or have a family history of diabetes. And here’s the catch: many doctors don’t check blood sugar unless symptoms show up—like extreme thirst, frequent urination, or blurry vision. By then, damage might already be starting.
What makes steroid-induced diabetes different is that it often reverses when the steroid is lowered or stopped. But while you’re on it, you still need to manage it. insulin resistance, when your body’s cells stop responding well to insulin is the main driver. That’s why simple fixes like cutting sugar won’t fix it alone. You need a plan. Some people need metformin. Others need insulin injections, even temporarily. And diet matters—not to restrict, but to stabilize. Eating consistent carbs, pairing them with protein and fiber, and avoiding sugary snacks can keep spikes from crashing your system.
You’re not alone in this. Many of the posts below come from people managing this exact problem. One person found their blood sugar spiked after starting prednisone for a flare-up. Another noticed their glucose monitor flashing red after years of normal readings. There’s advice on how to talk to your doctor about testing, how to adjust meals around steroid doses, and why some diabetes meds work better than others in this situation. You’ll also find real stories about balancing necessary treatment with long-term health—because stopping steroids isn’t always an option, but ignoring the sugar spike isn’t either.
What you’ll find here isn’t theory. It’s what works when you’re stuck between needing a steroid and protecting your body from its side effects. No fluff. No guesswork. Just clear, practical steps to understand, monitor, and manage steroid-induced diabetes while staying in control of your health.
Published on Dec 4
9 Comments
Corticosteroids like prednisone can cause sudden high blood sugar, even in people without diabetes. Learn how steroids trigger hyperglycemia, who’s at risk, and how to manage it safely with insulin, monitoring, and timely adjustments.