Pulmonary Embolism: What It Is, How to Spot It, and What to Do
Imagine a blood clot traveling from your leg or arm straight into your lungs – that’s a pulmonary embolism (PE). It can block oxygen flow, cause sudden chest pain, and become life‑threatening in minutes. Knowing the warning signs and the steps doctors take can make all the difference.
Common Symptoms You Shouldn't Ignore
Most people feel a sharp, stabbing pain that gets worse when they breathe deeply or cough. Shortness of breath appears out of nowhere, even if you’re just sitting down. Some experience rapid heartbeat, light‑headedness, or a faint feeling. If the clot is big, you might see a sudden drop in blood pressure, sweating, or a bluish tinge to lips and fingertips.
These symptoms can look like a heart attack or flu, so never assume they’ll pass on their own. When in doubt, call emergency services – every minute counts.
Why Clots Form and Who’s at Risk
Blood clots often start in the deep veins of the legs (deep‑vein thrombosis) after long periods of inactivity – think long flights, bed rest, or recovery from surgery. Factors that raise risk include smoking, obesity, certain cancers, hormonal therapy, and inherited clotting disorders.
If you’ve recently had major surgery, a serious injury, or an extended hospital stay, keep an eye on swelling or pain in your calves. Those are early clues that a clot might be forming.
How Doctors Diagnose a PE
The first step is a quick physical exam and questions about recent travel, surgeries, or family history. Blood tests look for elevated D‑dimer levels, which suggest clot activity. The gold‑standard test is a CT pulmonary angiography – an X‑ray that shows the blood vessels in your lungs.
In some cases, doctors use ultrasound on the legs to find clots at their source or a ventilation/perfusion (V/Q) scan if you can’t have a CT scan. The goal is to confirm the clot fast so treatment can start immediately.
Treatment Options and What to Expect
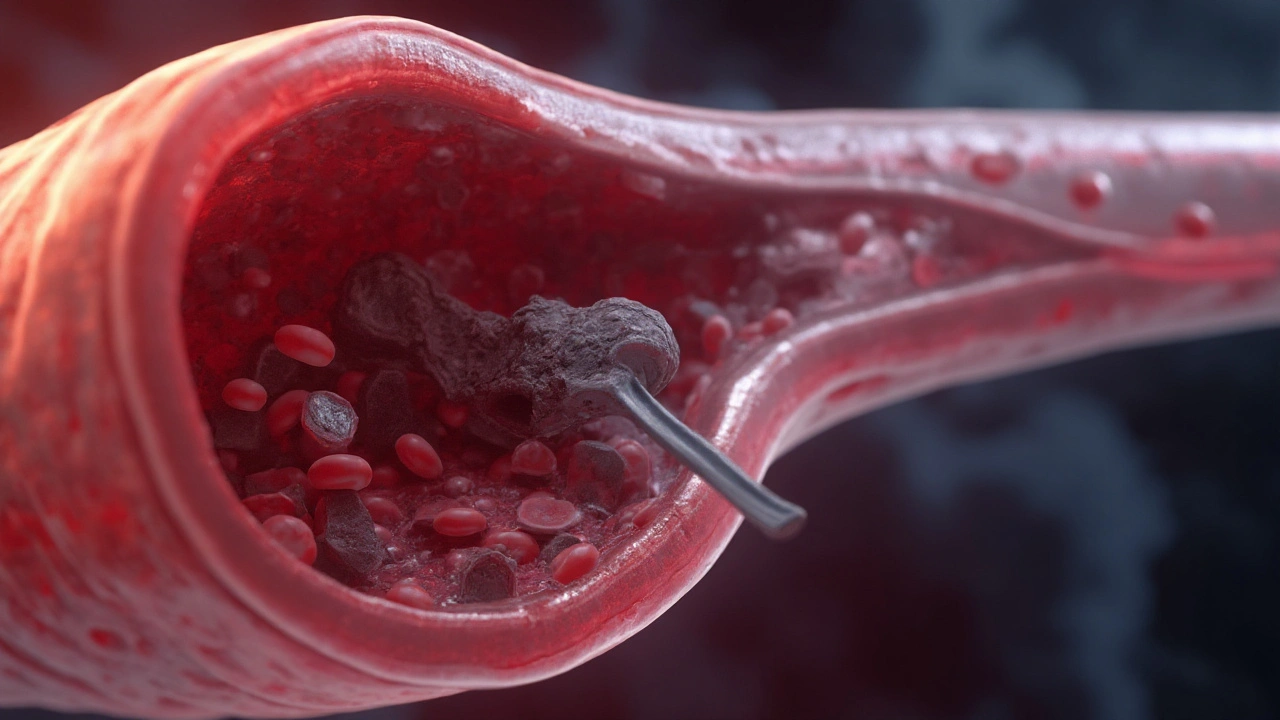
Anticoagulants are the first line of therapy. These blood thinners, like heparin followed by warfarin or newer oral agents (Xarelto, Eliquis), stop new clots from forming and let your body dissolve the existing one. For massive PE that threatens heart function, doctors may give clot‑busting drugs (thrombolytics) or even perform a catheter‑based removal.
Most people stay in the hospital for 2‑5 days to monitor vital signs and adjust medication doses. After discharge, you’ll likely continue an oral anticoagulant for at least three months, sometimes longer if risk factors persist.
Prevention Tips to Keep Clots at Bay
Stay active – walk around every hour during long trips or after surgery. Compression stockings can improve leg blood flow if you’re at higher risk. If your doctor prescribes a preventive anticoagulant before a big operation, take it exactly as directed.
Maintain a healthy weight, quit smoking, and manage chronic conditions like diabetes or high blood pressure. Small lifestyle changes add up to big protection against dangerous clots.
Knowing the signs of pulmonary embolism, understanding why clots happen, and acting quickly can save lives. Keep this guide handy, share it with friends, and don’t hesitate to seek help if something feels off.
Published on Aug 26
18 Comments
Clear, practical guide to embolism: what it is, causes, symptoms, diagnosis, and modern treatments-plus prevention tips, checklists, and FAQs.