Proton Pump Inhibitors: What They Are, How They Work, and What Alternatives Exist
When your stomach makes too much acid, it can cause heartburn, ulcers, or damage to your esophagus. That’s where proton pump inhibitors, a class of medications that block the stomach’s acid-producing pumps. Also known as PPIs, they’re among the most commonly prescribed drugs for acid-related conditions. These drugs don’t just mask symptoms—they stop acid at the source by targeting the proton pumps in stomach cells. That’s why they work better and last longer than antacids or H2 blockers like ranitidine.
But PPIs aren’t magic pills. Long-term use can lead to side effects like nutrient deficiencies, bone loss, or even kidney issues. That’s why many people start looking at alternatives. For example, H2 blockers, like famotidine or ranitidine, reduce acid production but don’t shut it down completely—they’re gentler and often used for short-term relief. Then there’s lifestyle changes, such as avoiding spicy food, eating smaller meals, or not lying down after eating, which can cut acid reflux without any pills at all. And if you’re dealing with an ulcer caused by H. pylori bacteria, antibiotics become the real solution—not just acid blockers.
The posts below cover real comparisons you can actually use. You’ll find how PPIs stack up against other stomach meds, what side effects to watch for, and when it’s time to switch. Some articles dig into how drugs like omeprazole and pantoprazole differ in strength and timing. Others show how people manage reflux without PPIs at all—using diet, timing, or safer alternatives. You’ll also see how chronic acid issues connect to ulcers, inflammation, and even long-term gut health. This isn’t just theory. These are real stories, real data, and real choices people are making every day.
Published on Oct 30
8 Comments
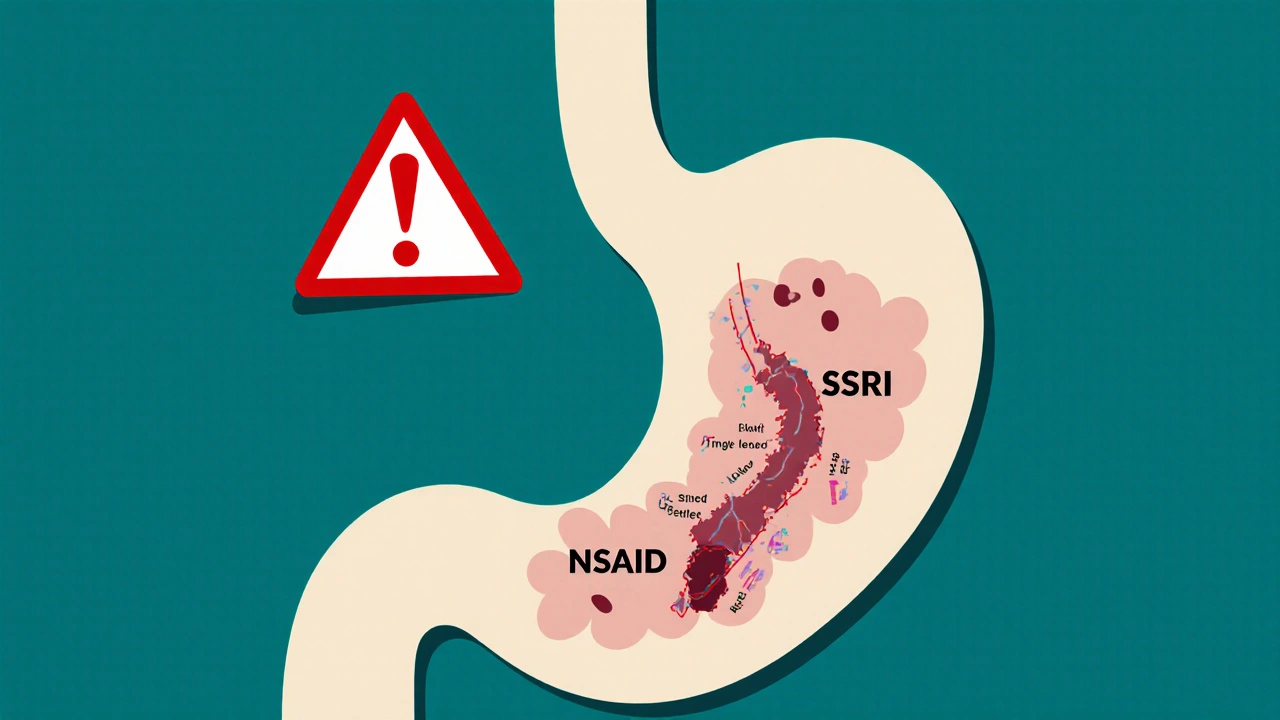
Combining SSRIs and NSAIDs can raise your risk of dangerous GI bleeding by 75%. Learn why this happens, who’s most at risk, and how to protect yourself with safer pain relief and proven prevention strategies.