Pelvic Floor Dysfunction: Causes, Symptoms, and What Actually Helps
When your pelvic floor muscles, a group of muscles that support the bladder, bowel, and uterus. Also known as pelvic floor tension, these muscles can become too tight, too weak, or uncoordinated—leading to a range of uncomfortable and often embarrassing symptoms. It’s not just about leaking urine when you cough. Pelvic floor dysfunction can cause chronic pelvic pain, trouble peeing or pooping, pain during sex, and even lower back pain. And yes, it happens to men, women, and people of all ages—not just after childbirth or in older adults.
Many people think this is just a normal part of aging or having kids, but it’s not. The pelvic floor, a hammock-like network of muscles and connective tissue. Also known as pelvic diaphragm, it works like a suspension system for your internal organs. When it’s not functioning right, everything below your belly button can suffer. Urinary incontinence, the accidental loss of urine. Also known as bladder leakage, is one of the most common signs—but it’s not the only one. You might feel pressure in your pelvis, have trouble starting urination, or feel like you never fully empty your bladder. Some people get constipated because the muscles won’t relax enough to let stool pass. Others feel pain when sitting for long periods or during intercourse.
What causes this? It’s rarely one thing. Pregnancy, surgery, chronic coughing, heavy lifting, and even long-term stress can tighten or weaken these muscles. Sitting all day at a desk? That’s a silent contributor. The body adapts to how you use it—and if you’re always hunched over, your pelvic floor gets ignored. And here’s the kicker: most people don’t know they have it until it’s bad. Doctors often miss it because they’re trained to look for infections or tumors, not muscle dysfunction.
The good news? You don’t need surgery or pills to fix this. Pelvic floor therapy, a specialized form of physical therapy focused on restoring muscle function. Also known as pelvic PT, is the most effective, science-backed approach. A trained therapist uses manual techniques, biofeedback, and exercises to teach your muscles when to relax and when to contract. It’s not Kegels—most people do those wrong and make things worse. Real therapy looks at the whole system: breathing, posture, movement patterns, even your emotional stress response.
What you’ll find in the posts below aren’t generic advice or miracle cures. These are real, practical insights from people who’ve been there and from clinicians who’ve seen the patterns. You’ll see how stress ties into pelvic pain, how certain medications can worsen symptoms, and how simple daily habits—like how you sit or breathe—can make a measurable difference. No fluff. No sales pitches. Just what works, based on real cases and evidence.
Published on Nov 18
9 Comments
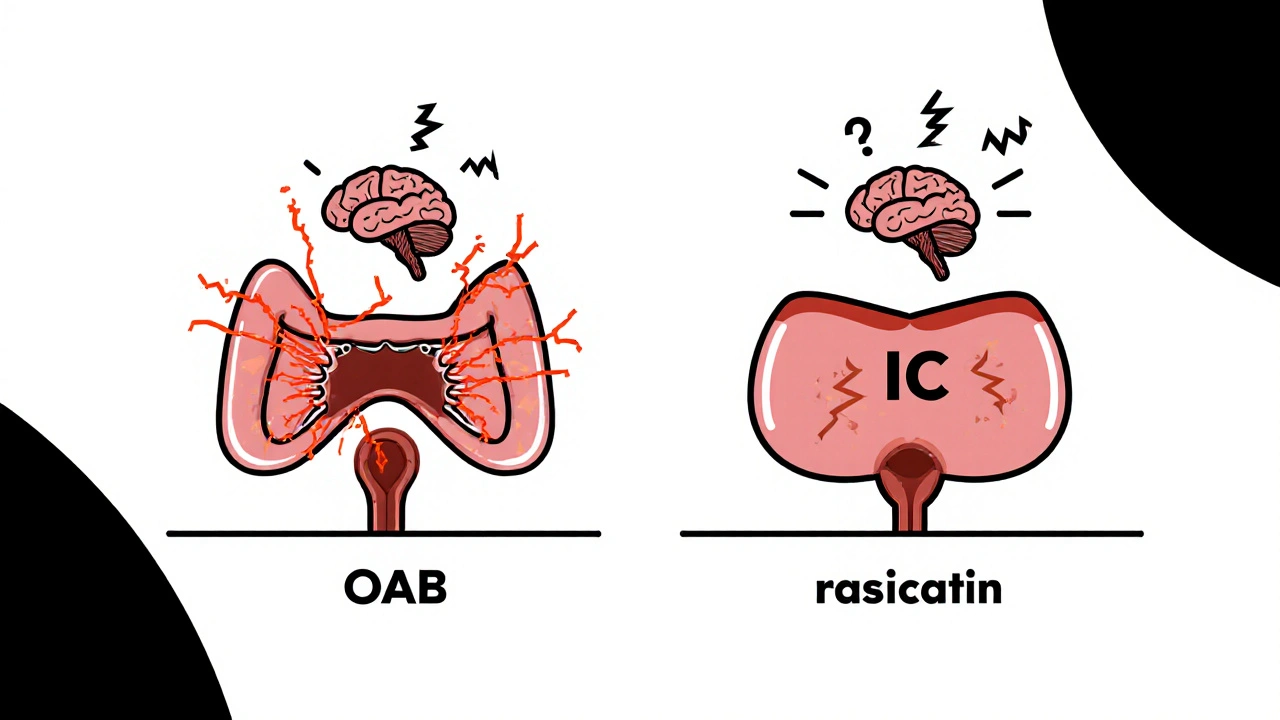
Overactive bladder and interstitial cystitis often occur together, causing urgency, frequency, and pelvic pain. Understanding how they connect helps you get the right treatment and find real relief.