If you’re constantly rushing to the bathroom, feeling sudden urges you can’t ignore, or dealing with pelvic pain that won’t go away, you’re not alone. Many people assume these symptoms are just part of aging or stress-but what if they’re signs of something deeper? Overactive bladder and interstitial cystitis often show up together, and confusing one for the other can delay real relief. The truth is, these two conditions aren’t the same, but they’re closely linked-and understanding how they interact is the first step toward getting proper care.
What Is Overactive Bladder?
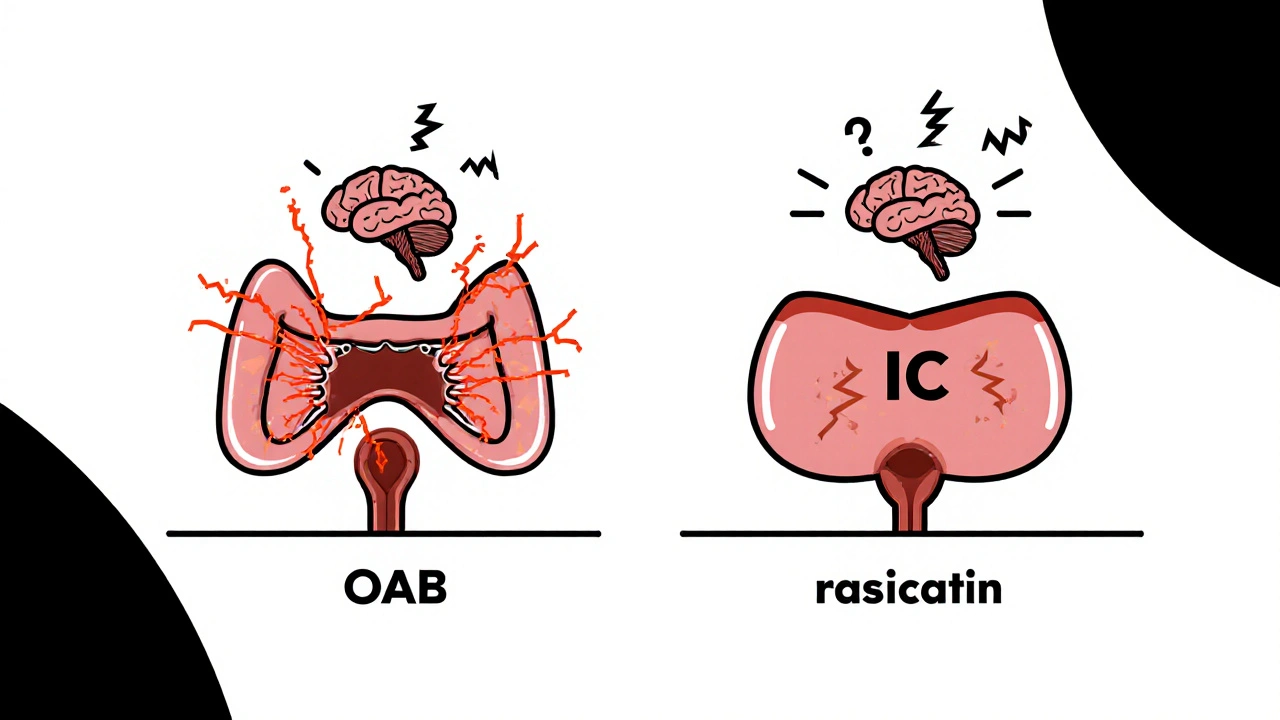
Overactive bladder, or OAB, is a group of urinary symptoms, not a disease. It’s defined by sudden, strong urges to urinate that are hard to control. You might find yourself leaking urine before you reach the toilet, waking up two or more times a night to go, or peeing more than eight times in a day. The bladder muscle (detrusor) contracts unexpectedly, even when it’s not full. This isn’t caused by infection or blockage-it’s a problem with nerve signals between the bladder and brain.
Think of it like a car alarm that goes off for no reason. The car isn’t being stolen, but the alarm doesn’t know that. In OAB, the bladder sends a "full!" signal even when it’s only half full. About 1 in 6 adults in Australia have OAB, and it’s more common in women, especially after menopause. But it’s not normal. And it’s not just inconvenient-it can wreck your sleep, your confidence, and your social life.
What Is Interstitial Cystitis?
Interstitial cystitis, or IC, is a chronic condition that causes bladder pressure, pain, and discomfort. Unlike OAB, IC isn’t just about urgency-it’s about pain. People with IC often describe it as a deep ache, burning, or sharp sensation in the lower abdomen or pelvis. The pain usually gets worse as the bladder fills and improves after urinating. Some feel like their bladder is full even when they just went. Others report pain during sex or in the urethra.
IC is also called bladder pain syndrome (BPS), because that’s what it really is: a pain disorder. The bladder wall becomes inflamed, and in some cases, tiny ulcers or lesions form. The exact cause isn’t known, but researchers think it may involve a damaged protective lining in the bladder, immune system overactivity, or nerve hypersensitivity. It affects about 3 to 8 million people in the U.S. alone, mostly women. Many go years without a diagnosis because doctors mistake it for a UTI.
Why Do These Two Conditions Overlap So Much?
Here’s the key point: up to 80% of people with interstitial cystitis also have symptoms of overactive bladder. And about half of those with OAB report pelvic pain that fits the pattern of IC. That’s not coincidence. It’s because both conditions involve the same system-the bladder and its nerves.
When the bladder lining is damaged (as in IC), it becomes more sensitive. That sensitivity tricks the nerves into sending constant "full" signals to the brain. That’s when urgency and frequency kick in-classic OAB symptoms. So, what starts as pain becomes a cycle: pain → nerve overactivity → frequent urges → more bladder irritation → more pain.
It’s like a broken thermostat. The sensor is faulty, so the heater keeps running even when the room is warm. In the bladder, the nerves are stuck on high alert. Even normal amounts of urine trigger pain and urgency. This overlap is why so many people are misdiagnosed. If you’re treated only for OAB with anticholinergic drugs but still have pain, the real issue-IC-is still there.
How Doctors Tell Them Apart
There’s no single test for either condition. Diagnosis is based on symptoms, ruling out other causes, and sometimes a few key procedures.
For OAB, doctors look for:
- Urgency without infection
- Frequency (more than 8 times a day)
- Nocturia (waking up to pee at night)
- May or may not have incontinence
For IC, they look for:
- Pelvic or bladder pain that worsens with filling
- Pain that improves after urinating
- Urgency and frequency, but with pain as the main complaint
- No infection or other clear cause
Doctors may do a urine test to rule out infection. They might ask you to keep a bladder diary for a few days, noting when you pee, how much, and how you felt. In some cases, a cystoscopy (a tiny camera inserted into the bladder) is used to check for Hunner’s lesions-patches of inflammation that are a telltale sign of IC. But even without visible lesions, IC can still be present.
Here’s the catch: if you have both, you’ll likely need two different treatment approaches. Treating just one won’t fix the whole problem.
Treatment That Addresses Both
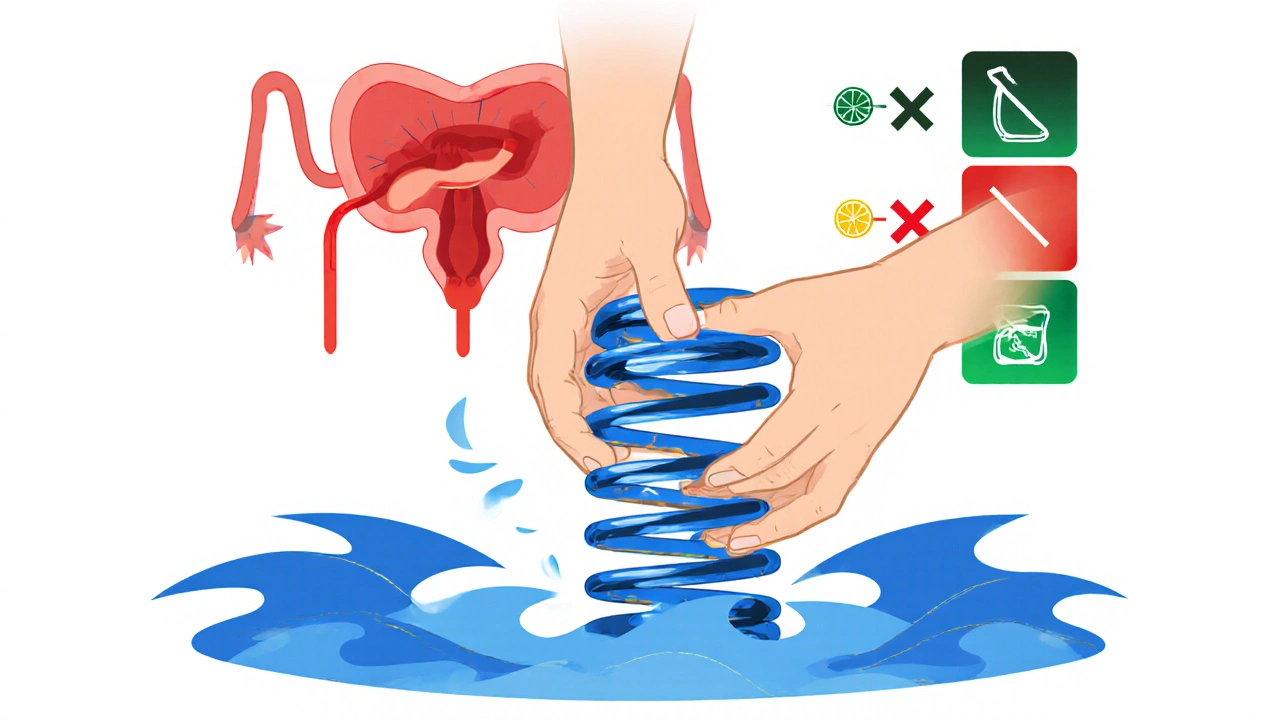
Medications like oxybutynin or tolterodine help with OAB by relaxing the bladder muscle. But they don’t touch the pain of IC-and sometimes make it worse by drying out the bladder lining. For IC, treatments focus on healing the bladder wall and calming the nerves.
Effective strategies for both conditions include:
- Bladder training: Gradually increasing the time between bathroom visits to retrain the bladder. This works best when pain isn’t severe.
- Pelvic floor physical therapy: Many people with IC and OAB have tight, overactive pelvic floor muscles. These muscles can pull on the bladder and worsen both urgency and pain. Therapy helps relax them-often with dramatic results.
- Diet changes: Acidic foods (citrus, tomatoes), caffeine, alcohol, and artificial sweeteners can irritate the bladder. Cutting them out for 2-4 weeks can reveal hidden triggers.
- Oral medications: Pentosan polysulfate sodium (Elmiron) is the only FDA-approved drug for IC. It helps repair the bladder lining. For pain, low-dose amitriptyline or gabapentin can calm nerve signals.
- Bladder instillations: A solution of lidocaine, heparin, or sodium bicarbonate is introduced into the bladder to soothe the lining. Done in a clinic, this can give relief for weeks.
Some people find relief with neuromodulation-devices like InterStim that send gentle electrical pulses to the sacral nerves, helping to reset the bladder’s signaling. It’s not for everyone, but for those who’ve tried everything else, it can be life-changing.
What You Can Do Right Now
If you’re dealing with urgency, frequency, and pain, don’t wait for a diagnosis to start feeling better. Here’s what works for most people:
- Keep a bladder diary for 3 days. Write down what you drink, when you pee, how much, and your pain level (0-10). This helps your doctor see patterns.
- Eliminate bladder irritants for 4 weeks: coffee, tea, soda, alcohol, citrus, spicy food, artificial sweeteners.
- Try pelvic floor relaxation exercises. Sit quietly, breathe deeply, and imagine your pelvic floor muscles softening-like a flower opening. Do this 5 minutes twice a day.
- Drink water slowly throughout the day. Chugging fluids overwhelms the bladder. Aim for 6-8 small glasses, not 2 big ones.
- See a pelvic health physiotherapist. They’re trained to spot muscle tension that’s causing or worsening symptoms.
Many people feel better within weeks just by making these changes. You don’t need to live with this pain.
When to Seek Help
If you’ve had symptoms for more than 6 weeks, or if they’re getting worse, it’s time to see a specialist-not your GP. Look for a urogynecologist, urologist with pelvic pain experience, or a pelvic floor physiotherapist. Don’t settle for "it’s just aging" or "drink less water." Those answers don’t fix the problem.
There’s no cure for IC or OAB, but there are dozens of ways to manage them. The key is treating both the urgency and the pain, not just one. The sooner you connect the dots between your symptoms, the sooner you’ll find relief.
Can overactive bladder turn into interstitial cystitis?
No, OAB doesn’t "turn into" IC. But the two often occur together because they share nerve pathways. If you have OAB and start developing pelvic pain, it’s likely you’re also developing IC-or you already had it and didn’t realize. The pain changes the way your bladder behaves, making OAB symptoms worse.
Is interstitial cystitis the same as a UTI?
No. A urinary tract infection (UTI) is caused by bacteria and usually comes with cloudy or foul-smelling urine, fever, or burning during urination. IC has no infection. Antibiotics won’t help. If your symptoms come and go without infection, it’s likely IC, not a UTI.
Can stress make overactive bladder and IC worse?
Yes. Stress doesn’t cause IC or OAB, but it amplifies them. When you’re stressed, your nervous system goes into high alert. That makes bladder nerves more sensitive. Many people notice flare-ups during work deadlines, family conflicts, or sleep loss. Managing stress with breathing, yoga, or therapy can reduce symptom severity.
Are there foods that help with interstitial cystitis?
Yes. A bladder-friendly diet focuses on non-irritating foods: bananas, pears, green beans, squash, oats, rice, and lean proteins. Drinking water with a pinch of baking soda can help neutralize acidity. Some people benefit from cranberry supplements-but only if they don’t trigger pain. Everyone’s triggers are different, so track what works for you.
How long does it take to see improvement with pelvic floor therapy?
Most people notice changes in 4 to 8 weeks with weekly sessions. Some feel better after just a few visits. It’s not about strengthening muscles-it’s about learning to relax them. If you’ve been told to do Kegels and it made things worse, you likely have tight muscles, not weak ones. Pelvic floor therapy teaches you how to release them.
Next Steps
Start with a bladder diary and eliminate irritants. That’s step one. Then find a pelvic health physiotherapist. They’re often overlooked, but they’re one of the most effective treatments for both conditions. If pain persists, ask your doctor about a referral to a urologist who specializes in chronic pelvic pain. Don’t accept vague answers. You deserve to feel better.

Jenny Lee
November 19, 2025 AT 22:35Just cut out coffee and soda for a week. I did. Life changed.
Brandon Lowi
November 20, 2025 AT 21:58Let me tell you something, America-this isn’t just a bladder issue, it’s a SYSTEMIC FAILURE of modern medicine! They treat symptoms like they’re glitches in a software update, not signs of a body screaming for help! The bladder? It’s not broken-it’s betrayed! The pharmaceutical giants don’t want you to know that pelvic floor therapy costs $0 and heals everything, but they’ll sell you $500 pills that dry you out like a desert wind! And don’t get me started on how they ignore the nerve overload-your bladder’s not malfunctioning, it’s been hijacked by stress, sugar, and corporate greed! We need a revolution-not more anticholinergics, but accountability! Wake up, people!
Joshua Casella
November 21, 2025 AT 18:40I’ve been dealing with this for years. The bladder diary was the first thing that actually helped. I didn’t realize how much soda I was drinking until I wrote it down. Then I cut out the artificial sweeteners and-boom-pain dropped by 70%. Pelvic floor PT was the real game-changer though. I thought I just needed to squeeze harder, turns out I needed to stop squeezing at all. No hype. Just results. If you’re reading this and stuck, start with the diary. It’s free, it’s simple, and it gives you data-not guesswork.
Richard Couron
November 22, 2025 AT 20:59They don’t want you to know this but IC and OAB are linked to 5G radiation and government microchips implanted during flu shots-ask anyone who’s been to a urologist after 2015 and they’ll tell you the same thing. The FDA approved Elmiron because it’s profitable, not because it works. My cousin in Ohio had his bladder lining peeled back by a doctor who said it was 'chronic inflammation'-turns out he was injected with a tracking dye that turned his nerves into screaming wires. The real cure? Raw garlic and grounding barefoot in your backyard at 3am. No one will tell you that because they’re paid off by Big Pharma and the NSA. I’m not crazy-I’m just the only one who’s connected the dots.
Alex Boozan
November 22, 2025 AT 23:58From a urodynamic standpoint, the neurogenic dysregulation of the sacral micturition reflex arc is the primary pathophysiological nexus between OAB and IC. The afferent C-fiber hypersensitivity, coupled with mast cell degranulation and proteoglycan layer degradation, creates a feed-forward loop of visceral hyperalgesia and detrusor overactivity. Standard antimuscarinics exacerbate mucosal dryness and reduce urothelial barrier integrity, thus accelerating the inflammatory cascade. A multimodal approach targeting neuroinflammation, pelvic floor myofascial tone, and epithelial repair via pentosan polysulfate is the only evidence-based paradigm that addresses the core mechanisms. If you're not treating the neuro-immune axis, you're just palliating.
mithun mohanta
November 23, 2025 AT 09:08Ohhhhh so now we’re all supposed to be experts on bladder nerves? I mean, I read the article and I’m just… wow. I didn’t know my bladder had a personality. But seriously, this is why I don’t trust Western medicine-they give you a 10-page PDF and expect you to solve your pain like it’s a crossword puzzle. Meanwhile, in India, we just drink warm turmeric milk, sit in silence, and let the universe realign your chi. Why are we overcomplicating this? The answer is simple: your bladder is mad because you’re stressed, you eat too much sugar, and you sit on your phone all day. Do less. Breathe. And stop Googling symptoms at 2am.
Ram tech
November 24, 2025 AT 04:37why do people even write this long stuff. just go to the doc. if they say its normal then its normal. i had the same thing and i just drank less water and it went away. no therapy no diet no nothing. stop making it a big deal
Timothy Uchechukwu
November 25, 2025 AT 07:28Look I live in Nigeria and we don't have fancy urologists here but we know one thing if your bladder hurts you drink more water not less. The western world is so obsessed with pills and diets they forget the body heals itself if you stop poisoning it. Stop drinking soda. Stop eating processed junk. Drink clean water. Walk. Sleep. That's it. You don't need a diary or a therapist. You need common sense and a little discipline. This whole thing is overmedicalized nonsense.
Ancel Fortuin
November 25, 2025 AT 21:47Oh so now the solution is to drink baking soda water and do pelvic floor yoga? Sure. Next they’ll tell us to wear copper bracelets and meditate under a full moon. I’ve been to three specialists. Two said it’s ‘stress’. One said ‘it’s all in your head’. The fourth one? He handed me a pamphlet and charged me $400. Meanwhile, my insurance won’t cover the one thing that actually helps-pelvic PT-because it’s ‘experimental’. So yeah, let’s all just chill and do breathing exercises while Big Pharma sells us more pills that make us drier than a desert. Brilliant. Just brilliant.