Overactive Bladder: Causes, Treatments, and What Really Works
When your bladder sends signals you can’t ignore—sudden urges, frequent trips to the bathroom, even leaks—you’re not just being impatient. You’re dealing with overactive bladder, a condition where the bladder muscle contracts involuntarily, even when it’s not full. Also known as urge incontinence, it’s not a normal part of aging, and it’s not something you have to live with quietly. It’s a real medical issue, not a nuisance. And while it’s often linked to older adults, it can hit anyone—even people in their 30s and 40s.
What causes it? Sometimes, it’s nerve damage from diabetes or surgery. Other times, it’s simply the bladder muscle getting too sensitive or overactive on its own. Caffeine, alcohol, and even dehydration can make it worse. And here’s the catch: many people assume it’s just a urinary tract infection, but if antibiotics don’t help, it’s likely overactive bladder, a functional disorder of the lower urinary tract. It’s not caused by infection, but it can be worsened by habits like holding it too long or drinking too much before bed.
There are two main paths to managing it: pelvic floor exercises, targeted muscle training that strengthens the support system around the bladder, and anticholinergics, medications that calm the bladder muscle and reduce sudden contractions. Pelvic floor rehab isn’t glamorous, but studies show it works as well as pills for many people—and without the dry mouth or constipation side effects. Anticholinergics like oxybutynin or tolterodine help, but they’re not magic. They work best when paired with behavioral changes: timed bathroom trips, cutting back on bladder irritants, and keeping a diary to spot triggers.
What you won’t find in most doctor’s offices? A clear plan that combines both. Too often, patients are handed a script and told to wait. But real progress comes from linking medication with daily habits. If you’re tired of planning your day around bathrooms, you’re not alone. The good news? You don’t need surgery or expensive devices to take back control. Small, consistent changes—like drinking water evenly through the day instead of chugging it at night—can make a bigger difference than you think.
Below, you’ll find real-world guides on how these treatments actually work, what side effects to watch for, and how to spot when a medication isn’t helping—or making things worse. You’ll see how diuretics can accidentally make bladder urgency worse, how stress affects bladder control, and what alternatives exist when standard drugs fail. This isn’t theory. These are the tools and insights people are using right now to live without constant worry.
Published on Nov 18
9 Comments
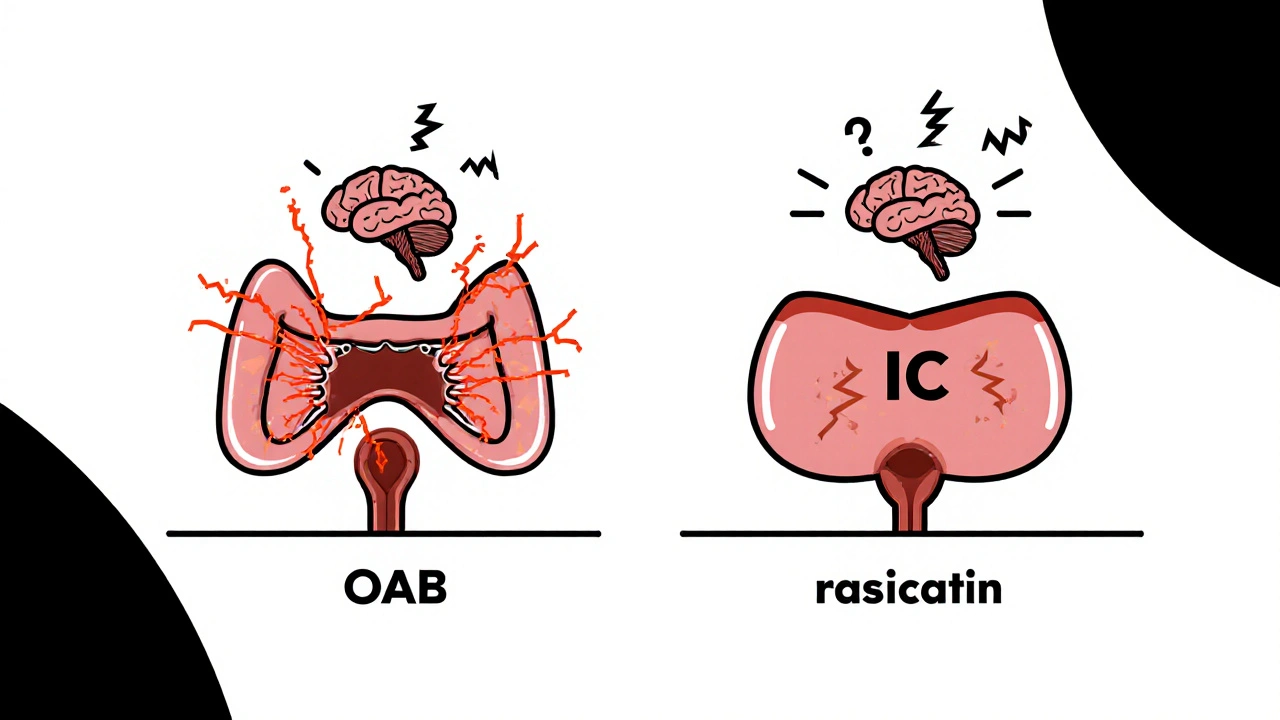
Overactive bladder and interstitial cystitis often occur together, causing urgency, frequency, and pelvic pain. Understanding how they connect helps you get the right treatment and find real relief.