Interstitial Cystitis: Causes, Symptoms, and Management Strategies
When your bladder hurts even when it’s not full, and every trip to the bathroom feels like a battle, you might be dealing with interstitial cystitis, a chronic condition causing bladder pressure, pain, and sometimes pelvic pain. Also known as bladder pain syndrome, it’s not an infection, not stress, and not in your head—it’s a real, poorly understood problem affecting up to 12 million people in the U.S. alone. Unlike a UTI, antibiotics won’t fix it. The lining of the bladder becomes irritated, sometimes with tiny ulcers, and nerves send pain signals even when there’s no infection present.
People with interstitial cystitis often report urinary urgency that comes out of nowhere, waking them up multiple times at night. The pain can range from a dull ache to sharp stabs, and it usually gets worse as the bladder fills. Many also experience pelvic floor dysfunction, where muscles around the bladder and pelvis tighten up painfully, making urination harder and adding to the discomfort. These aren’t just symptoms—they’re interconnected parts of a system that’s gone off track.
What triggers it? No single cause is proven, but food sensitivities (like coffee, alcohol, citrus), stress, and nerve hypersensitivity play big roles. Some studies link it to autoimmune responses or defects in the bladder’s protective lining. Diagnosis is tricky because it’s one of exclusion—you rule out infections, cancer, and other conditions first. A cystoscopy or bladder biopsy might be needed, but many patients go years without a clear answer.
There’s no magic cure, but real relief is possible. Some find success with dietary changes—cutting out acidic or spicy foods. Others benefit from physical therapy targeting the pelvic floor. Medications like pentosan polysulfate sodium can help repair the bladder lining. And while some doctors still push bladder instillations or nerve stimulators, many patients report better results from simple, consistent habits: timed voiding, gentle stretching, and avoiding prolonged sitting.
What you’ll find in the posts below aren’t generic advice or placebo-driven tips. These are real-world insights from people who’ve lived with this condition, backed by clinical data and practical strategies. You’ll see how certain medications interact with bladder health, why hydration matters more than you think, and how inflammation in other parts of the body can make IC worse. No fluff. No hype. Just what works—and what doesn’t—for managing this stubborn condition.
Published on Nov 18
9 Comments
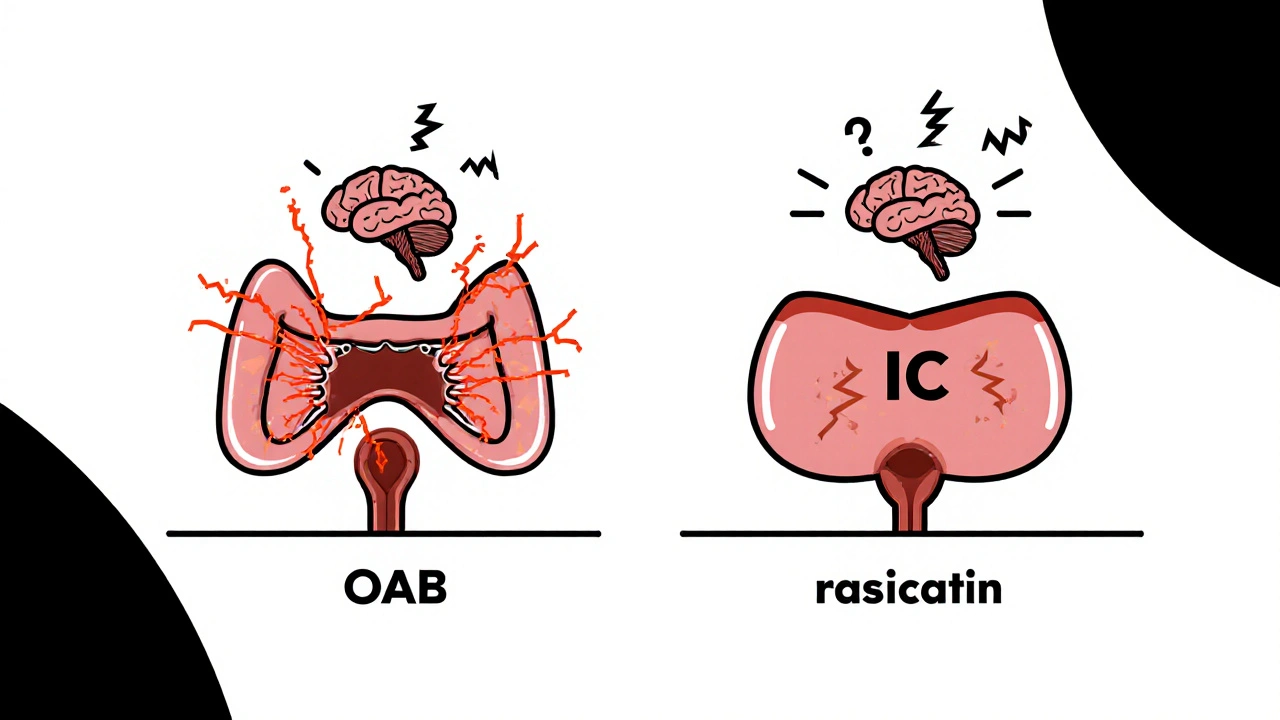
Overactive bladder and interstitial cystitis often occur together, causing urgency, frequency, and pelvic pain. Understanding how they connect helps you get the right treatment and find real relief.