Hypertension Guidelines: What You Need to Know About Blood Pressure Management
When it comes to hypertension guidelines, official recommendations that define how to diagnose, treat, and manage high blood pressure. Also known as blood pressure management protocols, these guidelines are updated regularly based on large clinical studies and real-world outcomes. If you or someone you know has high blood pressure, following the right guidelines isn’t just about taking a pill—it’s about knowing when to act, what to avoid, and how to track progress without guesswork.
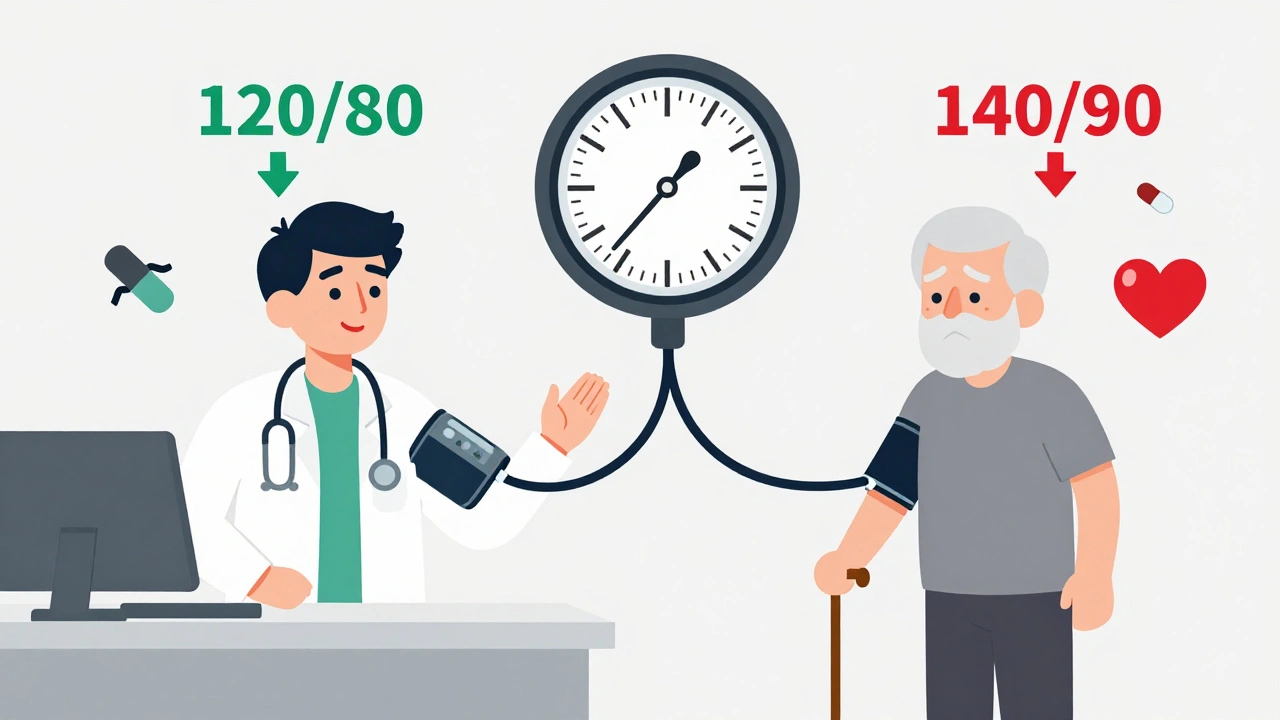
These guidelines don’t just tell you to lower your number—they show you blood pressure targets, specific systolic and diastolic readings that reduce stroke and heart attack risk. For most adults, the goal is under 130/80 mm Hg, but for older patients or those with kidney disease, the numbers might be adjusted. What’s surprising? Many people don’t realize that even small, consistent drops in pressure—like going from 150/95 to 135/85—can cut your risk of complications by nearly half. And it’s not just medication. lifestyle changes for hypertension, diet, exercise, salt reduction, and weight management are the foundation of every major guideline. In fact, studies show that losing just 5% of your body weight can drop systolic pressure by 5 to 20 points. No drug needed.
But here’s the catch: guidelines also warn against overtreating. Some people panic and take too many pills, leading to dizziness, falls, or kidney stress. That’s why antihypertensive drugs, medications like ACE inhibitors, calcium channel blockers, and thiazide diuretics are chosen carefully based on age, race, and other health conditions. For example, if you’re African American with high blood pressure, guidelines often recommend starting with a calcium channel blocker or diuretic—not an ACE inhibitor—because they work better in that group. And if you’re on multiple meds, the guidelines help you avoid dangerous combos, like mixing NSAIDs with diuretics, which can spike kidney risk.
You’ll also find that hypertension guidelines tie into other conditions you might not expect. Take kidney disease—high blood pressure is both a cause and a symptom. Or sleep apnea—untreated, it can make your pressure skyrocket even if you’re on meds. That’s why the best guidelines don’t just focus on the number on the monitor. They ask: Are you sleeping well? Are you eating too much salt? Are you checking your pressure at home, or just at the doctor’s office? The posts below cover these exact connections—from how diuretics affect hydration, to why turmeric can interfere with blood pressure meds, to how pharmacy substitution laws might swap your brand drug for a generic that doesn’t work the same way for you.
These aren’t theoretical rules. They’re tools used by doctors, pharmacists, and patients every day to avoid heart attacks, strokes, and hospital stays. And the more you understand them, the more control you have. Below, you’ll find real, practical advice from people who’ve lived with high blood pressure, tweaked their meds, tracked their numbers, and learned what actually works—without the fluff or fear.
Published on Dec 1
14 Comments
Should your blood pressure target be 120/80 or individualized? In 2025, guidelines clash over whether lower is always better. Learn who benefits from aggressive targets and who should aim higher for safety and quality of life.