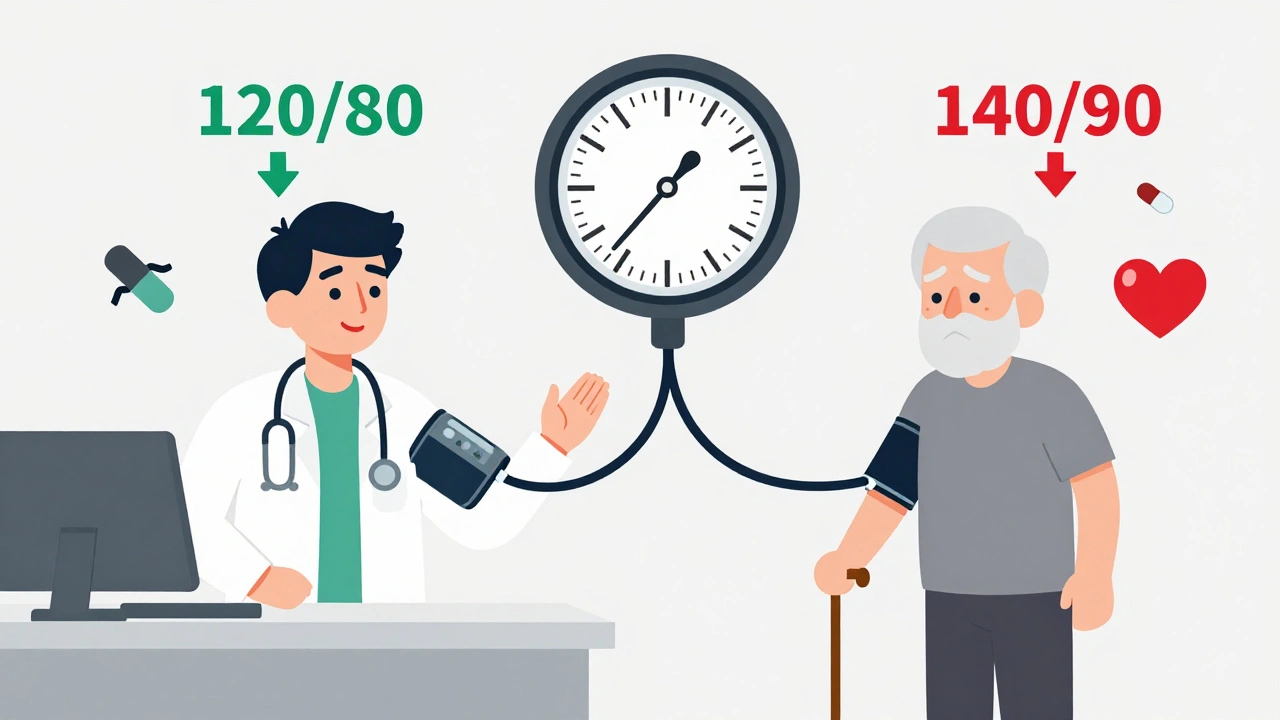
When you walk into a doctor’s office and hear your blood pressure reading - say, 138/86 - what does that number really mean for your heart? Should you be rushing to start medication? Or is it fine to wait and focus on lifestyle changes? The answer isn’t the same for everyone. In 2025, doctors are still arguing over whether everyone with high blood pressure should aim for 120/80, or if personal health history should guide the target.
Why 120/80 Became the New Benchmark
The push for a 120/80 mm Hg target started with the SPRINT trial in 2015. That study followed nearly 9,400 adults with high blood pressure but no diabetes or stroke history. Half were told to get their systolic pressure below 140. The other half were pushed hard to get below 120. After about four years, the group targeting 120 had 25% fewer heart attacks, strokes, and heart failure events. Their risk of dying dropped by 27%. It was a big deal. The American Heart Association and American College of Cardiology responded in 2017 by lowering the official definition of high blood pressure from 140/90 to 130/80. By 2025, they’re now urging most adults to aim for under 120 if it’s safe.But here’s the catch: SPRINT didn’t include older adults with multiple health problems, people with diabetes, or those at high risk of falling. Most real-world patients aren’t like the SPRINT group. So when guidelines say “everyone should aim for 120/80,” it doesn’t always fit.
The Other Side: Why 140/90 Still Makes Sense
The American Academy of Family Physicians (AAFP) took a different look at the same data. They found that while lower targets reduced heart events slightly, they also increased side effects - dizziness, fainting, kidney issues, and low blood pressure that made people feel awful. For every 33 people pushed to hit below 120, one had a serious adverse event like a fall or hospital visit. That’s not a small trade-off.AAFP’s 2022 review concluded: for most people, especially older adults or those with other health issues, 140/90 is just as good at preventing death and heart attacks - and much safer. They argue that the goal of treatment isn’t just to lower numbers. It’s to help people live longer without being sick from their meds.
Think about it this way: if you’re 78, live alone, take five other pills, and already feel lightheaded when you stand up, pushing your systolic pressure to 118 might not improve your life. It might just make you more likely to fall and break your hip.
Where the World Stands in 2025
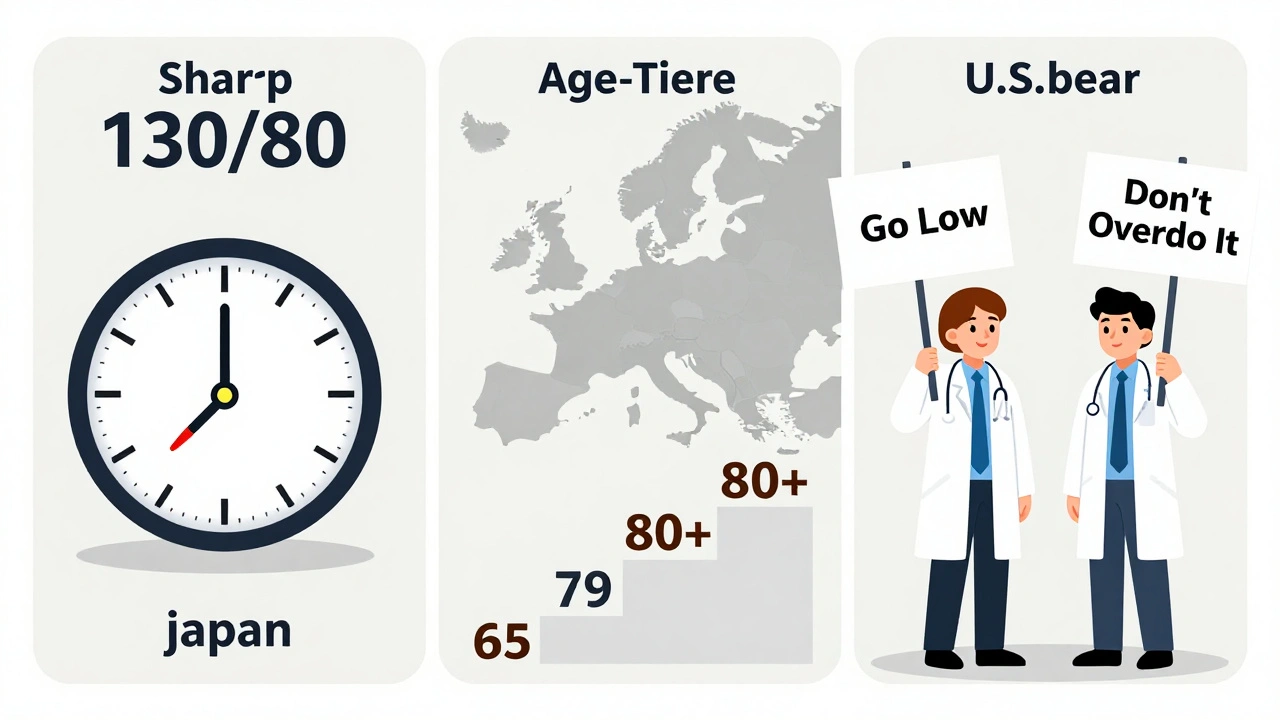
Guidelines aren’t just different in the U.S. - they’re worlds apart globally.Japan’s 2025 guidelines, published in Nature, now say: everyone, no matter their age or health, should aim for under 130/80. They’re betting that better monitoring and faster adjustments can prevent harm. Their doctors are trained to watch for drops in kidney function or potassium spikes, and they adjust meds quickly.
In Europe, the approach is more age-based. Under 65? Target 120-129/70-79. 65-79? Up to 139 systolic. 80+? 140-150 is acceptable. They accept that older bodies handle pressure differently.
The U.S. is stuck in the middle. The AHA/ACC says “go low if you can.” The AAFP says “don’t overdo it.” And many family doctors are confused. A 2024 Medscape survey showed only 41% of family physicians support targets below 130/80 - while 62% of cardiologists do. That gap isn’t just about knowledge. It’s about who you treat every day.
Who Should Aim for 120/80?
Not everyone needs to chase 120/80. But some people benefit a lot.- If you’re under 65 and have diabetes, chronic kidney disease, or a 10-year heart risk over 7.5% (calculated using the PREVENT tool), aiming for 120/80 is strongly recommended.
- If you’ve already had a heart attack, stroke, or heart failure, lower targets cut your risk of another event.
- If you’re otherwise healthy, under 60, and your pressure is 130-139/80-89, lifestyle changes alone may be enough - at least for now.
For these people, the benefits outweigh the risks. Medication can help. But even then, it’s not about hitting 120 at all costs. It’s about getting close - and staying steady.
Who Should Keep It at 140/90?
If you’re over 75, especially with frailty, memory issues, or multiple medications, 140/90 is often the smarter goal.- Older adults are more likely to drop too low and faint, leading to falls and fractures.
- Many seniors already have reduced kidney function - aggressive BP lowering can make that worse.
- Adding more pills increases the chance of bad drug interactions.
One study found that in people over 80, targeting below 140 didn’t reduce death rates - but it did increase hospital visits for low blood pressure. That’s not progress. That’s harm.
Also, if your blood pressure is controlled at 135/85 and you feel fine, don’t rush to add a third pill just to hit 120. You’re not saving years - you’re adding side effects.

How to Decide What’s Right for You
This isn’t a one-size-fits-all situation. Your doctor shouldn’t just give you a number and walk away. Here’s how to have a real conversation:- Ask: “What’s my 10-year risk for heart disease?” Use the PREVENT calculator - most clinics now have it built into their systems.
- Ask: “What are the side effects I’m likely to get if we lower this further?”
- Ask: “How many pills will I need? Will I feel worse before I feel better?”
- Ask: “What’s the plan if I get dizzy or weak?”
Good doctors don’t push numbers. They help you weigh trade-offs. If you’re healthy and active, going lower might be worth it. If you’re tired, taking eight pills, and scared of falling, staying at 135/85 might be the best outcome.
What’s Changing in 2025?
The debate isn’t over. The NIH just launched SPRINT-2 - a new trial that includes older adults, people with diabetes, and those at risk of falls. This will give us real answers for the people most affected by these guidelines.Also, tech is helping. Smart home monitors, AI-powered apps that track symptoms alongside BP, and wearable devices that flag sudden drops are making it safer to aim lower. If you can catch dizziness or low pressure early, you can adjust meds before you end up in the ER.
And the big shift? Shared decision-making. No more “take this pill.” Now it’s “Here’s what we know. Here’s what it might cost you. What matters most to you?”
The Bottom Line
There’s no magic number that fits everyone. 120/80 is ideal for younger, healthier people with high heart risk. But for many - especially seniors or those with complex health issues - 140/90 is safer, just as effective, and better for quality of life.Don’t let a number define your health. Let your life - your energy, your balance, your ability to enjoy your days - guide the goal. Blood pressure isn’t just a reading. It’s a tool. And like any tool, it’s only useful if it helps you live better, not just live longer.

James Kerr
December 2, 2025 AT 09:35My grandpa’s BP’s been 135/85 for 10 years and he still hikes every weekend. If it ain’t broke, don’t fix it. 🤷♂️
Gavin Boyne
December 2, 2025 AT 17:03Oh wow, so now we’re treating hypertension like a yoga pose? ‘Find your inner 120’? The SPRINT trial was conducted on people who didn’t have a single real-world problem - no meds, no dementia, no grandkids to babysit. Meanwhile, my 79-year-old neighbor got hospitalized because they pushed her BP too low and she took a header into her coffee table. The real villain here isn’t hypertension - it’s algorithm-driven medicine that treats humans like spreadsheet cells.
Rashi Taliyan
December 4, 2025 AT 07:44As someone whose mother had a stroke at 72 after being pressured to drop her BP to 118, I’m screaming into the void here. They didn’t ask her if she wanted to be dizzy all day. They didn’t ask if she wanted to stop gardening. They just wrote a number on a chart like it was a grocery list. This isn’t medicine - it’s performance art for doctors who think numbers are more real than people.
Archie singh
December 5, 2025 AT 13:28120/80 is the gold standard because it’s the only number that matters in peer-reviewed journals and pharma-funded guidelines. The AAFP? A bunch of Luddites clinging to 1990s thinking. If you’re over 65 and still walking without a cane, you’re not frail - you’re just lazy. Lower your BP or get off the pot. This isn’t a democracy - it’s physiology. You don’t get to vote on arterial pressure.
shalini vaishnav
December 6, 2025 AT 09:39India’s been treating BP at 140/90 for decades and our people live longer than Americans. Why? Because we don’t poison our elders with 7 different pills just to hit a number made by rich white men in white coats. This 120/80 nonsense is Western arrogance disguised as science. We know our bodies. We know our elders. Stop exporting your medical colonialism.
Charles Moore
December 8, 2025 AT 09:35There’s room here for both sides. The data shows lower targets help high-risk folks - no argument. But for seniors with multiple meds, dizziness, or a history of falls, pushing lower can be dangerous. The key isn’t which guideline wins - it’s whether the doctor listens. I’ve seen patients thrive at 130/80 and crash at 115/70. The goal isn’t the number - it’s the person behind it. Ask them what matters. Are they worried about living longer? Or living well?
sagar bhute
December 9, 2025 AT 19:40SPRINT was a scam. They excluded anyone who actually mattered - the old, the diabetic, the frail. Then they marketed the results like it was a miracle cure. Big Pharma loved it. More pills. More visits. More profits. The real study should’ve been: ‘How many elderly people get hospitalized because their doctor tried to turn them into a lab rat?’ Spoiler: it’s not a small number. This isn’t medicine. It’s capitalism in scrubs.
bobby chandra
December 10, 2025 AT 00:02Let’s get real - no one gives a damn about 120 vs 140 until they’re the one dizzying in the shower. I’m a cardiologist and I tell my patients: if you’re feeling like a zombie on three pills, we’re not winning. The number on the screen doesn’t care if you can still hug your grandkids. If your BP’s stable, you’re active, and you’re not falling over - chill. Medicine isn’t about perfection. It’s about peace.
Kara Bysterbusch
December 10, 2025 AT 23:04The paradigm shift here is not statistical - it’s philosophical. We’ve moved from a biomedical model that treats blood pressure as a disease to be eradicated, to a person-centered model that treats it as a variable within the ecosystem of lived experience. The goal is not normalization, but flourishing. When we reduce human vitality to a single numeric metric, we risk pathologizing aging itself. This is not merely a clinical debate - it is an ethical reckoning.
Cindy Lopez
December 11, 2025 AT 08:25Wow. So much text. Can we just say ‘it depends’ and move on?
Rashmin Patel
December 11, 2025 AT 15:48My aunt in Delhi has BP 138/88, takes one pill, walks 5km daily, cooks for 6 people, and dances at weddings. Her doctor says ‘perfect.’ Meanwhile, my cousin in Chicago is on 4 meds, feels like a ghost, and can’t climb stairs because his BP was pushed to 118/75. Who’s winning? The number? Or the person? Tech helps, yes - but only if it serves the human, not the algorithm. Let’s stop treating elders like broken machines and start treating them like people who’ve earned the right to feel okay.
vinoth kumar
December 13, 2025 AT 02:23I’m a nurse in Mumbai and I’ve seen both sides. We used to push everyone to 120. Then we started losing patients to falls and kidney crashes. Now we ask: ‘What do you want your life to look like?’ Some say ‘I want to live to 90.’ Others say ‘I want to play with my grandkids without passing out.’ We tailor from there. No one-size-fits-all. No drama. Just care. Maybe the US needs to learn from places like India - where family and function matter more than numbers.
Gene Linetsky
December 13, 2025 AT 06:06120/80 is a corporate health scam. The real target is your wallet. Every time you lower a BP number, a drug company makes millions. The SPRINT trial? Funded by the same people who sell the pills. They don’t care if you fall - they care if you refill. The government’s just their puppet. Wake up. Your BP isn’t broken. Your system is.
Ignacio Pacheco
December 14, 2025 AT 05:05So the AHA says ‘go low,’ the AAFP says ‘chill,’ and the patients are just sitting there like, ‘Can someone please tell me what to do without making me feel like a statistic?’ Meanwhile, the real innovation isn’t in the guidelines - it’s in the apps that let you log your dizziness, sleep, and BP together. Maybe the answer isn’t more rules - it’s better feedback loops. Let the person’s daily life be the guide, not a 2015 trial from a lab full of healthy 55-year-olds.