Hyperglycemia: What It Is, How It Affects You, and What You Can Do
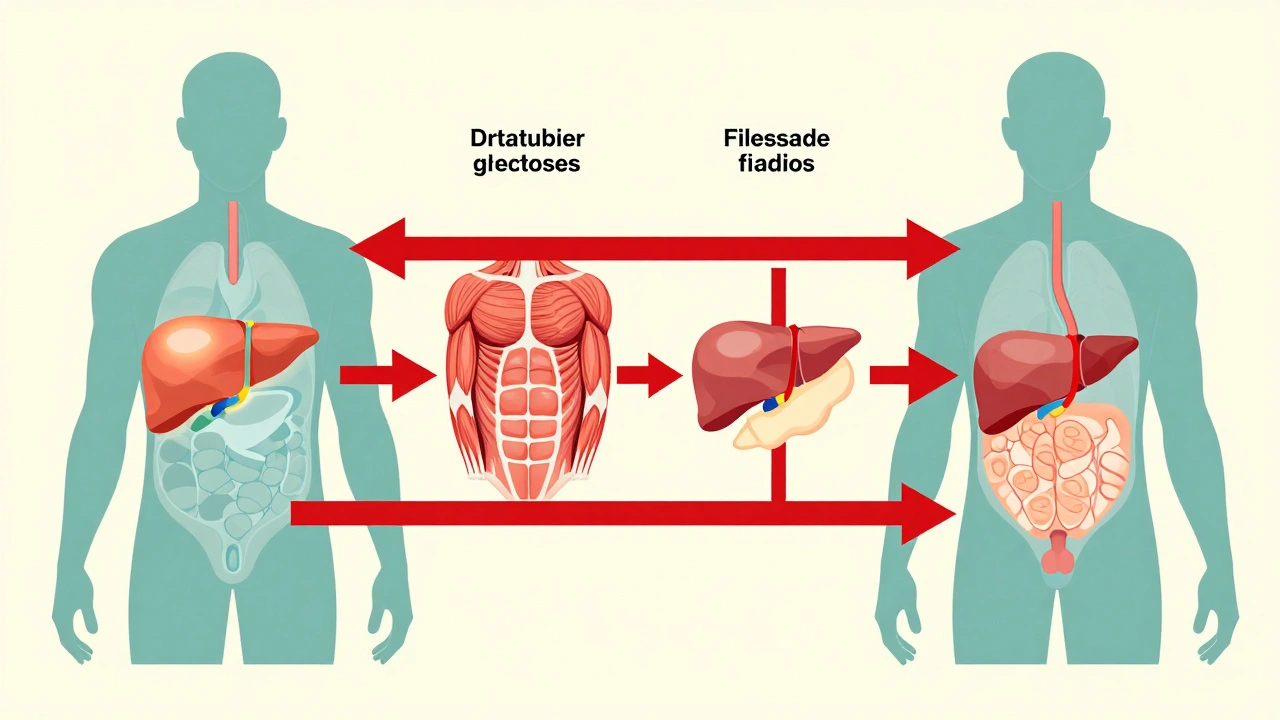
When your blood sugar stays too high, that’s hyperglycemia, a condition where glucose builds up in the bloodstream because the body can’t use or store it properly. Also known as high blood sugar, it’s not just a diabetes issue—it’s a warning sign your body’s energy system is out of balance. This isn’t about occasional sugar spikes after a big meal. Chronic hyperglycemia quietly damages nerves, blood vessels, kidneys, and eyes over time. And if left unchecked, it can lead to serious complications like diabetic ketoacidosis or long-term organ failure.
What causes it? Often, it’s tied to insulin, the hormone that tells cells to absorb glucose from the blood. If your body doesn’t make enough insulin—or if your cells stop listening to it—glucose piles up. That’s type 1 and type 2 diabetes in a nutshell. But it’s not always diabetes. Stress, certain medications, illness, or even skipping your meds can trigger spikes. And here’s something most people miss: what you eat isn’t the only factor. Lack of movement, poor sleep, and even chronic stress can make your blood sugar climb even if you’re eating "healthy."
Related to this is blood glucose, the actual measurement of sugar in your blood, usually checked with a finger prick or continuous monitor. Normal fasting levels are under 100 mg/dL. Anything above 125 mg/dL on two tests usually means diabetes. But even levels between 100 and 125—called prediabetes—are a red flag. You’re not doomed, but you’re running out of time to act. The good news? Small, consistent changes work better than drastic diets. Walking after meals, drinking water instead of soda, and getting 7 hours of sleep can lower your numbers more than any supplement.
And here’s the thing: hyperglycemia doesn’t always feel like a crisis. Many people don’t feel symptoms until their blood sugar is dangerously high. Thirst, frequent urination, blurry vision, fatigue—those are late signs. The real danger is silent damage. That’s why checking your levels regularly matters, even if you feel fine. It’s not about fear. It’s about control.
The posts below cover real-world ways to understand and manage this. You’ll find how certain medications like acarbose slow sugar absorption, why vitamin K intake matters if you’re on blood thinners (yes, it connects), how to avoid dangerous supplement interactions, and what to do when your body stops responding to your usual routine. These aren’t theory pages. They’re tools for people who live with this every day. Whether you’re newly diagnosed, managing it for years, or just worried about your numbers, what follows is practical, no-fluff advice from people who’ve been there.
Published on Dec 4
9 Comments
Corticosteroids like prednisone can cause sudden high blood sugar, even in people without diabetes. Learn how steroids trigger hyperglycemia, who’s at risk, and how to manage it safely with insulin, monitoring, and timely adjustments.