Fluid Intake: How Much You Really Need and Why It Matters for Your Health
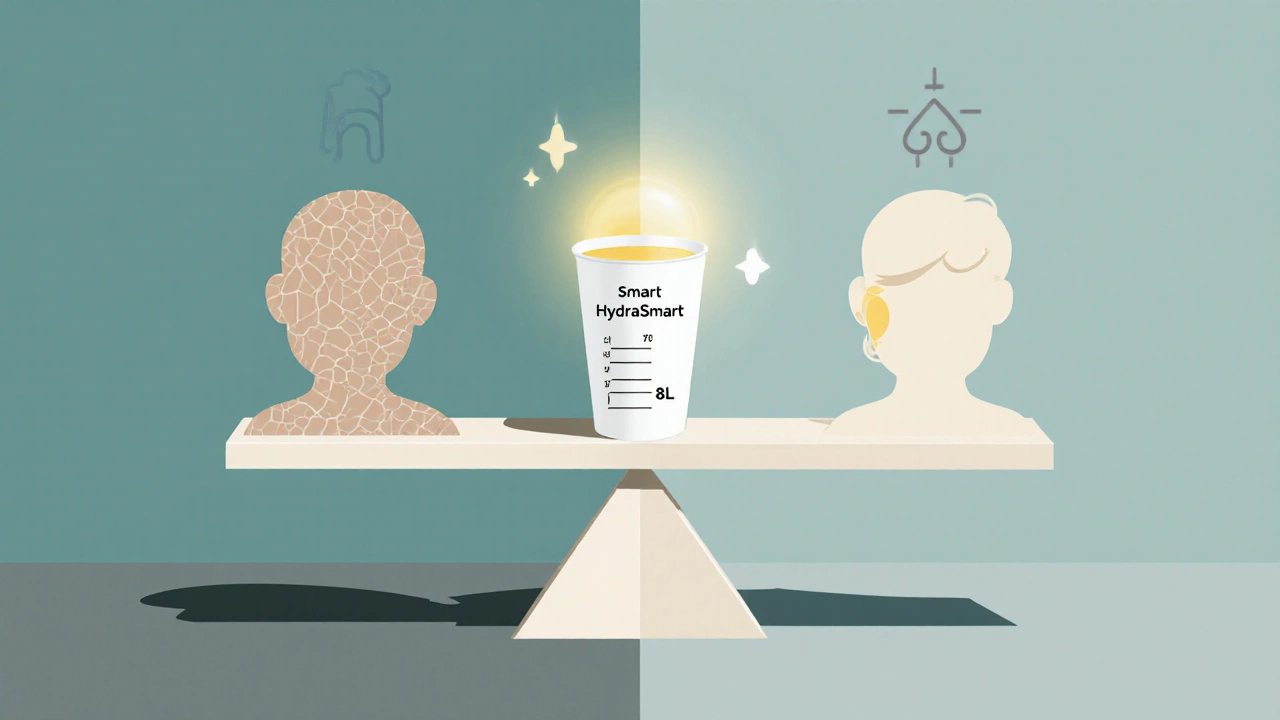
When we talk about fluid intake, the total amount of liquids consumed daily, including water, beverages, and moisture from food. Also known as hydration, it's not just about drinking water—it's a core part of how your body keeps every system running. Your kidneys, brain, heart, and even your skin rely on consistent fluid intake to do their jobs. Skip it for a day, and you’ll feel it: headaches, fatigue, dry mouth, and that dull brain fog. But drink too much? That can mess with your electrolytes too. It’s not a one-size-fits-all number.
Kidney health, how well your kidneys filter waste and balance fluids is deeply tied to your daily fluid intake. Too little, and your kidneys strain to concentrate urine, raising your risk for stones and long-term damage. Too much, and you flush out vital salts like sodium and potassium. Studies show people who drink around 2 to 2.5 liters a day—depending on weight, climate, and activity—have lower rates of kidney disease. But if you’re on dialysis or have heart failure, your doctor might tell you to limit fluids. It’s not about filling a glass every hour; it’s about matching your intake to your body’s needs.
Electrolyte balance, the levels of sodium, potassium, magnesium, and other minerals dissolved in your blood is another piece of the puzzle. Sweat, vomiting, or even just a hot day can throw this off. That’s why sports drinks aren’t always better than water—they’re only helpful if you’re sweating heavily for over an hour. For most people, plain water and eating food with natural salts (like bananas, spinach, or yogurt) is enough. Dehydration doesn’t just mean you’re thirsty—it means your cells aren’t working right. And chronic low fluid intake? It’s linked to higher blood pressure, urinary tract infections, and even confusion in older adults.
Looking at the posts here, you’ll see how fluid intake connects to everything from managing diabetes with dapagliflozin to preventing kidney disease, handling amantadine side effects like dizziness, and even how NSAIDs affect your kidneys. It’s not just a side note—it’s a foundation. Whether you’re older, on meds, active, or just trying to feel better daily, getting fluid intake right changes how your body responds to treatment, stress, and time.
You’ll find real advice here—not guesses. No "drink eight glasses" myths. Just what actually works based on health data, patient experiences, and medical guidelines. What works for someone with kidney disease won’t work for someone on diuretics. What helps an athlete won’t help someone bedridden. The right amount of fluid isn’t a number on a bottle—it’s the right fit for your body, your meds, and your life.
Published on Nov 12
15 Comments
Learn how to balance fluid intake when taking diuretics to avoid dehydration, electrolyte loss, and dangerous side effects. Practical tips for hydration, electrolytes, and daily monitoring.