Diuretic Fluid & Electrolyte Calculator
Your Diuretic Profile
Your Recommendations
Safe Daily Fluid Intake
Recommended range: 1.5 - 2 liters (6-8 cups)
Electrolyte Guidance
Critical Warning
Daily Tracking
When you’re on diuretics - often called "water pills" - your body is working harder to get rid of extra fluid. That’s the whole point. But if you don’t manage your fluid intake carefully, you can end up dehydrated, dizzy, or even in the hospital. This isn’t just about drinking more water. It’s about understanding how your body loses sodium, potassium, and fluids, and how to replace them without going too far in the other direction.
What Diuretics Do to Your Body
Diuretics like furosemide, hydrochlorothiazide, and spironolactone don’t just make you pee more. They change how your kidneys handle salt and water. Loop diuretics like furosemide block sodium reabsorption in a key part of the kidney, causing you to lose up to 2 liters of extra urine a day. Thiazides, like hydrochlorothiazide, are milder but still cause you to lose 50-100 milliequivalents of sodium daily. And potassium-sparing diuretics like spironolactone help you keep potassium, but can push your levels too high if you’re not careful.
The American Heart Association says about 48 million Americans take diuretics each year - mostly for high blood pressure or heart failure. These drugs save lives. But they also come with risks. About 15-20% of people starting diuretics experience mild dehydration within the first week. Muscle cramps, headaches, and dizziness when standing up are common signs your body is too dry.
Why Drinking Too Much or Too Little Is Dangerous
There’s no one-size-fits-all fluid goal. Too little water leads to low blood volume, which makes your heart work harder - and can actually raise your blood pressure. That’s a dangerous loop: you feel dizzy, think your diuretic isn’t working, and maybe take an extra pill. But the real problem? You’re dehydrated.
On the flip side, drinking too much can overload your system, especially if you have heart or kidney disease. A 2023 study in the New England Journal of Medicine found that 18% of heart failure readmissions were caused by patients drinking excessive fluids to "counteract" the diuretic. That’s not helping - it’s hurting.
Most experts recommend 1.5 to 2 liters (6-8 cups) of fluid daily for healthy adults on diuretics. But if your kidney function is poor (eGFR under 30), you may need to limit fluids to 1-1.5 liters. Always check with your doctor. Your ideal amount depends on your weight, age, kidney health, and the type of diuretic you’re taking.
How to Know If You’re Hydrated - Without Guessing
Don’t rely on thirst. By the time you’re thirsty, you’re already slightly dehydrated. Here’s what actually works:
- Check your morning weight. Weigh yourself at the same time every day, before eating or drinking. A drop of more than 1 kg (2.2 lbs) overnight means you lost too much fluid. A sudden gain of 1-2 kg could mean fluid buildup.
- Watch your urine color. Pale yellow? Good. Dark yellow or amber? You need more fluids. Clear urine might mean you’re overdoing it.
- Track your urine output. If you’re peeing more than 500 mL above your usual baseline, drink an extra 200-300 mL of fluid. Keep a simple log: morning weight, fluid intake, urine volume.
Patients who track these things - like one user on PatientsLikeMe who went from 4 hospital visits a year to none - see real improvements. It’s not complicated. It’s just consistent.

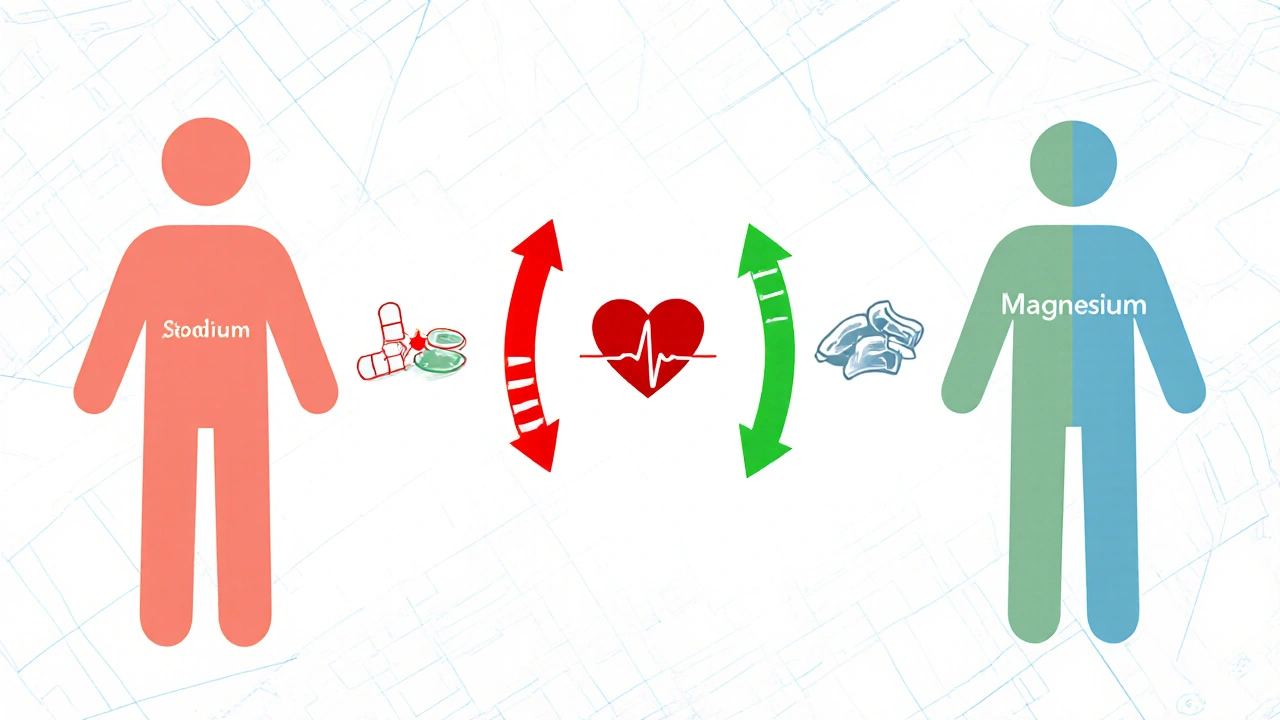
Electrolytes Matter More Than You Think
Diuretics don’t just take out water. They take out sodium, potassium, and magnesium. Thiazides can drop your potassium by 20-40 mEq per day. Loop diuretics? Up to 100 mEq. That’s why muscle cramps, irregular heartbeat, and fatigue are so common.
Potassium-sparing diuretics help, but they can cause dangerously high potassium levels - especially if you have kidney disease or take NSAIDs like ibuprofen. The key is balance. Most doctors recommend getting potassium from food: bananas, spinach, potatoes, and beans. But if you’re losing a lot, you may need a supplement.
Products like DripDrop ORS (which contains 1,000 mg sodium, 200 mg potassium, and 250 mg glucose per liter) are designed for this exact need. They’re not just water - they’re water with the right mix of electrolytes your body lost. And unlike sports drinks, they don’t overload you with sugar.
What to Avoid: Alcohol, Caffeine, and Other Traps
Alcohol is a diuretic too. So is caffeine - especially if you drink more than 250 mg a day (about 2-3 cups of coffee). Mixing these with prescription diuretics? That’s like turning up the volume on a loudspeaker.
Silver Ridge Recovery’s 2024 report found that people who drink alcohol while on diuretics are 2.7 times more likely to end up in the ER for dehydration. And 34% of patients admit they still do it. That’s not just risky - it’s life-threatening.
Even if you think you’re "just having one beer," it’s not worth it. Alcohol blocks the hormone that helps your body hold onto water. Add that to your diuretic, and you’re in trouble fast.
What Your Doctor Wants You to Do
Most doctors now follow a clear protocol:
- Check blood electrolytes within a week of starting a diuretic, then every 3-6 months if stable.
- For high-risk patients (like those on combo therapy), check every 2 weeks.
- Teach patients to track weight and urine output daily.
- Warn against alcohol and excessive caffeine.
- Recommend electrolyte-replacement solutions for those losing a lot of sodium or potassium.
Since 2021, the FDA has required all diuretic labels to include hydration warnings. In 2022, the European Medicines Agency did the same. That’s how serious this is.
New Tools Are Making It Easier
In January 2024, the FDA approved the first smart cup for diuretic users: the HydraSmart Cup. It tracks how much you drink, syncs with your phone, and sends data to your doctor. In clinical trials, it cut dehydration-related ER visits by 35%.
There’s also AI-driven hydration apps now that analyze your weight, urine output, and lab results to give real-time fluid recommendations. One trial showed a 42% improvement in electrolyte stability over 6 months.
And new combination pills are coming. PotassiSure - a pill that releases spironolactone with timed potassium - showed 58% fewer low-potassium episodes in trials. These aren’t sci-fi. They’re here.
Real Stories, Real Lessons
On Reddit, a user named CardioWarrior87 wrote: "I drank 3 liters in one day because I was so thirsty. Ended up in the ER with low potassium." That’s the trap. Thirst doesn’t mean you need to chug. It means your body is signaling imbalance.
Another user, DiureticDiva, kept a daily log: weight, fluid intake, urine volume. She adjusted slowly. Within 18 months, she went from 4 hospital visits a year to zero. She didn’t change her meds. She changed her habits.
Hydration isn’t about drinking as much as you can. It’s about drinking the right amount, at the right time, with the right balance of electrolytes.
Bottom Line: Hydration Is a Daily Practice
You don’t need to be perfect. But you do need to be consistent. Here’s what to do today:
- Buy a digital scale and weigh yourself every morning.
- Keep a small notebook or phone note: fluid intake, urine volume, weight.
- Check your urine color - aim for pale yellow.
- Avoid alcohol and limit coffee to 1-2 cups a day.
- If you’re cramping or dizzy, don’t just drink water - reach for an electrolyte solution.
- Call your doctor if your weight drops more than 1 kg overnight or you feel weak, confused, or have an irregular heartbeat.
Diuretics are powerful tools. But they’re not magic. They work best when you work with them - not against them. Balance isn’t a one-time fix. It’s a daily habit. And getting it right could mean the difference between staying healthy and ending up in the hospital.

Peter Aultman
November 14, 2025 AT 17:02Been on hydrochlorothiazide for 3 years. Weigh myself every morning like the post says. Pale yellow pee = good day. Dark yellow = drink more. Simple as that. No magic, just consistency.
Sean Hwang
November 16, 2025 AT 14:22my grandma took diuretics for her heart and she swore by bananas and a little bit of coconut water. never used those fancy drinks. just ate real food. doctors overcomplicate things sometimes.
gent wood
November 17, 2025 AT 01:16There is a profound lack of public awareness regarding the physiological interplay between diuretic therapy and electrolyte homeostasis. Many patients mistake thirst as a reliable indicator of hydration status, when in fact it is a lagging physiological signal. Daily weight monitoring, coupled with urine output tracking, provides objective data that can prevent iatrogenic complications. The data supporting this approach is robust and reproducible across multiple clinical cohorts.
Joe Goodrow
November 18, 2025 AT 03:26Why are we letting big pharma sell us overpriced electrolyte drinks when salt and water have been working for centuries? You want to replace sodium? Eat a damn pretzel. Potassium? Eat a potato. Stop buying into the wellness scam. America is getting soft.
Kevin Wagner
November 19, 2025 AT 11:48Listen up. This isn’t just advice - it’s a lifeline. I watched my uncle end up in the ER three times because he thought ‘drinking more water’ meant chugging Gatorade after every pee. He didn’t know his potassium was crashing. Then he started tracking his weight and urine color like the post says - no more hospital trips. No more panic. Just calm, smart habits. You don’t need a PhD to survive this. You just need to care enough to pay attention. Do the work. Your heart will thank you.
Jane Johnson
November 19, 2025 AT 12:36While the article presents a compelling framework for fluid management, it fails to adequately address the socioeconomic barriers faced by low-income patients who cannot afford digital scales, electrolyte solutions, or consistent access to fresh produce. The recommendation to ‘buy a digital scale’ assumes a level of privilege that is not universally available.
Brittany C
November 19, 2025 AT 20:23As a nephrology nurse, I can confirm that the 1.5–2L guideline is only appropriate for eGFR >45. For stage 3 CKD patients, fluid restriction is often critical, and urine output tracking is more predictive than weight alone. Also, DripDrop is excellent, but it’s not FDA-approved for therapeutic use - it’s a medical food. Important distinction.
Dilip Patel
November 21, 2025 AT 05:31all this talk about electrolytes and smart cups and apps… bro its 2024 and people still dont know that salt and water is all u need. in india we just drink nimbu pani with salt and sugar. works better than any fancy drink. why overcomplicate? also caffeine is fine if u dont be a wuss.
Scarlett Walker
November 21, 2025 AT 07:18I was skeptical at first but started tracking my weight and urine color. I didn’t realize how much I was losing overnight. Now I drink a little more before bed and I haven’t had a single cramp since. Small changes, huge difference.
Sean Evans
November 22, 2025 AT 06:36LOL. You people are so naive. Of course the FDA pushed this hydration nonsense. Big Pharma makes billions on DripDrop and smart cups. Meanwhile, your doctor is still prescribing HCTZ like it’s candy. Wake up. The system is rigged. Drink water. Stop buying gadgets.
Don Ablett
November 24, 2025 AT 01:37While the empirical evidence supporting daily weight monitoring is sound, the integration of such practices into routine patient self-management remains suboptimal due to cognitive load and adherence barriers. The proposed solutions, though technically valid, require behavioral architecture that is rarely addressed in clinical guidelines. A systems-level intervention may be more effective than individual compliance.
Anjan Patel
November 25, 2025 AT 12:50THIS IS WHY PEOPLE DIE. I saw a guy on the bus last week drinking 3 energy drinks and saying he was ‘hydrating’ because he’s on a diuretic. He looked like death. I wanted to scream. You’re not a soda machine. Your kidneys aren’t a coffee filter. Stop being dumb.
Barry Sanders
November 26, 2025 AT 13:21So you’re telling me a 70-year-old with heart failure should track urine output and weigh themselves daily? That’s not medicine. That’s surveillance. You’re turning patients into data points. What happened to trust? What happened to the doctor-patient relationship? This is dystopian.
kshitij pandey
November 28, 2025 AT 01:16From India to USA, this advice is universal. My uncle in Delhi uses a simple glass of water with pinch of salt and lemon every morning. No apps. No scales. Just tradition and sense. We don’t need tech to be healthy. We need common sense. And yes, banana is the real MVP.
Chris Ashley
November 29, 2025 AT 10:12bro i took a diuretic once and drank 5 liters of water and felt fine so im not sure why everyone is so scared. maybe ur body just knows what to do?