Understanding Blood Clots: What You Need to Know
If you’ve ever heard the term “blood clot” and felt unsure, you’re not alone. A clot is just a sticky lump of blood that forms inside a vein or artery. Most of the time it’s harmless, but sometimes it can block flow and cause serious problems. Knowing why clots form, how to spot them, and what to do about them can keep you safe.
What Causes Blood Clots?
Clots happen when three things line up: a damaged blood vessel, slow blood flow, and something that makes the blood extra sticky. Injuries, surgeries, or even sitting for long periods can damage vessels. Conditions like atrial fibrillation, cancer, or pregnancy also raise clot risk. Certain medicines, especially hormone pills, add to the stickiness. Lifestyle matters too—smoking, being overweight, and not moving enough all push the odds up.
How to Spot a Blood Clot
Spotting a clot early can mean faster treatment. In your legs, look for swelling, warmth, and pain that feels like cramping. The skin might turn red or bluish. If it’s in the lung (a pulmonary embolism), you could feel sudden shortness of breath, chest tightness, or a rapid heartbeat. A clot in the arm may cause a painful lump and tingling. Trust your gut—if something feels off, get checked.
Doctors usually confirm a clot with an ultrasound for legs or a CT scan for lungs. Blood tests that measure D‑dimer levels can also point to a problem. Don’t wait for perfect proof; if symptoms are severe, call emergency services right away.
Treatment Options
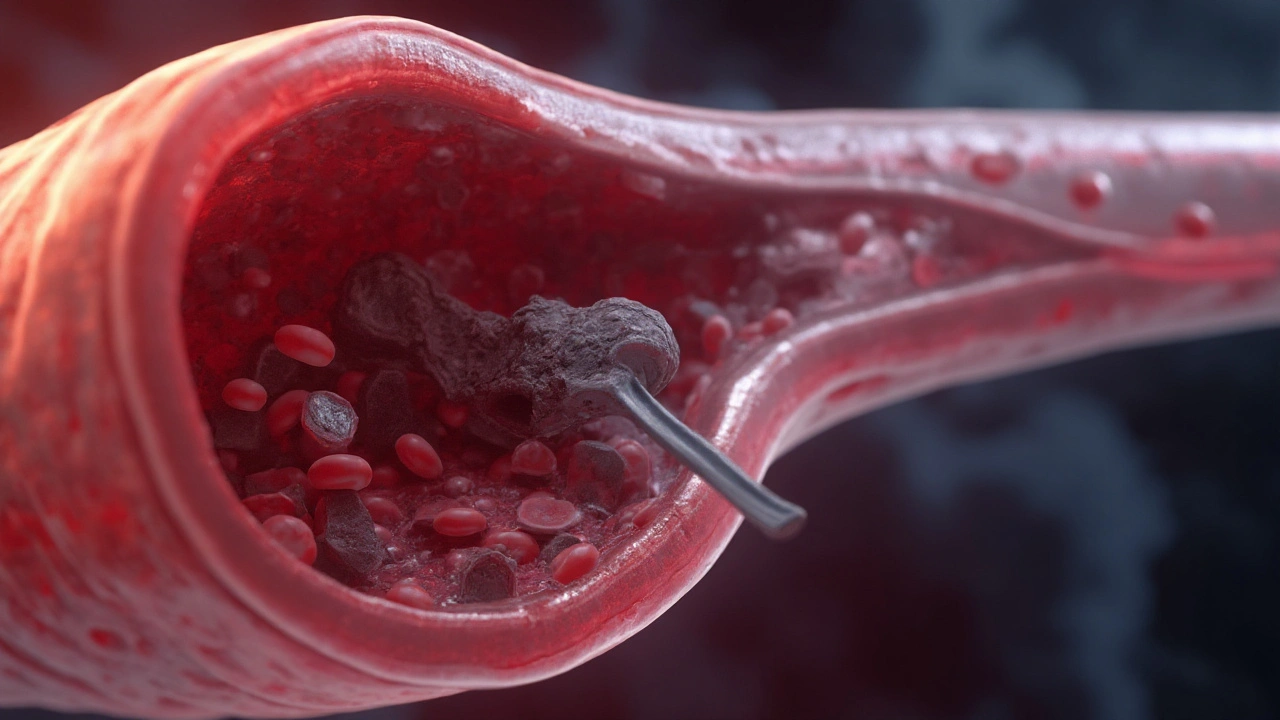
The goal of treatment is to stop the clot from growing and prevent new ones. Blood thinners like warfarin or newer drugs such as apixaban keep your blood thinner so clots don’t expand. In emergencies, doctors may use clot‑busting medicines called thrombolytics, which dissolve the clot quickly but can cause bleeding. For big clots in veins, a tiny filter might be placed in the vena cava to catch pieces before they travel.
After you start medication, regular blood checks make sure dosages stay safe. If you’re on warfarin, you’ll need frequent INR tests. Newer drugs usually need fewer check‑ups but still require follow‑up visits.
Preventing Future Clots
Prevention starts with small daily habits. Keep moving—stand up and stretch every hour if you sit at a desk. On long flights, walk the aisle or do calf raises to keep blood flowing. Stay hydrated; dehydration makes blood thicker. If your doctor says it’s safe, wear compression socks on your legs, especially after surgery.
Maintain a healthy weight, quit smoking, and limit alcohol. Talk with your doctor about any medicines you take that might raise clot risk. In some cases, low‑dose aspirin or a prescription blood thinner may be recommended for high‑risk people.
What to Do on This Site
This tag page gathers articles that touch on clot‑related topics—from drug safety to lifestyle tips. Browse the list below to find deeper dives on specific medications, nutrition advice, and real‑world stories about clot prevention. Each post is written in plain language so you can act fast if you need help.
Remember, a blood clot is serious but manageable when you know the signs and act quickly. Keep these tips handy, stay active, and reach out to your healthcare provider if anything feels off. Your health is worth the effort.
Published on Aug 26
18 Comments
Clear, practical guide to embolism: what it is, causes, symptoms, diagnosis, and modern treatments-plus prevention tips, checklists, and FAQs.