Antiepileptic Drugs: What They Are, How They Work, and What You Need to Know
When someone has epilepsy, their brain sends out abnormal electrical signals that cause seizures. Antiepileptic drugs, medications designed to reduce or prevent seizures by stabilizing brain activity. Also known as anti-seizure medications, they don’t cure epilepsy—but for many, they make daily life possible. These drugs work by calming overactive nerve cells, blocking signals that trigger seizures, or boosting the brain’s natural calming chemicals. There’s no one-size-fits-all solution. What works for one person might do nothing—or cause bad side effects—for another.
Seizure medication, a broad category that includes over 20 different antiepileptic drugs. Also known as AEDs, it includes older options like phenytoin and carbamazepine, and newer ones like lacosamide and cenobamate. Each has a different way of working. Some target sodium channels, others affect GABA or glutamate. The choice depends on seizure type, age, other health issues, and even gender. For example, valproate is highly effective but risky for women of childbearing age due to birth defect risks. That’s why doctors don’t just pick the strongest drug—they pick the safest one for you.
Drug side effects, a common concern with antiepileptic drugs, ranging from drowsiness and dizziness to serious liver or skin reactions. Many people quit their meds because of fatigue, weight gain, or brain fog—not because the seizures returned. But stopping suddenly can trigger dangerous rebound seizures. That’s why adjustments need to be slow and guided. Some side effects fade after a few weeks; others don’t. If you’re struggling, talk to your doctor before making any changes. There’s often another option.
Managing epilepsy isn’t just about popping pills. It’s about tracking what triggers your seizures—sleep loss, stress, flashing lights—and how your body reacts to each medication. Some people need just one drug. Others need combinations. And for some, even multiple drugs don’t fully stop seizures. That’s where other treatments—like vagus nerve stimulation or special diets—come in. But for most, antiepileptic drugs remain the first and most important line of defense.
The posts below cover real-world issues you might not hear about in a doctor’s office: how to handle missed doses, what to do when generics behave differently, why some people feel worse after switching brands, and how other meds—like antibiotics or painkillers—can mess with your seizure control. You’ll also find advice on dealing with side effects that no one talks about, like memory fog or mood swings. These aren’t theory pages. They’re from people who’ve lived it—and figured out what actually works.
Published on Dec 1
14 Comments
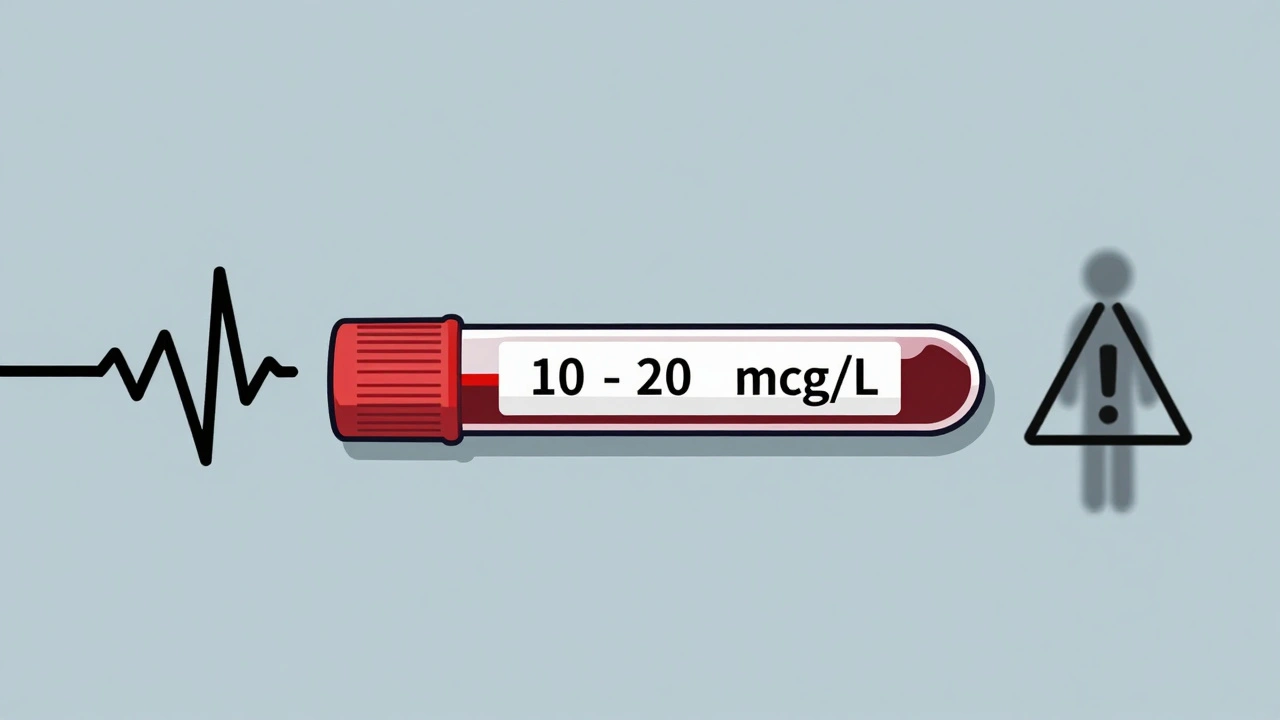
Switching generic phenytoin brands can be dangerous due to its narrow therapeutic window and non-linear metabolism. Learn when and how to monitor blood levels, correct for low albumin, and avoid toxicity or seizures.