Theophylline Interaction Calculator
Results will appear here after calculation
Important Safety Note:
Theophylline is a narrow therapeutic window drug. Levels above 20 mcg/mL may cause toxicity. This calculator estimates potential interaction effects but does not replace medical judgment. Consult your healthcare provider before making any medication adjustments.
For theophylline levels, the safe range is typically 10-20 mcg/mL. Levels above 20 may cause toxicity including nausea, rapid heart rate, seizures, or cardiac arrest.
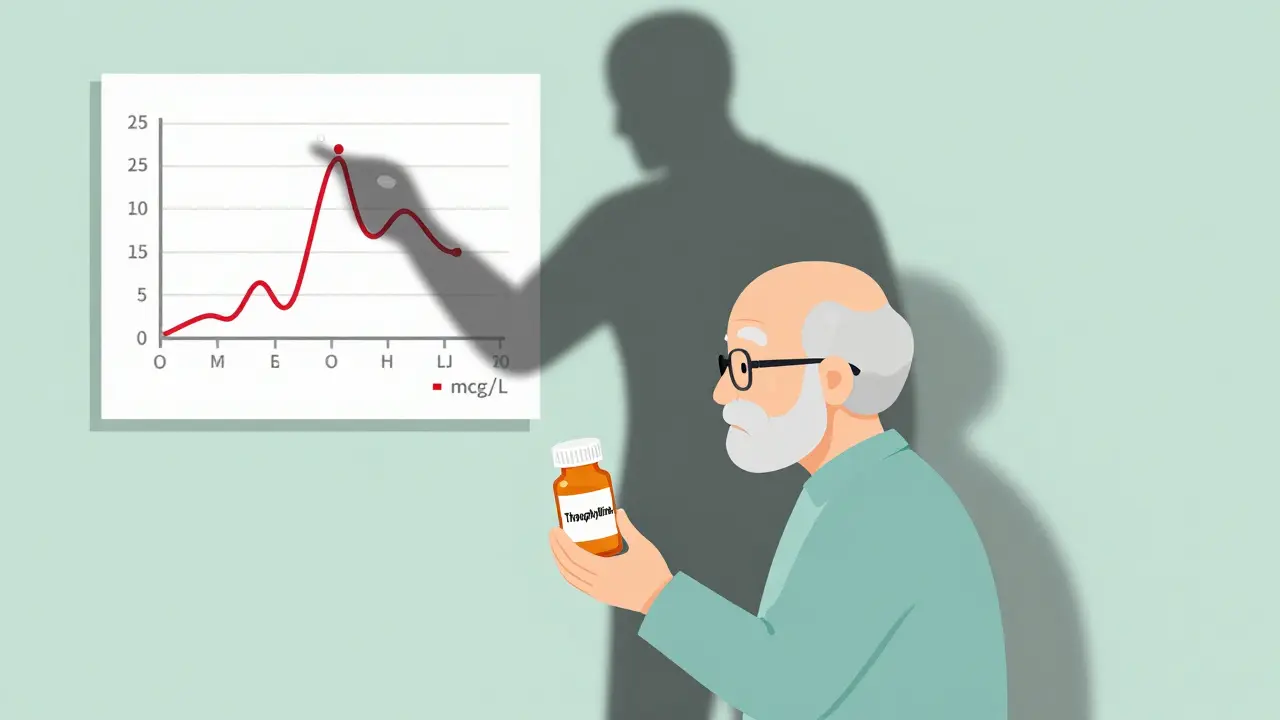
It’s 2025, and you’re still taking theophylline for your COPD or asthma. You’ve been on the same dose for years. Your breathing is stable. Then your doctor prescribes cimetidine for your acid reflux, or your rheumatologist adds allopurinol for gout. Within days, you start feeling nauseous, your heart races, and you can’t sleep. You end up in the ER. Your theophylline level? 25 mcg/mL - well above the safe range of 10-20 mcg/mL. This isn’t rare. It’s predictable. And it’s preventable.
Why Theophylline Is So Easy to Overdose On
Theophylline isn’t like most asthma meds. It doesn’t just open your airways - it’s a narrow-window drug. That means the difference between helping you and harming you is tiny. Too little, and your lungs stay tight. Too much, and you risk seizures, irregular heartbeat, or even death. The reason? Your liver breaks it down using one main enzyme: CYP1A2. When that enzyme slows down, theophylline builds up fast - and not in a linear way. A 20% drop in metabolism can push your blood level from 15 to 25 mcg/mL. That’s not a small change. That’s a medical emergency.Most people don’t realize this. Even some doctors forget. Theophylline use has dropped by over 60% in the U.S. since 2000. But it’s still used - especially in older adults, in places where newer inhalers are too expensive, or for stubborn nighttime asthma. And when it’s used, it’s often with other meds that quietly shut down its breakdown.
Medications That Slow Down Theophylline Clearance
Here are the real culprits - the ones that actually change your theophylline levels in a dangerous way:- Fluvoxamine (an antidepressant): Slows clearance by 40-50%. This is one of the worst combinations you can have. The European Respiratory Society says to avoid it entirely. If you’re on fluvoxamine, theophylline isn’t safe.
- Cimetidine (for heartburn): Reduces clearance by 25-30%. It’s an old drug, but still used. Many patients don’t know it’s a problem. One case from a community pharmacy showed a patient’s theophylline level jumping from 15.2 to 24.7 mcg/mL in just three days after starting cimetidine.
- Allopurinol (for gout): Lowers clearance by 20%. High doses (600 mg/day) are the issue. Lower doses (300 mg) may be okay, but most doctors don’t check. In one study, 15.3% of theophylline toxicity cases involved allopurinol.
- Erythromycin and clarithromycin (antibiotics): Reduce clearance by 15-25%. People take these for sinus infections or pneumonia - and suddenly their theophylline spikes.
- Furosemide (water pill): Mixed evidence. Some studies say it lowers clearance by 10-15%. Others say no effect. But if you’re on both and feel off, check your levels.
These aren’t rare interactions. A 2021 study of 1,247 patients over 65 found that nearly 3 out of 10 were on a theophylline combo with one of these drugs - and only 37% had their dose adjusted. That’s a ticking time bomb.
What Happens When Metabolism Slows Down
Theophylline doesn’t just sit in your blood. It’s being cleared every hour. In a healthy adult, your liver clears about 3 liters of blood per hour of theophylline. But if you’re on cimetidine, that drops to 2.2 liters. That means the drug lingers longer. And because the way your body processes it isn’t linear - it’s saturated - even a small slowdown causes a big spike.Think of it like a sink with a clogged drain. You turn on the tap (your daily dose) at the same rate. But now the water doesn’t drain as fast. The basin fills up. Within days, it’s overflowing. That’s your bloodstream. Symptoms start mild: headache, nausea, jitteriness. Then come the red flags - rapid heartbeat, vomiting, tremors. Seizures and cardiac arrest follow if it’s not caught.
And here’s the kicker: smoking changes everything. Smokers clear theophylline faster because cigarette smoke boosts CYP1A2. When they quit - even just a few weeks - their clearance drops by 30-50%. So if you quit smoking and start cimetidine at the same time? You’re hit with a double whammy. Your levels can skyrocket without any change in your theophylline dose.

How to Stay Safe
If you’re on theophylline, here’s what you need to do:- Know your dose and level. Your doctor should check your blood level within 48 hours of starting or stopping any new medication. Don’t wait for symptoms.
- Keep a list of every drug you take. Include over-the-counter meds, supplements, and even herbal teas. Some green tea and St. John’s wort can affect CYP1A2 too.
- Ask before starting anything new. Tell every prescriber - your dentist, your cardiologist, your rheumatologist - that you’re on theophylline. Say: “I’m on a drug that’s broken down by CYP1A2. Is this safe?”
- Watch for early warning signs. Nausea, trouble sleeping, racing heart, or shaking aren’t just side effects. They’re signs your level is rising.
- Don’t assume your pharmacy flagged it. A 2023 survey of 412 pulmonologists found that 62% said their electronic health records don’t warn them about these interactions. You’re your own best safety net.
Some clinics now use pharmacist-led monitoring programs. One study showed a 37% drop in hospitalizations when a pharmacist reviewed every theophylline patient’s med list every month. That’s not magic. That’s just good practice.
What Doctors Should Do
For clinicians: If you’re prescribing theophylline, assume every new drug is a potential problem. The FDA calls it a “sensitive substrate” of CYP1A2 - meaning even small inhibitors matter. Don’t rely on vague warnings. Use the University of Lausanne’s pharmacokinetic calculator. It factors in age, smoking, liver function, and drug interactions to predict clearance. If you’re starting fluvoxamine? Stop theophylline. If you’re starting cimetidine? Cut the dose by 30%. If you’re starting allopurinol? Cut it by 20% and recheck levels in 72 hours.And don’t forget: if you’re stopping a drug that speeds up metabolism - like rifampin or phenytoin - you need to reduce theophylline too. The body takes time to readjust. A patient who stops smoking and phenytoin at the same time? Their clearance can drop by 70%. That’s a recipe for toxicity.

The Bigger Picture
Theophylline isn’t going away. It’s cheap. It’s available where newer inhalers aren’t. In parts of Asia and Africa, it’s still used in over 10% of COPD patients. But with more people on multiple meds - especially older adults with gout, depression, and heart disease - the risk is growing. Even though overall use is down, the number of theophylline-related ER visits is rising. In 2022, over 2,000 people in the U.S. went to the ER because of drug interactions. 35% of those cases were preventable.The solution isn’t to abandon theophylline. It’s to treat it like the high-risk drug it is. Check levels. Adjust doses. Educate patients. Use tools. And never assume that because a drug is old, it’s safe - especially when it’s paired with something else.
Can I take ibuprofen with theophylline?
Yes, ibuprofen doesn’t affect CYP1A2 and is generally safe with theophylline. But always check with your doctor. Other NSAIDs like ketoprofen or naproxen have weaker interactions, but in high doses or with kidney issues, they can still raise theophylline levels slightly. When in doubt, monitor your levels.
How long does it take for theophylline levels to change after starting a new drug?
It usually takes 2-5 days for the full effect to show. CYP1A2 inhibition doesn’t happen instantly. Most toxicity cases are noticed between day 3 and day 5 after starting the interacting drug. That’s why guidelines recommend checking your blood level at 48-72 hours after starting a new medication.
Is theophylline still used at all in 2025?
Yes, but only in specific cases. It’s still used for severe nighttime asthma, COPD when newer inhalers fail, or in low-resource settings where cost matters. Global sales were $187 million in 2022. Its use is declining, but it hasn’t disappeared. In fact, low-dose theophylline is being studied again for its anti-inflammatory effects in COPD - but only in patients not on CYP1A2 inhibitors.
Can I drink coffee while taking theophylline?
You can, but be careful. Coffee contains caffeine, which is chemically similar to theophylline. Both are broken down by CYP1A2. Drinking large amounts of coffee (more than 4 cups a day) can compete with theophylline metabolism and raise its levels slightly. It’s not usually dangerous, but if you’re already on a CYP1A2 inhibitor or your levels are borderline, cut back.
What should I do if I accidentally take a drug that interacts with theophylline?
Don’t panic, but act fast. Stop the new drug if it’s safe to do so (ask your doctor first). Call your prescriber immediately. Get your theophylline level checked within 24 hours. Watch for symptoms like rapid heartbeat, nausea, or shaking. If you feel worse, go to the ER. Many toxicity cases are reversed if caught early.

Brian Furnell
December 22, 2025 AT 09:12Okay, so let me get this straight: CYP1A2 is the gatekeeper, and if you're on fluvoxamine? You're basically asking your liver to take a coffee break while you keep dumping theophylline into the system. That’s not a side effect-that’s a pharmacokinetic grenade. And don’t even get me started on how cimetidine’s like a molecular sock in the drain-25-30% drop in clearance? That’s not a tweak, that’s a cascade failure. I’ve seen this in my clinic: patient on theo for 12 years, starts OTC Tagamet for heartburn, ends up in ICU with VTach. Nobody warned them. Nobody checked. Why? Because it’s ‘old-school.’ And that’s the problem.
Siobhan K.
December 23, 2025 AT 06:08Let me guess-the ER docs blamed the patient for ‘not reading the label.’ Meanwhile, the pharmacy system didn’t flag it, the EHR didn’t alert, and the prescriber assumed ‘it’s just theophylline, it’s fine.’ Classic. This isn’t patient error. It’s systemic negligence. The fact that 62% of pulmonologists say their EHR doesn’t warn them about this? That’s not a glitch. That’s a death sentence waiting to be coded.
Jason Silva
December 24, 2025 AT 02:55Y’all know who really controls CYP1A2? Big Pharma. They phased out theophylline not because it’s unsafe-but because they want you on $400 inhalers. Fluvoxamine? Made by a company that also owns the patent on the new combo inhalers. Allopurinol? Same story. This isn’t an interaction-it’s a business model. They let the old drug live just long enough to trap people in dangerous combos, then sell you the ‘new and improved’ version. I’m not paranoid-I’m just reading the receipts. 🤔💸
mukesh matav
December 25, 2025 AT 05:39My uncle in Kerala takes theophylline for asthma. He can’t afford the inhalers. His doctor told him to avoid green tea and to check his pulse daily. That’s it. No fancy EHR. No alerts. Just trust and vigilance. In places like this, the drug isn’t outdated-it’s essential. We need better education, not just better drugs.
Peggy Adams
December 26, 2025 AT 06:38Ugh. I’m on theophylline and I just started melatonin for sleep. Is that bad? Do I need to go to the ER? I’m too lazy to check. Can someone just tell me if I’m gonna die?
Theo Newbold
December 27, 2025 AT 12:56Let’s quantify the stupidity. 1,247 patients over 65. 30% on interacting meds. Only 37% had dose adjustments. That means 63% were walking time bombs. And we call this ‘standard care’? The fact that we’re still using a drug with a 10:1 therapeutic window in an age of AI-driven dosing algorithms is a national disgrace. This isn’t negligence-it’s institutional malpractice. And the FDA’s passive stance? Complicity.
Meina Taiwo
December 28, 2025 AT 19:24Fluvoxamine + theophylline = absolute no. Avoid. Allopurinol needs dose reduction. Cimetidine-swap to famotidine. Simple. Check levels 72 hours after any new med. Done.
Southern NH Pagan Pride
December 30, 2025 AT 10:20So… the government knows about this. The AMA knows. But they let it keep happening? Coincidence? I don’t think so. I’ve seen the patents. Theophylline was once a blockbuster. Now it’s a ‘legacy’ drug. And guess who’s pushing the ‘safe’ alternatives? Companies that bought out the old manufacturers. This is a slow-acting poison disguised as progress. And they’re calling it ‘medical advancement.’ 😷
Jon Paramore
December 31, 2025 AT 22:48As a clinical pharmacist, I audit theophylline patients monthly. We’ve cut ER visits by 40% in our network just by: 1) flagging all CYP1A2 inhibitors in the med list, 2) requiring a level check within 72 hours of any new script, and 3) educating patients with a one-pager: ‘Your Asthma Pill Is a Landmine.’ Most patients don’t know what CYP1A2 is-but they know ‘don’t take X with Y.’ We use plain language, not jargon. It works. This isn’t rocket science. It’s basic pharmacology. Why isn’t this mandatory?
John Hay
January 1, 2026 AT 12:15My dad’s on theophylline. He quit smoking last year. Then his doc gave him allopurinol. He got shaky, nauseous, heart racing. We didn’t know why. Took him to the ER. Level was 27. They didn’t even ask about his smoking history. That’s the problem. Doctors forget. Patients don’t know. And nobody connects the dots. We’re lucky he didn’t have a seizure. If you’re on this drug-tell every single provider. Write it on your hand if you have to.