Medication Error Reduction Calculator
How Telepharmacy Improves Safety
Based on studies, telepharmacy reduces medication errors by 15-20% compared to clinics without remote pharmacy support. It also prevents hospitalizations due to medication problems (12.9% vs 40.2% in studies).
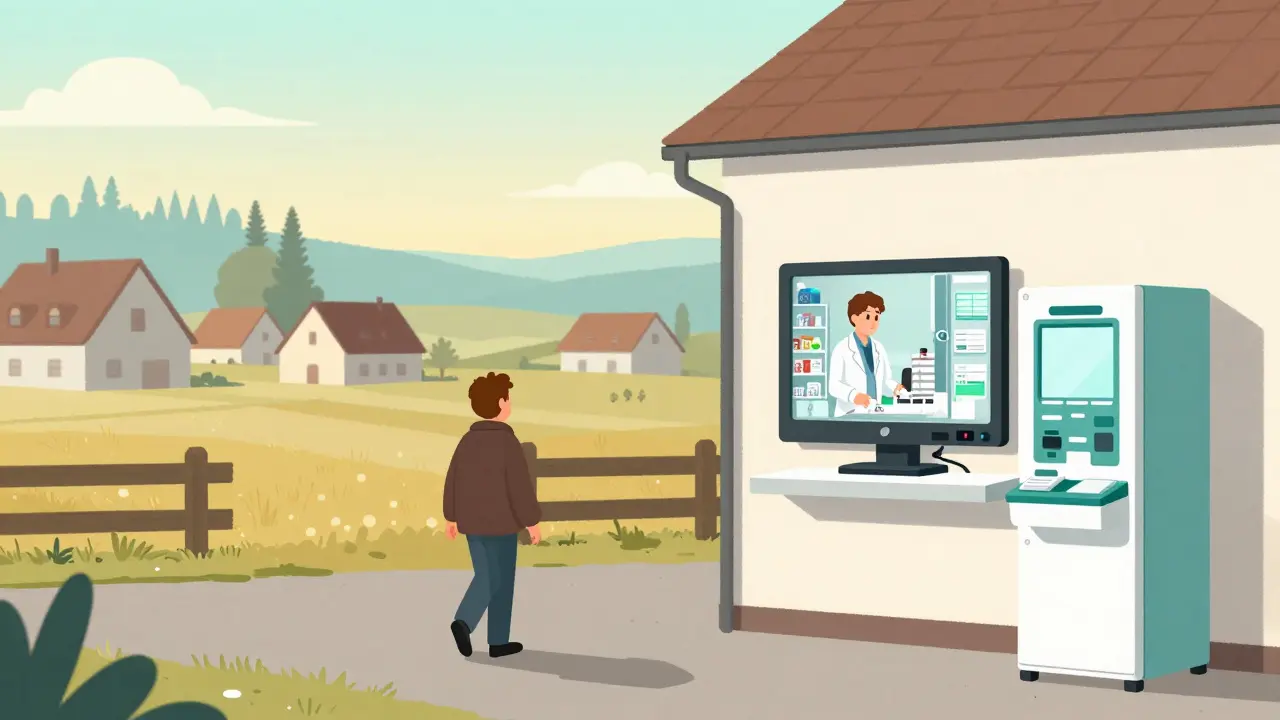
When you live in a remote town with no pharmacy nearby, getting your prescriptions filled isn’t just inconvenient-it can be dangerous. Missing a dose of blood pressure medication or not catching a dangerous drug interaction might mean a trip to the ER, or worse. That’s where telepharmacy comes in. It’s not science fiction. It’s real, growing fast, and quietly changing how millions get their meds. But does it keep people safe? Let’s look at what the data actually says.
What Telepharmacy Really Does
Telepharmacy isn’t just video calls with a pharmacist. It’s a full system: secure video consultations, automated dispensing machines, electronic prescriptions, and remote verification of meds-all managed by licensed pharmacists from a central location. Think of it like a pharmacy hub that serves dozens of small clinics, nursing homes, or rural stores. In places where hiring a full-time pharmacist is impossible, telepharmacy steps in.
North Dakota led the way back in 2001, but it wasn’t until after 2020 that this model exploded. The pandemic forced health systems to find alternatives to in-person care. By 2022, 28 states had passed laws specifically allowing telepharmacy. Today, over 42% of U.S. Health Professional Shortage Areas rely on it. That’s not a niche experiment-it’s becoming essential infrastructure.
How Safe Is It? The Numbers Don’t Lie
One of the biggest fears people have is: “Can a pharmacist really catch a dangerous mistake over a screen?” The answer, based on six major studies reviewed in 2021, is yes-almost as well as in-person pharmacies.
Research from the Journal of Health Care for the Poor and Underserved found that telepharmacy sites had medication dispensing accuracy rates between 99.2% and 99.8%. Traditional pharmacies? 99.3% to 99.9%. The difference? Statistically meaningless. That means for every 1,000 prescriptions, both models miss about one error. Not bad.
But here’s where telepharmacy shines: error prevention. One study showed telepharmacy reduced medication errors by 15-20% compared to clinics without remote pharmacy support. Why? Because pharmacists can double-check every prescription in real time. They catch drug interactions, wrong doses, and allergies before the pill leaves the machine. One South Dakota pharmacist reported catching 1.2 errors per 100 prescriptions-right on par with brick-and-mortar pharmacies.
And it’s not just about accuracy. A 2021 study in Telemedicine and e-Health tracked 3,782 patients over a year. Those with telepharmacy access had a 12.9% increase in hospitalizations due to medication problems. Those without? 40.2%. That’s a huge gap. Telepharmacy isn’t just convenient-it’s preventing life-threatening mistakes.
The Hidden Advantage: Access Saves Lives
Safety isn’t just about avoiding errors. It’s also about getting meds at all. In rural America, 1 in 5 people live in a “pharmacy desert”-a place with no pharmacy within 10 miles. A 2023 JAMA Network Open study found that states with telepharmacy laws saw a 4.5% drop in pharmacy deserts within just one year. In some areas, the number of people living without nearby pharmacy access dropped by over 11%.
One patient in rural Montana told a Reddit forum: “Being able to video chat with a pharmacist about my warfarin dosing without driving 2 hours has probably prevented at least two emergency room visits.” That’s not an outlier. It’s the norm for people who used to skip doses because the drive was too far, too expensive, or too hard.
Telepharmacy doesn’t just improve safety-it removes a barrier that was killing people slowly, quietly, and invisibly.
Where It Falls Short
But it’s not perfect.
A user in North Dakota reported a bad experience: “The video connection was poor. The technician missed my insulin allergy. I had an adverse reaction.” This isn’t rare. A 2022 survey found that 35% of telepharmacy sites struggle with unstable video or audio connections. If the connection drops during a consultation, the pharmacist can’t see if the patient is sweating, confused, or struggling to speak-signs that could mean a dangerous reaction.
And then there’s training. A 2016 study found pharmacy students performed consultations 15-20% less effectively via telepharmacy than face-to-face. Why? They weren’t trained for it. That’s still a problem today. The American Society of Health-System Pharmacists says pharmacists need 16-24 hours of special training to handle remote consultations. Not every site provides it.
Dr. Jerry Fahrni, writing in the Journal of the American Pharmacists Association, warned: “The absence of physical presence may limit the pharmacist’s ability to detect non-verbal cues indicating potential medication misuse or adverse reactions.” That’s real. You can’t feel a patient’s pulse or notice their skin color changing over Zoom.
How the Best Programs Fix These Problems
The Indian Health Service’s telepharmacy program for Navajo Nation communities doesn’t just rely on video. They use dual verification for high-risk drugs like insulin, warfarin, or opioids. Two pharmacists review every order. They also have a rule: if a patient’s case is too complex, they transfer care to an in-person pharmacy immediately.
That’s the gold standard. And it works. Their error rate? 0.45%. The national average? 0.67%. That’s 33% fewer errors.
Successful programs also have backup systems: secondary internet lines, offline prescription storage, and trained technicians who know when to pause a dispensing cycle and call for help. They don’t assume the tech will always work. They plan for failure.

What’s Next? AI, Regulation, and the Road to 2026
The market for telepharmacy is growing fast. It was worth $1.87 billion in 2022. By 2030, it could hit $6.84 billion. But growth without standards is risky.
The FDA launched a new monitoring project in January 2023 to track adverse drug events tied to telepharmacy. The Centers for Medicare & Medicaid Services now reimburses telepharmacy services under Medicare Part D. And the Patient-Centered Outcomes Research Institute is funding a $3.2 million, three-year randomized trial to finally compare safety outcomes head-to-head between telepharmacy and traditional pharmacies.
Companies like MedsAI are using artificial intelligence to predict medication errors before they happen. Early trials show a 18.7% improvement in catching dangerous drug combinations. That’s not science fiction-it’s happening now.
By 2026, analysts predict telepharmacy will match traditional pharmacy safety levels. But only if we fix the gaps: better broadband in rural areas, mandatory training for all staff, and national standards for video quality, verification, and emergency response.
Final Takeaway: It Works-If Done Right
Telepharmacy isn’t a miracle. It’s a tool. And like any tool, its safety depends on how it’s used.
The data is clear: when implemented well, telepharmacy matches-or even improves-medication safety. It prevents hospitalizations. It saves lives in places that have been ignored for decades. But poor connections, weak training, and lack of oversight can turn it into a risk.
If you’re in a rural area, it might be the only thing keeping you alive. If you’re a policymaker, it’s time to fund the infrastructure. If you’re a pharmacist, it’s time to learn how to do this right. The evidence isn’t just promising. It’s urgent.

Gloria Ricky
February 12, 2026 AT 08:55Vamsi Krishna
February 12, 2026 AT 11:45Brad Ralph
February 13, 2026 AT 11:32Suzette Smith
February 13, 2026 AT 13:21Autumn Frankart
February 15, 2026 AT 00:13Stephon Devereux
February 16, 2026 AT 15:08steve sunio
February 17, 2026 AT 07:17athmaja biju
February 18, 2026 AT 07:59Robert Petersen
February 18, 2026 AT 10:58Reggie McIntyre
February 19, 2026 AT 15:57Rachidi Toupé GAGNON
February 20, 2026 AT 15:32Alyssa Williams
February 22, 2026 AT 08:53Ernie Simsek
February 23, 2026 AT 07:39