Placebo Effect: How Belief Shapes Health Outcomes
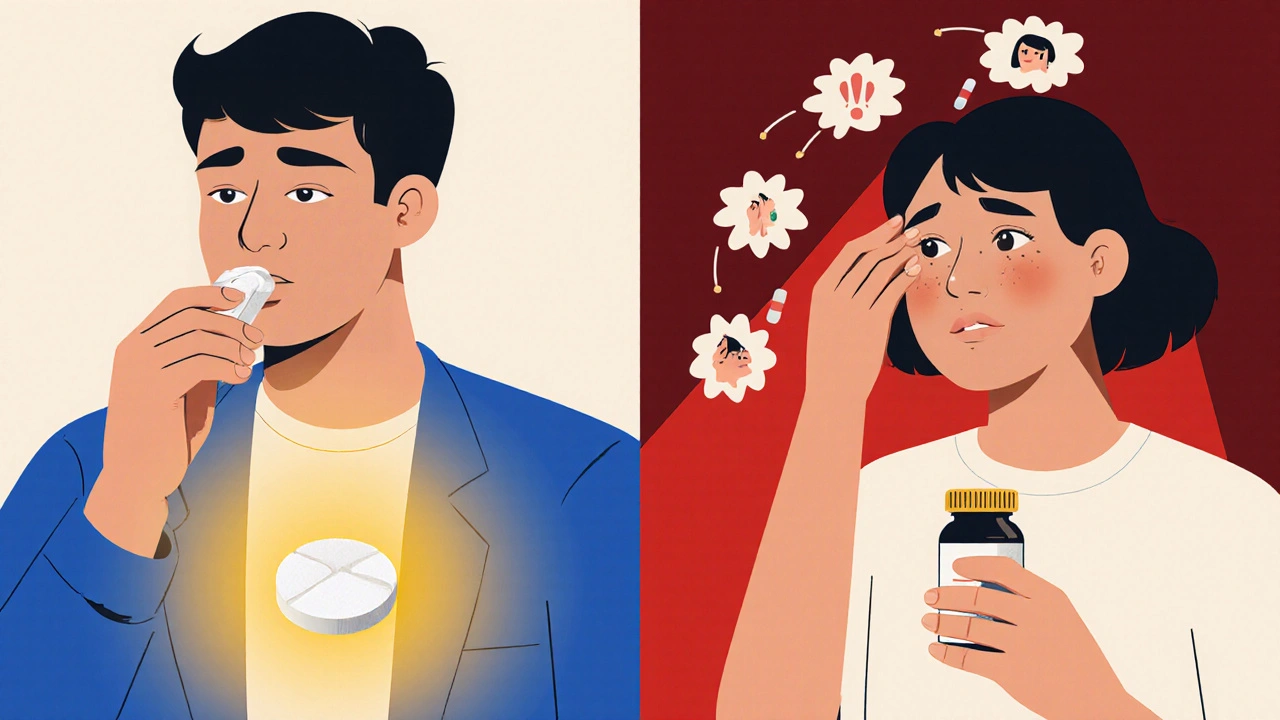
When you take a sugar pill and feel better, it’s not magic—it’s the placebo effect, a measurable change in symptoms caused by expectation rather than active medication. Also known as the placebo response, it’s one of the most powerful forces in medicine, capable of reducing pain, easing anxiety, and even altering brain chemistry—even when nothing medically active is given. This isn’t fantasy. Studies show that in some pain trials, up to 60% of patients report relief from placebos, matching or nearly matching real drugs. The brain responds to belief like it responds to chemistry: dopamine, endorphins, and other natural painkillers are released when you expect improvement.
The mind-body connection, the link between mental states and physical health outcomes is the engine behind this. If you believe a pill will help your arthritis, your nervous system may reduce inflammation on its own. If you trust your doctor’s confidence in a treatment, your stress hormones drop, and your body heals faster. This isn’t about being gullible—it’s about biology. Even in drug trials, controlled studies used to test new medications, the placebo group often shows measurable improvement, forcing researchers to prove their drug does more than just hope.
What’s surprising is how often the placebo effect shows up in real life. People with chronic back pain, depression, or even Parkinson’s have reported real symptom relief after taking inert substances. In some cases, fake surgeries—where incisions were made but no actual procedure occurred—produced outcomes nearly identical to real operations. This doesn’t mean the illness isn’t real. It means your brain has an incredible ability to influence how you experience it. That’s why doctors can’t ignore the power of context: how a treatment is delivered, how much time is spent explaining it, and how much trust is built all play a role in whether a patient improves.
And it’s not just about pills. The color of a capsule, the size of a tablet, even the price tag can change how effective a placebo feels. Blue pills work better for depression. Red pills feel stronger for pain. Expensive placebos outperform cheap ones—even when they’re identical. These aren’t quirks. They’re clues to how deeply our expectations shape healing.
What you’ll find in the posts below isn’t a list of fake cures. It’s a collection of real, science-backed stories about how belief, context, and physiology interact in ways that matter. From how antidepressants sometimes work more because of patient trust than chemistry, to why some pain medications lose effectiveness over time—these aren’t abstract ideas. They’re daily realities for people managing chronic conditions, making treatment decisions, and wondering why some therapies work for others but not for them. You’ll see how the placebo effect isn’t the enemy of medicine—it’s a part of it, and understanding it helps you get better care.
Published on Nov 17
9 Comments
Placebo and nocebo effects shape how you experience medication side effects - even when you're taking a sugar pill. Studies show up to 76% of side effects reported in trials happen in placebo groups, driven by expectations, not chemistry.