Myeloma Diagnosis: What You Need to Know
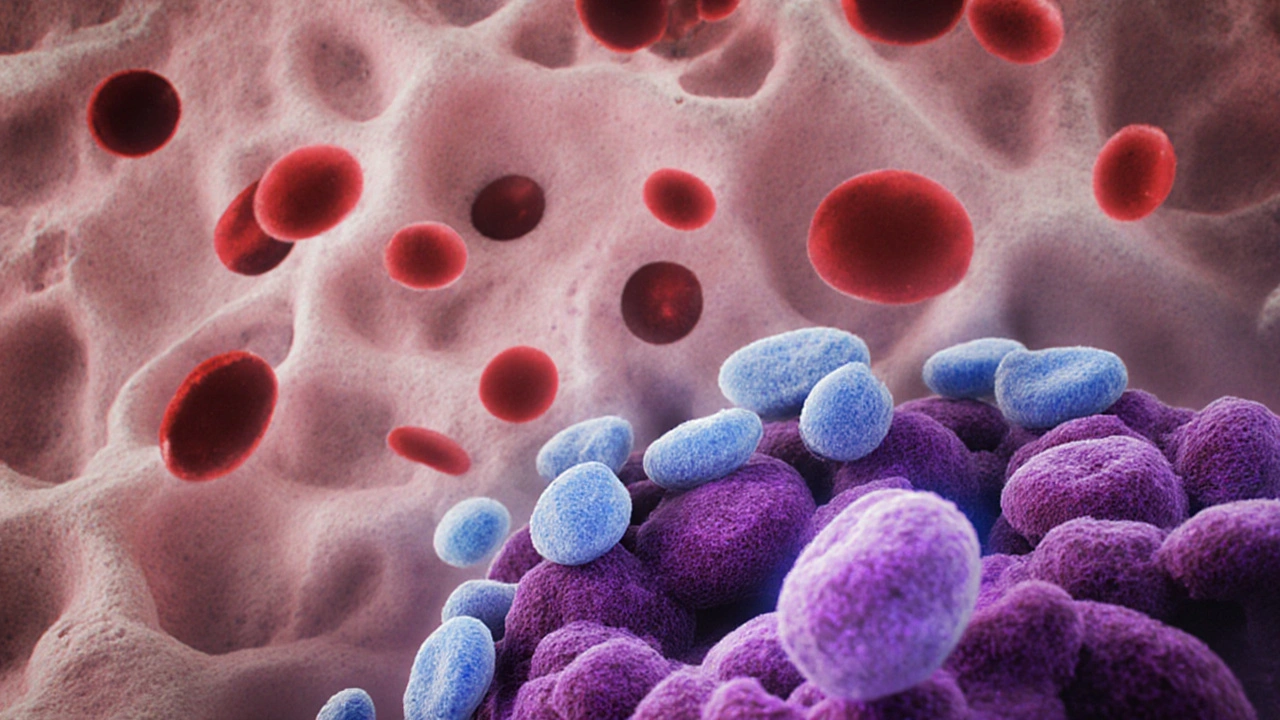
When working with myeloma diagnosis, the process of confirming multiple myeloma through labs, imaging, and tissue sampling. Also known as multiple myeloma detection, it guides treatment decisions and survival outlook. A related entity is multiple myeloma, a cancer of plasma cells that builds up in bone marrow and can cause bone pain, anemia, and kidney problems. Another key player is serum protein electrophoresis, a blood test that separates proteins to reveal abnormal monoclonal spikes. Finally, bone marrow biopsy, a procedure that extracts a small marrow sample for microscopic analysis provides definitive proof. Together, these entities form the backbone of accurate disease identification.
Why does early myeloma diagnosis matter? Because symptoms often hide behind vague complaints—persistent back pain, fatigue, or unexplained bruising. When unchecked, malignant plasma cells crowd out healthy marrow, leading to fractures, infections, and renal failure. Detecting the disease at a pre‑symptomatic stage lets doctors start therapy before organ damage sets in, dramatically improving long‑term outcomes. Moreover, the diagnostic journey isn’t just about confirming cancer; it also establishes a baseline for monitoring response to treatment and spotting relapse.
Key Tests and What They Reveal
Lab work kicks off the assessment. Serum protein electrophoresis (SPEP) screens for an M‑spike, the hallmark of monoclonal protein production. Follow‑up immunofixation pinpoints the exact immunoglobulin class, while quantitative immunoglobulin levels show how much the tumor is secreting. Serum free light chain assays add sensitivity, catching cases where traditional SPEP appears normal. Urine studies—24‑hour collection for Bence Jones proteins—capture light chains filtered by kidneys, a critical clue for renal involvement.
Imaging studies supplement blood work. Whole‑body low‑dose CT, MRI, and PET/CT map bone lesions, spinal compression, and soft‑tissue plasmacytomas. Imaging not only confirms skeletal damage but also feeds into the International Staging System, which blends lab values with radiographic findings to predict prognosis. The clearer the picture, the more precise the treatment plan.
When labs and scans point to multiple myeloma, a bone marrow biopsy seals the deal. Pathologists count plasma cells, look for clonal markers, and assess genetic abnormalities such as del(13q) or t(4;14). These cytogenetic insights influence drug choices—some mutations respond better to proteasome inhibitors, others to immunomodulatory agents. In short, the biopsy links the clinical story to the tumor’s molecular fingerprint.
Beyond the standard toolkit, newer biomarkers are reshaping the diagnostic landscape. Mass spectrometry can detect tiny amounts of monoclonal protein that SPEP misses, while circulating tumor DNA offers a non‑invasive window into genetic changes. Researchers are also exploring serum amyloid A and soluble BCMA as early warning signs. Although still emerging, these tests promise even earlier detection and real‑time monitoring of disease activity.
Putting it all together, a thorough myeloma diagnosis blends laboratory science, advanced imaging, and pathology. This multi‑modal approach not only confirms the presence of multiple myeloma but also maps its extent, uncovers high‑risk genetics, and sets the stage for personalized therapy. Below you’ll find articles that dive deeper into each of these components, compare treatment options, and share practical tips for navigating the diagnostic process.
Published on Oct 6
17 Comments
A clear, patient‑focused guide on multiple myeloma covering definition, diagnosis, symptoms, treatment options, daily management and support resources.