
Stress and Hirsutism Risk Calculator
Stress and Hirsutism Risk Assessment
This tool helps estimate your risk of stress-related hirsutism by analyzing your stress level and lifestyle factors. Results are educational and not a substitute for medical advice.
Your Stress-Related Hirsutism Risk Assessment
Ever wondered if a hectic workday could make unwanted hair sprout on your chin or chest? That’s the crux of Hirsutism is excessive, unwanted hair growth in areas where women typically have fine hair. While genetics and hormones are the usual suspects, stress is creeping onto the radar as a potential trigger. This article untangles the biology, looks at real‑world studies, and offers practical ways to keep stress from turning your skin into a forest.
Key Takeaways
- Stress spikes cortisol, which can boost androgen production and worsen hirsutism.
- People with PCOS or insulin resistance are especially vulnerable to stress‑driven hair growth.
- Clinical studies link chronic stress to higher levels of DHEA‑S (a weak androgen produced by the adrenal glands).
- Mind‑body techniques, regular exercise, and adequate sleep can blunt cortisol’s impact on hair follicles.
- Medical treatment combined with stress management offers the best odds of controlling hirsutism.
Understanding Hirsutism
Hirsutism affects about 5‑10% of women of reproductive age, according to a 2023 epidemiological survey. The condition is defined by a Ferriman‑Gallwey score of8 or higher, which assesses hair density on nine body sites. Androgens are the primary drivers; they bind to androgen receptors in hair follicles, turning fine vellus hairs into thick, pigmented terminal hairs.
Beyond the obvious cosmetic concerns, hirsutism can signal underlying endocrine disorders such as Polycystic Ovary Syndrome (PCOS) (a hormonal disorder characterized by ovarian cysts, insulin resistance, and elevated androgens. Other causes include congenital adrenal hyperplasia, androgen‑secreting tumors, and certain medications (e.g., anabolic steroids).
How Stress Messes with Hormones
When you face a deadline or a personal crisis, the hypothalamic‑pituitary‑adrenal (HPA) axis fires up. The hypothalamus releases corticotropin‑releasing hormone (CRH), prompting the pituitary to secrete adrenocorticotropic hormone (ACTH). ACTH then tells the adrenal cortex to pump out cortisol (the body’s main stress hormone, which regulates metabolism, immune response, and blood pressure).
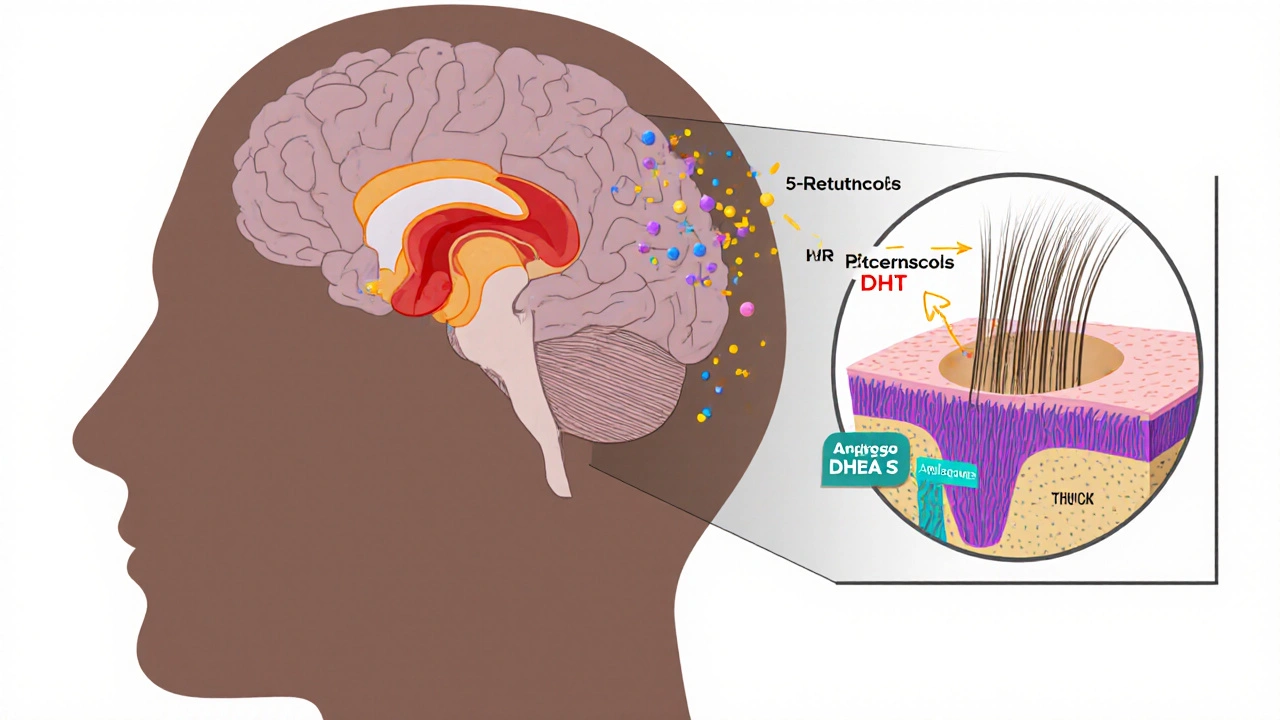
Cortisol isn’t just a fight‑or‑flight hormone; it also influences other endocrine pathways. Chronic elevation can up‑regulate enzymes that convert adrenal precursors into weak androgens like dehydroepiandrosterone sulfate (DHEA‑S). Those weak androgens can then be converted into potent testosterone in peripheral tissues, including skin. The net effect: more androgenic stimulus at the hair follicle level.
Cortisol, Androgens, and the Hair Follicle
Hair follicles have their own mini‑endocrine environment. When cortisol binds to glucocorticoid receptors on follicular cells, it can increase the expression of 5α‑reductase, the enzyme that transforms testosterone into dihydrotestosterone (DHT). DHT binds strongly to androgen receptors, accelerating the shift from vellus to terminal hairs.
Animal studies from 2022 showed that mice exposed to sustained high‑cortisol diets exhibited a 30% rise in skin DHT levels and a corresponding increase in hair shaft diameter. Human data echo this pattern: a 2024 cross‑sectional analysis of 1,200 women linked self‑reported chronic stress with a mean 12% increase in serum testosterone, even after adjusting for BMI and age.
Why PCOS and Insulin Resistance Matter
Women with PCOS already have an overactive HPA axis and higher baseline cortisol. Add chronic stress, and the hormonal cascade can tip into a feedback loop. Insulin resistance, common in PCOS, also fuels androgen production by stimulating ovarian theca cells. The combination of high insulin, cortisol, and androgens creates a perfect storm for hirsutism.
A 2023 randomized trial compared two groups of PCOS patients: one received standard metformin therapy, the other received metformin plus a mindfulness‑based stress reduction program. After six months, the stress‑reduction group saw a 20% drop in Ferriman‑Gallwey scores versus a 5% drop in the control arm, underscoring the tangible impact of stress management.
Clinical Evidence: What the Studies Say
Here’s a quick snapshot of recent research linking stress to hair growth:
- 2022 longitudinal cohort (n=3,500) - women reporting high perceived stress had a 1.4‑fold higher odds of developing new hirsutism over 5years.
- 2024 meta‑analysis of 12 trials - cortisol‑blocking agents (e.g., mifepristone) reduced serum testosterone by 8% and improved hair scores in 68% of participants.
- 2021 case‑control study - cortisol awakening response was significantly steeper in women with severe hirsutism compared to matched controls.
While the data aren’t yet definitive enough to declare stress the sole cause, the pattern is clear: stress amplifies androgenic activity and can worsen existing hirsutism.
Managing Stress to Keep Hair Growth in Check
Given the hormonal interplay, tackling stress isn’t just about feeling better-it’s a concrete strategy for hair control. Below are evidence‑backed tactics:
- Mind‑body practices: Yoga, meditation, and progressive muscle relaxation have been shown to lower cortisol by 15‑20% in controlled trials.
- Regular aerobic exercise: 30minutes of moderate activity (e.g., brisk walking) five times a week improves insulin sensitivity and blunts HPA activation.
- Sleep hygiene: Aim for 7‑9hours; sleep deprivation raises ACTH and cortisol dramatically.
- Nutrition: A low‑glycemic diet stabilizes blood sugar, reducing insulin spikes that can fuel androgen synthesis.
- Cognitive behavioral therapy (CBT): Structured CBT programs cut perceived stress scores by an average of 25% and have downstream hormonal benefits.
In practice, combining any two of these methods often yields measurable hormonal shifts within three months.
Medical Treatments Complemented by Stress Control
Traditional hirsutism therapies include oral contraceptives, anti‑androgens (e.g., spironolactone), and topical eflornithine. These address the androgenic stimulus directly. However, when stress remains unchecked, patients frequently report rebound hair growth after stopping medication.
Integrating stress management can prolong the effectiveness of pharmacologic options. For instance, a 2025 pilot study paired low‑dose oral contraceptives with an eight‑week mindfulness course; the combination group maintained a 30% lower Ferriman‑Gallwey score six months post‑treatment compared to the contraceptive‑only group.
Practical Checklist for Reducing Stress‑Induced Hair Growth
| Stress Factor | Hormonal Change | Effect on Hair Follicle |
|---|---|---|
| Cortisol spikes | ↑ 5α‑reductase activity | More DHT → terminal hair growth |
| Chronic ACTH elevation | ↑ DHEA‑S production | Peripheral conversion to testosterone |
| Insulin resistance (stress‑linked) | ↑ Ovarian androgen synthesis | Compounds existing androgen load |
Use this table as a quick reference when evaluating lifestyle factors that might be nudging your hormones toward extra hair growth.
Bottom Line
Stress isn’t a mystical villain, but its hormonal ripple effect can certainly fan the flames of hirsutism. By recognizing the cortisol‑androgen link, especially in conditions like PCOS, you can take proactive steps-both medical and lifestyle-to keep unwanted hair at bay. Think of stress management as a missing piece of the hirsutism puzzle, not just a feel‑good add‑on.
Frequently Asked Questions
Can acute stress cause a sudden increase in hair growth?
Acute stress can raise cortisol temporarily, but noticeable hair changes usually require sustained hormonal shifts. A single stressful event is unlikely to cause visible hirsutism, though repeated bouts may add up over weeks.
Is there a test to see if my hair growth is stress‑related?
Doctors often measure serum cortisol, ACTH, and androgen levels (testosterone, DHEA‑S). Elevated cortisol alongside high androgens, especially if other causes are ruled out, points toward a stress component.
Will meditation alone reduce hirsutism?
Meditation can lower cortisol, but on its own it might not reverse established hair growth. Combined with medical therapy or other lifestyle changes, it can help maintain improvements and prevent new hair from emerging.
Are there specific foods that worsen stress‑induced hirsutism?
Highly processed carbs and sugary drinks spike insulin, which can amplify androgen production. Opt for low‑glycemic foods like whole grains, legumes, and leafy greens to keep both insulin and cortisol more stable.
How long does it take to see results after reducing stress?
Hormonal shifts can appear within 4-6weeks of consistent stress‑reduction practices. Visible hair changes may lag a bit longer, often 3‑6months, as existing hairs shed and new growth patterns emerge.
Remember, tackling stress isn’t just about feeling calmer-it’s a strategic move to keep your hormones balanced and your skin smooth. If you suspect stress is fueling your hirsutism, talk to a dermatologist or endocrinologist about integrating stress‑management into your treatment plan.
stress hirsutism is a complex, but manageable, connection. By understanding the science and acting on it, you can regain control over both your emotions and your hair.

Laura MacEachern
October 4, 2025 AT 13:54Wow, this stress‑hirsutism link is something many of us overlook. Stress can really mess with hormone balance, which may lead to unwanted hair growth. Keeping stress low with meditation or a hobby can help keep those hormones in check. Remember, taking small steps each day makes a huge difference for both your skin and your peace of mind.
Alexander Rodriguez
October 4, 2025 AT 19:27Fact: Chronic stress raises cortisol, which can trigger androgen production. Those androgens are the main drivers behind hirsutism. If your stress score is high, your risk calculation will reflect that. Simple lifestyle tweaks can lower that score dramatically.
Abhinav Sharma
October 5, 2025 AT 01:01Think of your body as a symphony; stress is the discordant note that throws everything off‑balance. When cortisol spikes, the endocrine orchestra can overproduce androgens, leading to extra hair where you don’t want it. Managing stress isn’t just about feeling calmer-it’s about keeping that hormonal harmony intact. Try consistent sleep, mindful breathing, and regular movement to restore the rhythm. Small daily practices compound into big hormonal stability over time.
Vivek Koul
October 5, 2025 AT 02:07Indeed, the physiological cascade you described aligns with current endocrinology literature. Reducing chronic stress can mitigate cortisol‑induced androgen excess. Incorporating structured relaxation techniques may therefore be a prudent preventive measure.
Welcher Saltsman
October 5, 2025 AT 09:21Hey folks, just a quick heads‑up-stress really does mess with hair growth. If you’re pulling all‑nighters, expect more hair where you don’t want it. Sleep, exercise, and a balanced diet are the real MVPs here. Keep it chill and you’ll see the difference.
Frank Reed
October 5, 2025 AT 10:27Totally agree! I’ve found that even a short walk after work helps my stress levels drop. When my stress drops, the extra hair fades too. Keep it simple and steady.
april wang
October 5, 2025 AT 17:41Stress is more than just a feeling; it’s a physiological response that triggers a cascade of hormonal events. When the hypothalamic‑pituitary‑adrenal axis is activated, cortisol levels rise, and prolonged elevation can lead to an increase in adrenal androgen production. These androgens, such as DHEA‑S, are known to stimulate the hair follicles, especially in areas predisposed to hirsutism. Moreover, stress can exacerbate underlying conditions like polycystic ovary syndrome (PCOS), which already skews the hormonal milieu toward excess androgen. Sleep deprivation, a common side‑effect of chronic stress, further impairs the body’s ability to regulate these hormones, creating a feedback loop that perpetuates both stress and unwanted hair growth. Lifestyle modifications, such as implementing a regular sleep schedule, engaging in moderate‑intensity exercise at least three times a week, and practicing mindfulness or yoga, have been shown to blunt cortisol spikes. Nutrition also plays a role; low‑glycemic, balanced meals stabilize insulin and reduce inflammatory markers, which can indirectly lower androgenic activity. Consistent stress‑management practices like deep breathing, journaling, or even short, purposeful breaks during the day can reduce the overall cortisol burden. In addition, regular medical check‑ups to monitor hormone levels help identify any deviations early, allowing for timely intervention. For those already experiencing hirsutism, topical treatments like eflornithine or professional laser therapy can be adjuncts, but addressing the root cause-stress-offers a more sustainable solution. Ultimately, the interplay between stress and hair growth underscores the importance of a holistic approach to health, where mental well‑being is considered as vital as physical health.
Vishnu Raghunath
October 5, 2025 AT 23:14Oh great, another article telling us stress makes us hairy-just what the world needed, right?
Aparna Dheep
October 6, 2025 AT 04:47One must question the scientific rigor behind such simplistic correlations. Reducing complex endocrinology to “stress = hair” is intellectually lazy. While lifestyle surely matters, attributing hirsutism solely to stress smacks of reductionist thinking. A more nuanced exploration of genetics, insulin resistance, and environmental factors is warranted. Nonetheless, the piece does provide a user‑friendly entry point for lay readers.
Nicole Powell
October 6, 2025 AT 05:54Honestly, if you’re looking for a quick fix, the calculator is a gimmick. Real solutions require professional guidance, not a web form. Stop buying into the hype.
Ananthu Selvan
October 6, 2025 AT 13:07This is just another fear‑mongering post. Stress is a normal part of life; you can’t blame it for everything. Get a proper diagnosis before blaming your hair on anxiety.
Nicole Chabot
October 6, 2025 AT 18:41It’s fascinating how the body reacts to chronic stress, especially regarding hormonal pathways. The calculator can be a helpful self‑awareness tool, but it shouldn’t replace a doctor’s assessment. I’ve seen patients improve their symptoms by integrating stress‑reduction techniques like meditation and regular exercise. Consistency is key; occasional effort won’t shift the hormonal balance much.
Bailee Swenson
October 7, 2025 AT 00:14Totally agree-stress is a hidden culprit! 🌟 Don’t ignore the signs.
tony ferreres
October 7, 2025 AT 05:47From a philosophical standpoint, stress reflects our relationship with control and expectation. By reframing how we perceive pressures, we can modulate the physiological response. Practical steps-mindful breathing, setting realistic goals, and seeking community support-can reduce cortisol output. When cortisol drops, androgenic triggers wane, potentially easing hirsutism. Embrace both inner reflection and outer action for lasting change.
Arjun Premnath
October 7, 2025 AT 11:21Encouraging folks to take small, manageable steps can make a big difference. Consistent sleep, balanced meals, and a few minutes of meditation each day help keep stress in check. Over time, those habits can lower the risk of stress‑related hair growth. Keep at it, and you’ll notice the benefits.
Johnny X-Ray
October 7, 2025 AT 16:54Listen, the drama of stress turning you into a hairy beast is real. But you’ve got the power to flip the script! Dive into yoga, crank up the music, and watch the stress melt away. Your hormones will thank you, and the extra fuzz will fade. Stay dramatic in life, not in your hair.
Mark Rohde
October 7, 2025 AT 22:27Another pseudo‑science article trying to sell fear. If you’re serious about health, look beyond click‑bait calculators.
Rajan Desai
October 8, 2025 AT 04:01The connection between chronic stress and androgenic activity is supported by several peer‑reviewed studies. Elevated cortisol can alter the hypothalamic‑pituitary‑adrenal axis, leading to increased androgen synthesis. Mitigating stress through evidence‑based interventions may therefore serve as an adjunctive strategy for managing hirsutism. Nonetheless, clinical evaluation remains essential.
BJ Anderson
October 8, 2025 AT 09:34Stress can definitely make hair grow.