Steroid-NSAID Risk Calculator
Personal Risk Assessment
Risk Assessment Results
When you take a steroid like prednisone for a flare-up of arthritis or asthma, and you’re already on ibuprofen or naproxen for pain, you might think you’re just managing two separate problems. But what you’re really doing is putting your stomach in serious danger. The combination of systemic corticosteroids and NSAIDs doesn’t just add risks-it multiplies them. Studies show this mix can increase your chance of a life-threatening gastrointestinal (GI) bleed by nearly 9 times compared to taking neither drug.
Why This Combination Is So Dangerous
NSAIDs like ibuprofen, naproxen, and diclofenac work by blocking enzymes called COX-1 and COX-2. COX-2 is involved in inflammation and pain, which is why these drugs help. But COX-1 is critical for protecting your stomach lining. It helps produce prostaglandins-chemicals that keep mucus flowing, blood circulating in the stomach wall, and acid levels balanced. When NSAIDs shut down COX-1, your stomach loses its natural defense system. Corticosteroids like prednisone make things worse. They don’t just add to the damage-they interfere with healing. Steroids slow down the repair of tiny ulcers before they even become noticeable. They also reduce mucus production and can hide early warning signs like stomach pain or nausea, so you don’t realize something’s wrong until it’s severe. The result? A perfect storm where your stomach lining is weakened, healing is stalled, and symptoms are masked. The numbers don’t lie. A landmark study from 2001 found that people taking both a steroid and an NSAID had an 8.9 times higher risk of upper GI bleeding or perforation than those taking neither. For those on high-dose NSAIDs (like 1200 mg or more of ibuprofen daily), that risk jumps to over 12 times higher. And it’s not just upper GI. About one-third of NSAID-related bleeds happen in the lower intestine, not the stomach or duodenum. These are harder to detect and often more deadly.Who’s at Highest Risk?
Not everyone who takes both drugs will bleed. But certain people are sitting on a ticking clock:- People over 65
- Those with a past history of ulcers or GI bleeding
- Anyone taking blood thinners like warfarin or apixaban
- Patients on high-dose NSAIDs (e.g., diclofenac ≥100 mg/day, ibuprofen ≥1200 mg/day)
- Those taking multiple NSAIDs or combining them with aspirin
- People on long-term or repeated steroid bursts-even just 7 days of prednisone can raise risk
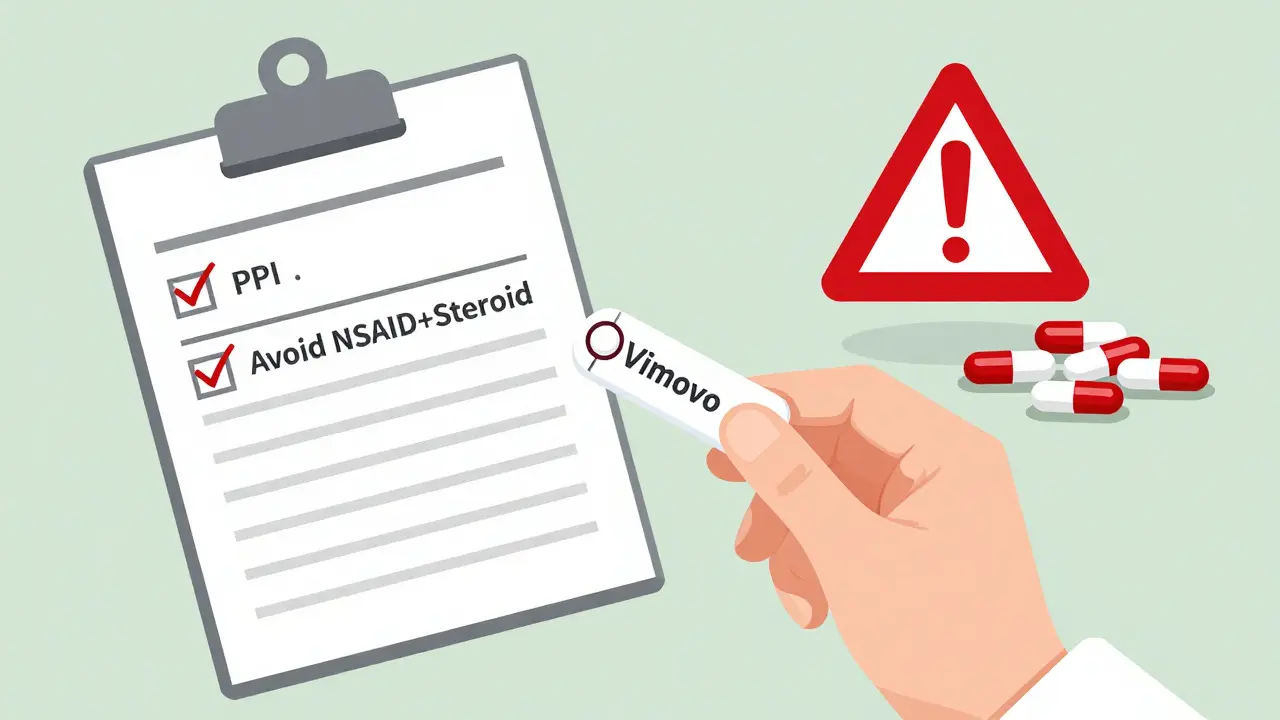
What You Can Do: Prevention Is Non-Negotiable
If you’re prescribed both a steroid and an NSAID, you need a plan. The good news? This risk is almost entirely preventable. The gold standard is a proton pump inhibitor (PPI). Drugs like omeprazole, esomeprazole, or pantoprazole work by turning down stomach acid production, giving your lining time to heal. Studies show PPIs reduce NSAID-induced ulcers by over 70%. In contrast, H2 blockers like famotidine (Pepcid) are only about half as effective. Here’s what guidelines recommend:- Standard risk: Omeprazole 20 mg daily or equivalent PPI for the entire time you’re on both drugs.
- High risk: Double dose (e.g., omeprazole 40 mg daily) if you’re over 65, have a past ulcer, or are on a blood thinner.
- Long-term use: Continue PPI as long as you’re on NSAIDs-even after the steroid is stopped, since NSAIDs alone still carry risk.
Are Some NSAIDs Safer Than Others?
Yes. Traditional NSAIDs (tNSAIDs) like naproxen and ibuprofen are the worst offenders. COX-2 inhibitors like celecoxib (Celebrex) were developed to spare the stomach. Studies show they cut upper GI bleeding risk by 50-60% compared to tNSAIDs. But here’s the catch: even celecoxib isn’t risk-free when paired with steroids. The combination still raises bleeding risk, just not as dramatically. For high-risk patients, the safest path is celecoxib + PPI-not celecoxib alone. There’s also a newer option: Vimovo (naproxen + esomeprazole). It’s a single pill combining a tNSAID with a PPI, designed specifically for patients who need both. Clinical trials showed a 54% reduction in ulcers compared to naproxen alone. It’s not perfect-it’s still a tNSAID-but it’s a step forward.What’s Going Wrong in Real Life?
Despite clear guidelines, the gap between knowledge and practice is huge. A 2022 study found that only 39% of patients on both steroids and NSAIDs were given a PPI. In non-specialist clinics, that number dropped to 22%. Many doctors still default to H2 blockers because they’re cheaper or think they’re “good enough.” They’re not. H2 blockers have a 48% higher ulcer risk than PPIs. Another common mistake? Stopping the PPI when the steroid is finished. But if you’re still taking ibuprofen for arthritis pain, your stomach is still at risk. Prophylaxis needs to last as long as the NSAID does. And then there’s the over-the-counter problem. Millions of people take daily ibuprofen for back pain or headaches while also getting a short steroid course for a sinus infection. No one tells them the risk. A 2023 survey by the NSAID Injury Foundation found 63% of patients who suffered a GI bleed had never been warned about this interaction.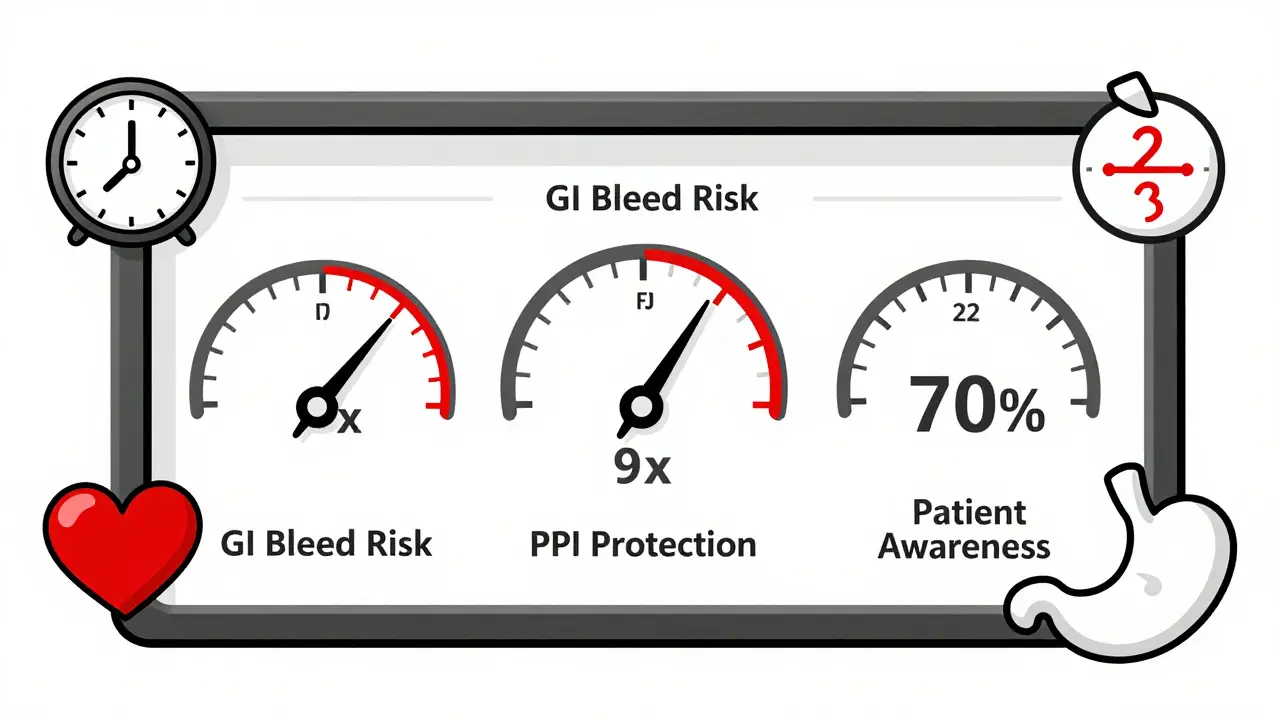
What You Should Ask Your Doctor
If you’re being prescribed a steroid and you’re already on an NSAID-or your doctor suggests starting one-ask these questions:- Is this NSAID absolutely necessary? Could I use acetaminophen (Tylenol) instead?
- Can we switch to a COX-2 inhibitor like celecoxib?
- Will you prescribe a PPI? Which one, and for how long?
- Am I at high risk based on my age, history, or other meds?
- What signs of bleeding should I watch for-black stools, vomiting blood, sudden dizziness?
The Bigger Picture
This isn’t just about one drug combo. It’s about how we prescribe. Steroid bursts are common-for allergies, back pain, even viral infections. NSAIDs are OTC and widely used. The system isn’t built to catch these overlaps. In places like Kaiser Permanente and the Mayo Clinic, where electronic systems automatically suggest PPIs when both drugs are ordered together, GI bleeding rates dropped by nearly 70%. That’s not magic-it’s smart design. The future may include genetic testing. Early research shows some people have gene variants (like CYP2C9 or PTGS1) that make them far more sensitive to NSAID damage. In the next few years, we may see personalized risk scores based on DNA. But today? The solution is simple: if you’re on steroids and NSAIDs together, you need a PPI. No exceptions. No compromises.What to Do Right Now
If you’re currently taking both a steroid and an NSAID:- Check your prescription list. Are you on omeprazole, pantoprazole, or esomeprazole?
- If not, contact your doctor or pharmacist. Ask for a PPI.
- Don’t wait for symptoms. Bleeding can happen without warning.
- If you’re taking OTC NSAIDs daily, talk to your doctor about whether you still need them while on steroids.
Can I take ibuprofen with prednisone if I use a PPI?
Yes, but only if you’re also taking a proton pump inhibitor (PPI) like omeprazole or esomeprazole. The PPI reduces stomach acid and protects your lining, which lowers the risk of bleeding. However, this combination still carries more risk than using either drug alone. Always use the lowest effective dose of ibuprofen and limit the duration. Talk to your doctor about whether an alternative pain reliever like acetaminophen might be safer.
How long should I take a PPI with steroids and NSAIDs?
You should take the PPI for the entire time you’re on the NSAID-even after the steroid is stopped. Steroids are often short-term, but NSAIDs can be taken for months or years. The stomach protection is needed as long as the NSAID is active in your system. Stopping the PPI too early leaves you vulnerable to ulcers and bleeding.
Is celecoxib safer than ibuprofen when taking steroids?
Yes, celecoxib (a COX-2 inhibitor) is significantly safer for your stomach than ibuprofen or naproxen when combined with steroids. Studies show it reduces upper GI bleeding risk by 50-60%. However, it’s not risk-free. Even celecoxib increases bleeding risk when paired with steroids, so it should still be used with a PPI in high-risk patients. Never assume a COX-2 inhibitor is safe without protection.
Can I use aspirin with steroids and NSAIDs?
Combining aspirin with both steroids and NSAIDs is extremely dangerous. Aspirin itself increases GI bleeding risk, and adding it to this mix can push your odds of a serious bleed over 13 times higher than someone taking none of these drugs. If you’re on low-dose aspirin for heart protection, talk to your doctor about alternatives or whether you can temporarily pause it during a steroid course. Never combine all three without a PPI and close medical supervision.
What are the warning signs of GI bleeding from this combo?
Symptoms can be subtle. Watch for: black, tarry stools; vomiting blood or material that looks like coffee grounds; sudden weakness, dizziness, or fainting; unexplained abdominal pain; or a rapid heart rate. Some people feel nothing until they collapse. If you’re on this drug combo and notice any of these signs, seek emergency care immediately. Don’t wait to see if it passes.
Are there natural alternatives to NSAIDs for pain while on steroids?
Acetaminophen (Tylenol) is the safest over-the-counter option for pain relief when you’re on steroids. It doesn’t affect the stomach lining or interfere with prostaglandins. For inflammation, consider non-drug approaches like ice packs, physical therapy, or gentle movement. While some people turn to turmeric or fish oil, there’s no strong evidence they’re effective enough to replace NSAIDs in moderate-to-severe pain. Always check with your doctor before starting any supplement, especially with steroids.

Angela Spagnolo
December 27, 2025 AT 18:42I’ve been on prednisone for my RA, and my doc just handed me ibuprofen like it’s candy… I didn’t know the combo could kill me. I’m now on omeprazole, and honestly? I’m terrified I waited this long. I’m telling everyone I know.
Sarah Holmes
December 29, 2025 AT 02:30It is not merely a pharmacological oversight-it is a systemic failure of medical ethics. The fact that 78% of fatal GI bleeds occur in those with prior ulcers, yet no mandatory protocol exists, reveals a healthcare system that prioritizes convenience over human life. This is not negligence; it is institutionalized violence against the vulnerable.
Jay Ara
December 30, 2025 AT 00:00bro this is wild. i had a friend who bled out after a steroid shot and kept taking naproxen for his back. no one told him. i showed him this post and he’s now on ppi. thanks for sharing. stay safe out there.
Michael Bond
December 30, 2025 AT 07:19PPIs save lives. Period.
Kuldipsinh Rathod
January 1, 2026 AT 03:52my uncle took prednisone for his lungs and ibuprofen for his knee. he ended up in ICU. no one warned him. this is so important. everyone needs to read this.
SHAKTI BHARDWAJ
January 2, 2026 AT 17:14OMG I just took celecoxib with prednisone and thought I was being SMART… so you’re saying even THAT’S dangerous?? I’m gonna die, aren’t I??!! I didn’t even know what a PPI was 10 minutes ago!!
Matthew Ingersoll
January 4, 2026 AT 00:35As someone who grew up in a household where "just take two Tylenol" was the default, I can’t believe how normalized this risk is. The fact that OTC NSAIDs are sold next to candy bars while the dangers are buried in medical journals is a cultural failure. We need public health campaigns. Not just doctor visits.
carissa projo
January 5, 2026 AT 22:48There’s something quietly heroic about taking a PPI daily-it’s not glamorous, it’s not a cure, it’s not even noticed. But it’s the quiet guardian of your insides, the unsung hero in the war against silent bleeding. For those of us who’ve seen loved ones lose their stomachs to this, it’s not just medicine-it’s reverence for the body you’re trying to keep alive.
david jackson
January 6, 2026 AT 09:24Okay, let’s go full nerd mode here-so COX-1 inhibition reduces prostaglandin E2, which normally stimulates mucus secretion and bicarbonate production, while also maintaining mucosal blood flow. But steroids? They suppress the transcription of COX-2, which is actually involved in tissue repair-so you’re not just blocking protection, you’re crippling regeneration. And the fact that H2 blockers are still being prescribed like they’re the gold standard? That’s like using duct tape to fix a ruptured pipe because it’s cheaper. We need systemic change. Not just better pills-better prescribing culture.
Jody Kennedy
January 8, 2026 AT 08:51I’m a nurse and I’ve seen this too many times. Patients come in with black stools and say, "I just took Advil for my headache." I want to scream. We need warning labels on OTC bottles. Like, right now. Like, yesterday.
christian ebongue
January 8, 2026 AT 18:16so you’re telling me i’ve been taking naproxen for 5 years and just got a 7-day steroid course… and i didn’t get a ppi? lol. guess i’m lucky. or just a statistical outlier. either way, doc, call me when you’re ready to fix this.
jesse chen
January 9, 2026 AT 05:48This is so important. I’m so glad someone put this together. I’ve been on prednisone twice now and never thought to ask about NSAIDs. I’m going to print this out and give it to my doctor. Thank you.
Joanne Smith
January 9, 2026 AT 17:48They market NSAIDs like they’re vitamins. "Take two for pain!" Meanwhile, your stomach is slowly turning into Swiss cheese and no one’s telling you. It’s not just ignorance-it’s commodification of pain relief at the cost of organ integrity. I’m not mad, I’m just… profoundly disappointed.
Prasanthi Kontemukkala
January 10, 2026 AT 17:16I’m from India, and here, people take ibuprofen like water-especially for back pain or fever. No one even knows what a PPI is. I’ve started sharing this with my family and neighbors. Maybe one person will survive because of this. That’s enough.