St. John’s Wort might seem like a safe, natural way to ease mild depression-but if you’re on any prescription medication, it could be silently undermining your treatment. This isn’t just a theoretical risk. Real people have had organ transplants fail, birth control stop working, and antidepressants lose their effect-all because they took St. John’s Wort without knowing the danger.
How St. John’s Wort Changes How Your Body Handles Medications
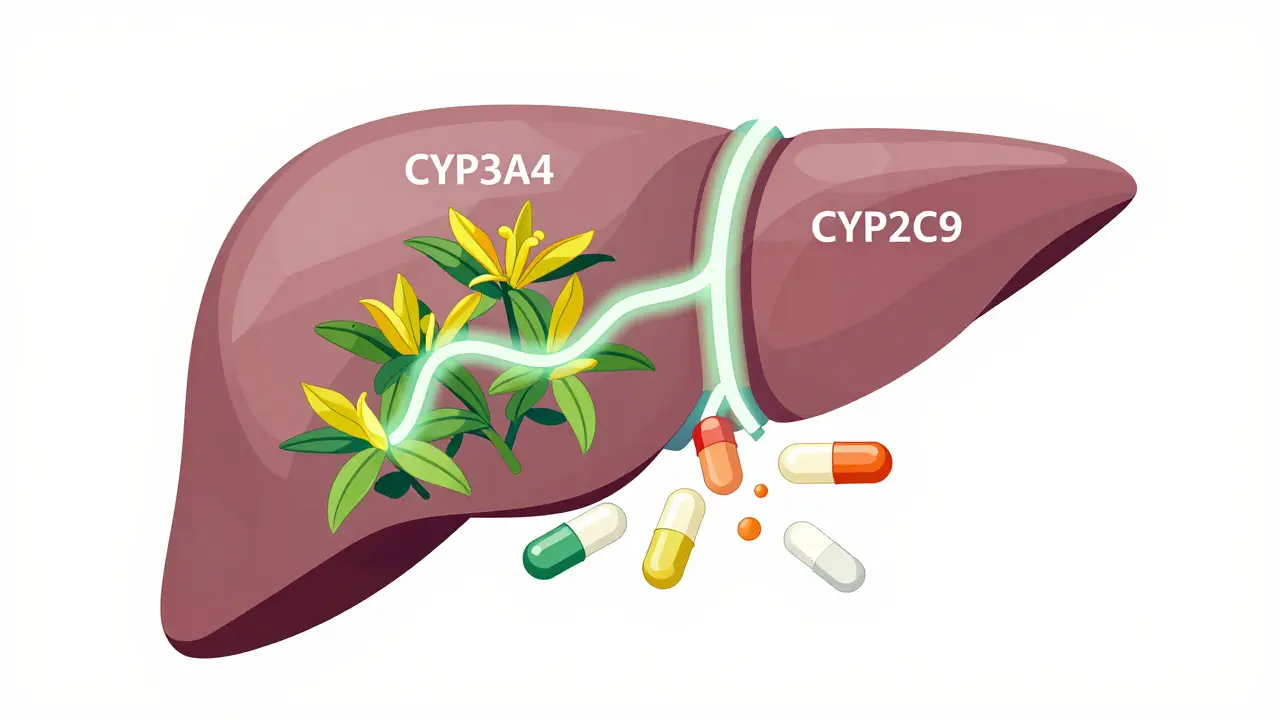
St. John’s Wort doesn’t just sit in your system. It actively rewires how your body processes drugs. The key player is hyperforin, a compound in the herb that turns on a switch in your liver called the pregnane-X-receptor (PXR). When this switch flips, your body starts producing more of certain enzymes-especially CYP3A4, CYP2C9, and CYP1A2-that break down medications faster than normal.Think of it like this: if your medication is a key that unlocks a door in your body, St. John’s Wort is a factory that makes thousands of copies of a fake key. The real key still works, but it’s lost in the crowd. Your body clears the real drug before it can do its job.
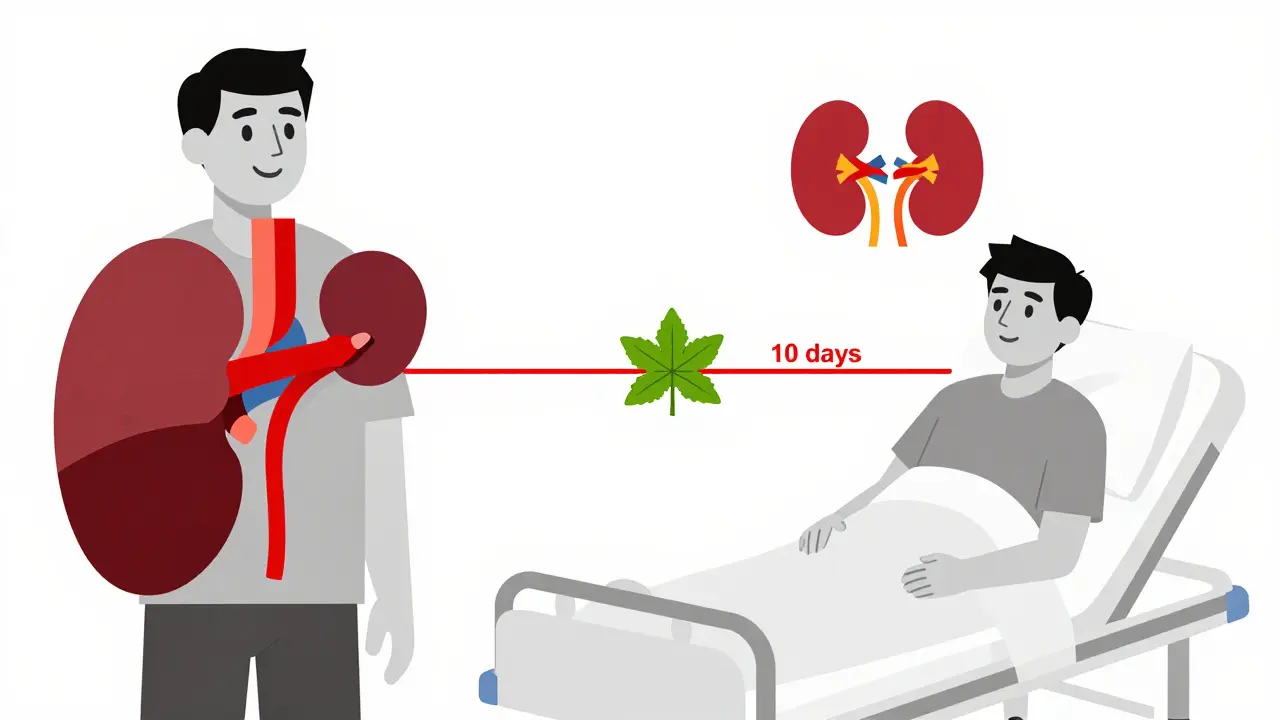
This isn’t slow or subtle. The effect builds over 10 days, and even after you stop taking St. John’s Wort, the enzymes stay elevated for up to two weeks. That means if you quit the herb, your medication might suddenly become too strong-because your body’s now slowing back down.
The Medications That Can Fail When Mixed With St. John’s Wort
You might think, “I’m not on anything dangerous.” But here’s the problem: many of the most common prescriptions are affected.- Immunosuppressants like cyclosporine, tacrolimus, and sirolimus: Used after organ transplants. One case in 2019 saw a kidney transplant patient reject her new organ because St. John’s Wort dropped tacrolimus levels by over 50%. She was on the exact same dose she’d been on for months-until she added the herb.
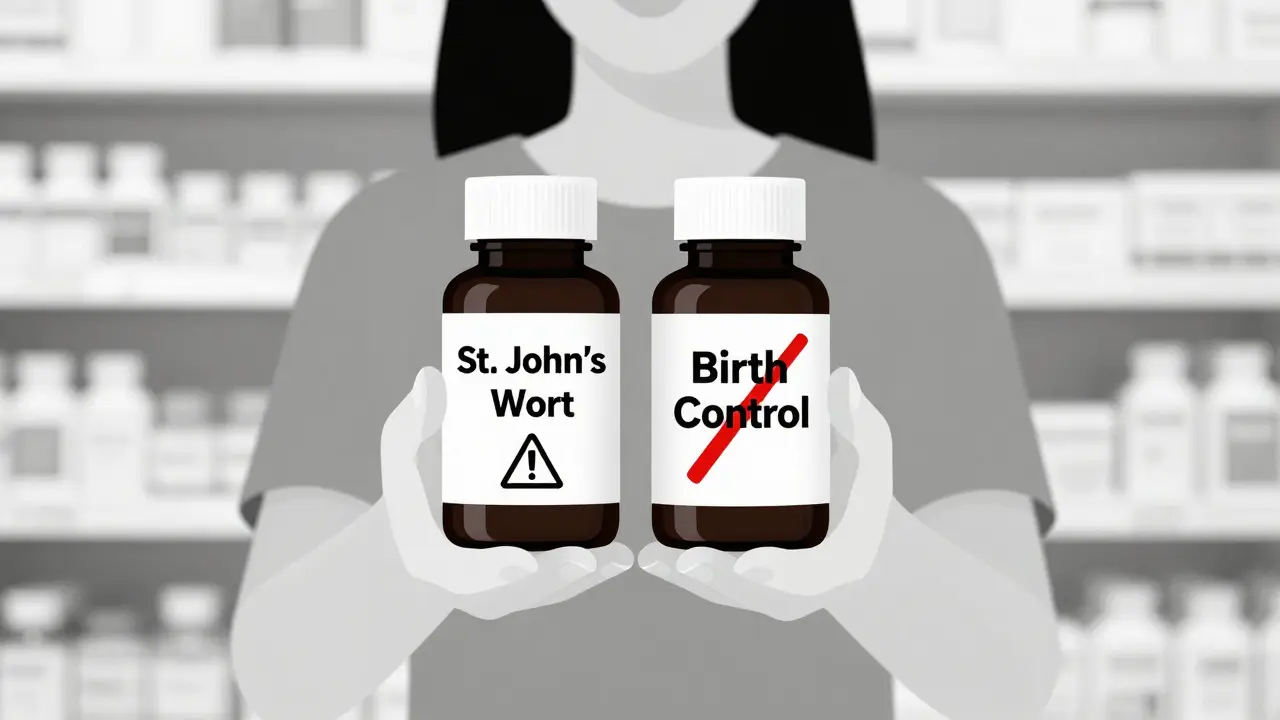
- Birth control pills: At least 17 documented cases of unintended pregnancy from women on oral contraceptives while taking St. John’s Wort. The herb speeds up estrogen breakdown, so levels drop below the threshold needed to prevent ovulation.
- Antidepressants: SSRIs like sertraline, fluoxetine, or escitalopram. Mixing them with St. John’s Wort can cause serotonin syndrome-a rare but deadly condition where your brain gets flooded with serotonin. Symptoms: high fever, confusion, rapid heartbeat, muscle rigidity. Emergency room visits from this combo are rising.
- Anticoagulants like warfarin: A 2000 case report showed a patient’s INR (a measure of blood clotting) dropped from 2.5 to 1.4 in just 10 days after starting St. John’s Wort. That’s the difference between being protected from clots and being at high risk for stroke.
- HIV medications: Protease inhibitors like ritonavir and indinavir. St. John’s Wort can slash their levels by up to 60%, turning life-saving drugs into useless ones.
- Pain meds: Oxycodone, methadone, tramadol. The herb makes these less effective, leaving patients in uncontrolled pain.
There are over 128 documented interactions. Of those, 28 are classified as major-meaning they can kill you. The European Medicines Agency says St. John’s Wort shouldn’t be used with any drug that has a narrow therapeutic index-meaning the difference between a safe dose and a toxic one is tiny.
Why This Isn’t Just a ‘Natural’ Issue
People assume herbal means safe. But St. John’s Wort is more like a prescription drug than a vitamin. It’s potent. It’s predictable. And it’s regulated like candy in the U.S.In the U.S., the FDA doesn’t approve supplements before they hit shelves. That means a bottle labeled “St. John’s Wort 300 mg” could have anywhere from 0.1% to 5% hyperforin. Two different brands, same label, wildly different risks. One might barely affect your meds. Another could cause transplant rejection.
In contrast, the European Medicines Agency requires all St. John’s Wort products sold in the EU to carry warnings for 12 specific drug classes. In Germany, where it’s the most popular antidepressant, pharmacists are trained to screen for it during every prescription refill.
Meanwhile, in the U.S., you can buy it next to the gum and candy at Walmart-with no warning labels beyond “For dietary use only.”
Who’s Most at Risk?
It’s not just people on complex meds. The biggest group using St. John’s Wort? Women aged 35 to 54. That’s exactly the demographic most likely to be on birth control, antidepressants, or cholesterol meds.According to the 2017 National Health Interview Survey, 4.7% of U.S. adults use it. That’s over 11 million people. And 8.2% of women in that 35-54 group use it-nearly 1 in 12.
Older adults? Only 1.9% use it. Why? Because they’re on more medications. They’ve seen the side effects. They’ve been warned. They know the risks.
And yet, a 2017 study found most people take 3 to 6 weeks to realize something’s wrong. A woman on birth control might think she’s just stressed. A transplant patient might think their body is rejecting the organ for “normal” reasons. By the time they connect the dots, it’s too late.
What to Do Instead
If you’re considering St. John’s Wort for depression, ask yourself: Am I on any medication-even over-the-counter? If the answer is yes, don’t risk it.There are safer alternatives:
- SAM-e: Works for mild depression. Minimal interactions-only avoid if you’re on MAO inhibitors.
- 5-HTP: A serotonin precursor. Fewer interactions than St. John’s Wort, but still avoid if you’re on SSRIs or SNRIs.
- Cognitive behavioral therapy (CBT): Proven to be as effective as antidepressants for mild to moderate depression-with zero drug interactions.
- Exercise: Just 30 minutes of brisk walking five times a week has been shown to lift mood as effectively as SSRIs in clinical trials.
And if you’re already taking St. John’s Wort? Don’t quit cold turkey. Talk to your pharmacist or doctor. They can help you taper safely and monitor your medication levels.
What You Should Do Right Now
If you’re on any prescription medication, here’s your checklist:- Look at your pill bottles. Do you take anything for depression, anxiety, heart disease, transplants, HIV, or birth control?
- If yes, check your supplement cabinet. Is there a bottle labeled St. John’s Wort?
- If yes, don’t stop taking your meds. Don’t quit the herb suddenly. Call your pharmacist.
- Ask: “Could this herb be affecting my prescription?”
- Ask them to check your blood levels for drugs like warfarin, cyclosporine, or tacrolimus if you’re on them.
There’s no shame in asking. This isn’t about being “natural” or “alternative.” It’s about staying alive.
St. John’s Wort isn’t evil. But it’s not harmless either. It’s a powerful biochemical tool-and like any tool, it can save you or hurt you, depending on how you use it.
Right now, millions of people are using it without knowing the stakes. Don’t be one of them.
Can I take St. John’s Wort with antidepressants?
No. Combining St. John’s Wort with SSRIs, SNRIs, or other antidepressants can cause serotonin syndrome-a potentially fatal condition. Symptoms include high fever, confusion, rapid heart rate, and muscle stiffness. This is not a minor side effect. It requires emergency care.
Does St. John’s Wort affect birth control?
Yes. St. John’s Wort increases the breakdown of estrogen in birth control pills, patches, and rings. This can drop hormone levels below the threshold needed to prevent ovulation. There are over 17 documented cases of unintended pregnancy in women using both. If you’re on hormonal birth control, avoid St. John’s Wort entirely.
How long does it take for St. John’s Wort to affect medications?
It takes about 10 days for St. John’s Wort to fully induce liver enzymes. But the effects can last up to two weeks after you stop taking it. That means even if you quit the herb before surgery or starting a new drug, you’re not safe until two weeks have passed.
Is St. John’s Wort regulated like a drug?
In the U.S., no. The FDA treats it as a dietary supplement, so it doesn’t need pre-market approval. In the European Union, it’s regulated as a herbal medicinal product and must carry specific interaction warnings. The lack of standardization in the U.S. means potency varies wildly between brands-some may be harmless, others deadly.
Are there safer herbal options for depression?
Yes. SAM-e and 5-HTP have fewer documented interactions, though 5-HTP should still be avoided with SSRIs. But the safest options are non-herbal: cognitive behavioral therapy (CBT) and regular exercise. Both are proven to help mild to moderate depression without interfering with any medications.
What should I do if I’m already taking St. John’s Wort and prescription drugs?
Don’t stop your prescription meds. Don’t quit St. John’s Wort suddenly. Contact your pharmacist or doctor. Bring your supplement bottle with you. They can check your medication levels-especially for drugs like warfarin, cyclosporine, or tacrolimus-and help you safely transition off St. John’s Wort if needed.

Shane McGriff
January 18, 2026 AT 23:41This is one of those posts that makes you stop and actually think. I used to take St. John’s Wort for anxiety, didn’t realize it was messing with my blood pressure med until my doctor flagged it. I thought herbal = harmless. Big mistake. Now I check every supplement with my pharmacist. Seriously, if you’re on anything prescription, don’t guess. Ask.
And yeah, CBT and walking? Game changers. I started doing 20 minutes a day and honestly? Better than any pill I’ve ever taken.
Jacob Cathro
January 19, 2026 AT 14:51bro why is everyone acting like this is news?? i’ve been saying this for years. st. john’s wort is basically a sneaky drug. u buy it next to cheetos and think ur being ‘natural’ but it’s literally sabotaging ur meds. also why does the FDA let this fly?? capitalism is a cult.
Paul Barnes
January 20, 2026 AT 22:46The enzyme induction mechanism described here is clinically accurate. CYP3A4 induction by hyperforin is well-documented in pharmacokinetic literature. The 10-day onset and two-week washout period align with peer-reviewed studies. This is not anecdotal-it’s evidence-based pharmacology. The lack of regulatory oversight in the U.S. is indefensible.
clifford hoang
January 22, 2026 AT 14:28EVERYTHING IS A GOVERNMENT TRAP. 🤡 They don’t want you to know that St. John’s Wort cures depression because Big Pharma owns the FDA. They’re scared of natural cures. That’s why they let you buy it like candy-so you’ll get sick and go back to their $200/month pills. 🚨 Also, the WHO is secretly funded by Pfizer. I’ve seen the documents. 😈
pragya mishra
January 23, 2026 AT 03:09Why do Americans think they can just swallow anything? In India, we don’t take herbs without consulting an Ayurvedic doctor. You can’t treat depression like it’s a cold. You need discipline, not magic pills. Even if it’s ‘natural,’ your body isn’t a lab experiment.
Andy Thompson
January 24, 2026 AT 05:26AMERICA IS GETTING WORSE. 🇺🇸 They let this herb be sold next to Skittles while REAL medicine is regulated like a nuclear code. It’s a socialist plot to make us weak. If you’re on birth control and take this? You deserve what happens. 🤬
kumar kc
January 25, 2026 AT 16:45St. John’s Wort is dangerous. Don’t use it. End of story.
Thomas Varner
January 25, 2026 AT 20:53Wow. I had no idea this was such a big deal. I’ve been taking it for six months with my antidepressant… I think I’m going to call my doctor tomorrow. 😅 I mean… I’ve been feeling kinda ‘off’ lately, but I thought it was just stress. Maybe not. Thanks for the wake-up call.
Emily Leigh
January 26, 2026 AT 13:29Okay but… what if I just take a tiny bit? Like, one capsule a week? Isn’t that harmless? I mean, I’ve seen people on Reddit say they mix it with SSRIs and ‘it’s fine.’ Maybe the science is exaggerated? 🤷♀️
Renee Stringer
January 28, 2026 AT 12:22I’m glad someone finally said this. I’ve been a nurse for 18 years. I’ve seen patients come in with failed transplants because they thought ‘natural’ meant ‘safe.’ It’s heartbreaking. Please, just listen to the science.
Crystal August
January 29, 2026 AT 07:32Why do people always assume herbal = better? You wouldn’t eat random mushrooms you found in the woods and call it medicine. Why is this any different? This isn’t ‘alternative health.’ It’s dangerous ignorance wrapped in a cute label.
Nadia Watson
January 30, 2026 AT 02:06As someone who grew up in a culture where herbal remedies are deeply respected, I want to say: respect doesn’t mean recklessness. In many traditions, herbs are used with precise dosing, timing, and under guidance. St. John’s Wort in the U.S. is like handing someone a loaded gun and saying ‘use wisely.’ It’s not the herb’s fault-it’s the system’s failure.
Also, CBT is amazing. I’ve seen clients transform with it. No pills. No risks. Just work. And walking? My grandmother walked two miles every morning. She lived to 97. Coincidence? I think not.
Courtney Carra
January 31, 2026 AT 22:58It’s wild how we treat plants like they’re magic and pills like they’re evil. 🌿💊 But plants are chemicals. They’re just… older chemicals. Hyperforin? That’s a molecule. Not a spiritual force. The fact that we glorify ‘natural’ while demonizing pharmaceuticals is just… irrational. And yet, here we are.
thomas wall
February 1, 2026 AT 07:24It is a matter of profound regret that the United States continues to permit the unregulated sale of substances with demonstrable, life-threatening pharmacological interactions. The European model is not merely preferable-it is morally imperative. To permit such risk in the name of ‘freedom’ is not liberty; it is negligence dressed as individualism.
Manoj Kumar Billigunta
February 1, 2026 AT 07:26I used to take this for low mood. Then I started feeling dizzy and my blood sugar went crazy. I stopped, talked to my doctor, and switched to walking every morning. Now I feel better than ever. No pills. No herbs. Just me and the sidewalk. You don’t need magic. You just need consistency.