
Getting a colonoscopy and finding polyps can be stressful. You might think, "Now I need to do this every year," but that’s not true. The good news? Most people don’t need another colonoscopy for years - sometimes even a decade. The key is understanding what kind of polyps you had, how many, and how big they were. That’s what determines when you come back.
Not All Polyps Are the Same
Not every polyp is a warning sign. Some are harmless. Others can turn into cancer over time. Doctors classify them into three main types: conventional adenomas, serrated polyps, and hyperplastic polyps. Each has its own rules for follow-up.Conventional adenomas are the most common and the most studied. If you had just one or two of them, and they were smaller than 10 mm (about the size of a pencil eraser), you’re in the lowest risk group. In the past, doctors told you to come back in 5 years. Now, based on data from over 1 million colonoscopies, the guidelines say: 7 to 10 years. Why? Because studies show your risk of developing colon cancer in that time is nearly the same as someone with a completely normal colon.
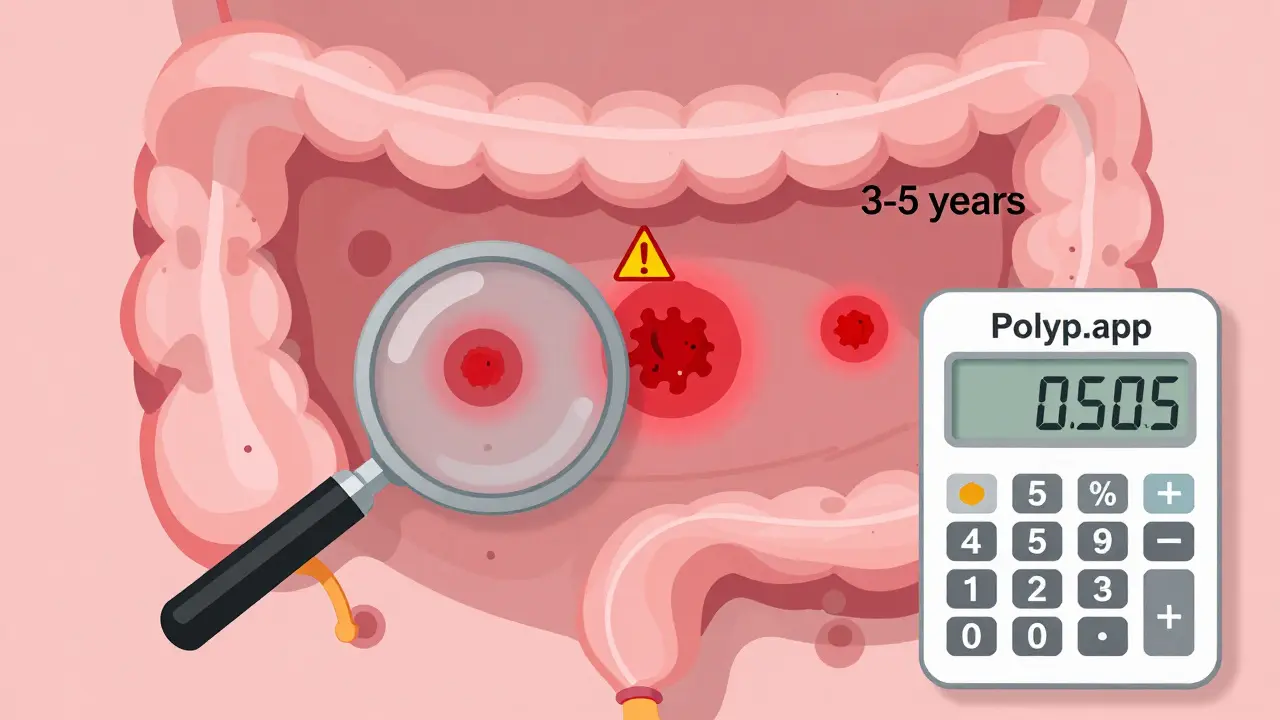
If you had three or four adenomas, all under 10 mm, the window tightens to 3 to 5 years. That’s because more polyps mean a higher chance that something else is growing unnoticed. Five or more adenomas - no matter their size - means you need a repeat colonoscopy in 3 years. This isn’t about fear. It’s about catching problems early, before they turn dangerous.
Size Matters - A Lot
The size of a polyp is one of the strongest predictors of risk. A polyp 10 mm or larger is considered high-risk, even if it’s just one. That’s because larger polyps are more likely to have pre-cancerous changes deep inside. If you had even one adenoma that big, you’re looking at a 3-year follow-up.Another high-risk feature is the shape and cell structure. If the pathologist says your polyp had villous features or high-grade dysplasia, those are red flags. They mean the cells are starting to look abnormal in ways that can lead to cancer faster. Traditional serrated adenomas (TSAs) also fall into this category. Even if they’re small, they need closer monitoring.
Then there are sessile serrated lesions (SSLs). These are trickier. They’re flat, often hard to see, and can hide in folds of the colon. If you had one or two SSLs under 10 mm, you’re still in the 5-10 year range. But if you had three to four, it drops to 3-5 years. Five or more? Back in 3 years. The tricky part? SSLs can look like harmless hyperplastic polyps. That’s why doctors sometimes err on the side of caution.
What About Hyperplastic Polyps?
Most hyperplastic polyps (HPs) are harmless. If they’re small and in the lower part of the colon, you probably don’t need another colonoscopy for 10 years - if ever. But if you had a hyperplastic polyp that was 10 mm or larger, or if it was in the right side of the colon (where serrated lesions hide), the rule changes. Now, you need a repeat colonoscopy in 3 to 5 years. Why? Because large HPs can sometimes be mistaken for SSLs, and if the colon wasn’t perfectly cleaned out, doctors can’t be sure.Also, if your bowel prep was poor, or if the polyp wasn’t fully removed, that pushes you into a shorter window. It’s not about the polyp itself - it’s about uncertainty. Medicine doesn’t like guessing when cancer is involved.
What If the Polyp Was Removed in Pieces?
Sometimes, especially with larger polyps (20 mm or more), doctors can’t remove them in one piece. They have to cut it out in chunks - called piecemeal resection. This is a problem because it’s harder to know if all the abnormal tissue is gone. The risk of leftover cells turning into cancer is higher.The U.S. guidelines say: if you had a polyp this big removed in pieces, come back in 6 months. That’s not a typo. Six months. This gives doctors a chance to look again, make sure nothing was missed, and confirm the area is healing properly. Some European guidelines say 3 to 6 months, giving doctors flexibility. But in the U.S., it’s fixed at 6 months. No exceptions.
Serrated Polyposis Syndrome: A Special Case
A rare condition called serrated polyposis syndrome (SPS) changes everything. If you have this, you’ve got a genetic tendency to develop dozens of serrated polyps. It’s not common, but if you’re diagnosed, your follow-up is intense. In Japan, you need a colonoscopy every year. In the U.K., it’s every 1 to 2 years - and you keep doing it until you’re 75. Even if no polyps are found on the next exam, you still stick to the 2-year schedule. Why? Because SPS carries a very high lifetime risk of colon cancer - up to 70% by age 80.Why Are Doctors Still Getting It Wrong?
Here’s the uncomfortable truth: many doctors still recommend colonoscopies too soon. A 2020 study at a Veterans Affairs hospital found that 81.4% of doctors who knew the updated U.S. guidelines still told patients with one or two small adenomas to come back in 5 years - even though the correct interval is 7 to 10 years. Why? Fear. Fear of missing something. Fear of lawsuits. Fear of patients getting cancer later and blaming them.And it’s not just doctors. Patients get confused too. The American Cancer Society says most people need a colonoscopy in 3 years - which is true for high-risk groups, but misleading for low-risk ones. Primary care providers, who often manage follow-up care, are even less familiar with the details. One survey found only 28.5% of doctors could correctly identify the right interval for small sessile serrated lesions.
The result? Over 60% of early repeat colonoscopies are unnecessary. That means more cost, more risk from sedation, more time off work, and more anxiety - all for no benefit.

What’s Changing in the Future?
The future of colonoscopy surveillance isn’t just about counting polyps anymore. Researchers are testing blood and stool tests that look for DNA changes linked to cancer. One study (NCT04567821) is tracking whether a simple blood test can tell you if you’re at high risk - so you might only need a colonoscopy every 10 years, or even skip it if your biomarkers are clean.Some hospitals are already using tools like Polyp.app, a free online calculator built by doctors at Massachusetts General Hospital. You plug in the number, size, and type of polyps, and it tells you exactly when to come back. It’s simple, accurate, and built on the latest guidelines.
The European Society of Gastrointestinal Endoscopy plans to update its guidelines by the end of 2024. They’re likely to tighten intervals for certain types of serrated polyps as new data comes in. The U.S. guidelines will probably shift again too.
What Should You Do?
After your colonoscopy, ask for a copy of the report. Look for these details:- Number of polyps found
- Size of each (in millimeters)
- Type (adenoma, SSL, hyperplastic)
- How they were removed (in one piece or piecemeal)
- Quality of bowel prep (good, fair, poor)
Then ask your doctor: "Based on this, when should I come back?" Don’t let them say, "Usually 5 years." Push for the exact recommendation based on your findings.
If you had low-risk polyps - one or two under 10 mm - you’re probably safe for 7 to 10 years. That’s not a suggestion. It’s science. Use that time to eat well, stay active, and avoid smoking. Those habits matter more than you think.
But if you had high-risk features - large polyps, many polyps, serrated types, or piecemeal removal - don’t delay. Follow the 3-year or 6-month window. That’s not fear. That’s protection.
How often do I need a colonoscopy if I had one small adenoma?
If you had one adenoma smaller than 10 mm and no other high-risk features, you should wait 7 to 10 years for your next colonoscopy. This is based on 2020 U.S. guidelines, which found that people in this group have nearly the same cancer risk as those with no polyps at all.
What if I had three polyps, all under 10 mm?
Three to four adenomas under 10 mm mean you should return for a colonoscopy in 3 to 5 years. This is because having multiple polyps increases your risk of developing more in the future. The exact timing depends on your overall health and bowel prep quality.
Do I need a colonoscopy every year if I had a large polyp?
No. Even with a large polyp (10 mm or larger), you don’t need yearly exams. You’ll need a repeat colonoscopy in 3 years. Only if the polyp was removed in pieces (piecemeal) and was 20 mm or larger do you come back in 6 months - not every year.
Are serrated polyps more dangerous than adenomas?
Sessile serrated lesions (SSLs) can be more dangerous because they’re flat, hard to spot, and can turn into cancer without going through the typical polyp stage. Even small SSLs require careful follow-up. One or two under 10 mm mean 5-10 years, but three or more mean 3-5 years. They’re not necessarily worse than large adenomas, but they’re harder to monitor.
Why does my doctor want me back in 5 years when I thought it was 10?
Many doctors still follow older guidelines or are unsure about the 2020 updates. Some are cautious because of legal concerns or poor bowel prep during your first exam. Ask for your report and double-check the polyp details. If you had one or two small adenomas, 7-10 years is correct. Don’t be afraid to ask for clarification.
Can I skip colonoscopy if I have a negative stool test?
Not yet. Even if you have a negative stool test (like FIT or Cologuard), you still need a colonoscopy if you’ve had polyps before. Stool tests screen for cancer or bleeding, but they can’t detect small polyps or tell you if new ones are growing. Your history of polyps means you need direct visualization - not just a stool test.

John Sonnenberg
February 8, 2026 AT 08:53Let me get this straight. You're telling me I can wait 7 to 10 years after one small adenoma? That's longer than some of my relationships. I'm not saying I'm paranoid, but I've had my colon checked more often than my car's oil. Still, if the science says it's safe, I'll believe it. Just don't tell my mom. She'd have a heart attack if I skipped a year.
And no, I won't be using that time to eat kale. I'm not a saint. I'm a man with a burger and a beer.
Joshua Smith
February 9, 2026 AT 15:55This is actually really helpful. I had my first colonoscopy last year and found one small adenoma. My doctor said 5 years, but I didn’t know about the 2020 update. I’m going to print this out and show them. It’s good to know the guidelines have changed based on real data, not just caution. I appreciate how clear this is.
Also, the part about bowel prep quality affecting timing makes sense. I didn’t realize that mattered as much as the polyp itself.
Elan Ricarte
February 11, 2026 AT 04:05Oh sweet mercy. We’re now trusting algorithms and apps to tell us when to shove a camera up our ass? Polyp.app? Sounds like a porn site for gastroenterologists. And don’t get me started on the 6-month rule for piecemeal resection. That’s not medicine, that’s a trauma bond with a colonoscope.
Let’s be real - this whole system is a money machine. Insurance companies love repeat procedures. Doctors love billing codes. Patients love not knowing they’re being played. And here we are, debating whether to come back in 3, 5, or 7 years like it’s a damn dating app.
Meanwhile, the real cause of colon cancer? Sugar. Processed meat. Sitting on your ass for 12 hours a day. But nope. Let’s just keep shoving tubes into people and calling it prevention.
THANGAVEL PARASAKTHI
February 11, 2026 AT 17:22Very informative post. I am from India and here many people avoid colonoscopy because of shame or fear. This helps to explain why timing matters. I will share with my uncle who had polyp removed last year. He was told to return in 1 year. Now I know he can wait 5-7 years if low risk. Thank you for clear details.
Also, the part about bowel prep is important. Many clinics here don't stress enough on clean prep. That's why doctors overreact.
Lyle Whyatt
February 13, 2026 AT 03:32I’ve spent the last three months researching this topic because my dad had three serrated polyps and I was terrified. This article? It’s the first thing that made sense. The distinction between SSLs and hyperplastic polyps was a game-changer for me. I didn’t realize how much morphology matters - not just size or number.
And the fact that even small SSLs can be sneaky? That’s terrifying, but also empowering. Now I know what to ask for in the pathology report. I’ve started keeping a spreadsheet - polyp type, size, location, prep quality. It’s weirdly satisfying. My wife thinks I’m obsessive. I say I’m prepared.
Also, the 6-month follow-up for piecemeal resection? That’s brutal, but necessary. I’d rather have two colonoscopies in a year than risk missing something. I’ll take the discomfort over the dread any day.
Ken Cooper
February 13, 2026 AT 23:38Wait so if I had one small adenoma and my prep was 'fair'... do I still get the 7-10 year window? Or does that get bumped up? I'm confused. My doc didn't mention prep quality. Also, what if I had a polyp removed but they said 'incomplete resection'? Does that count as piecemeal? I need to reread this 5 times.
Also, I think I'm gonna print this out and tape it to my fridge. My wife keeps asking me when I'm getting the next one. I'm tired of this conversation.
MANI V
February 14, 2026 AT 21:18Of course the guidelines changed. Because money. Always money. You think they care about your health? They care about your insurance coverage. The fact that 81% of doctors still say 5 years? That’s because they’re scared. Scared of lawsuits. Scared of being called negligent. Not scared of cancer - scared of paperwork.
And don’t even get me started on the ‘blood test future.’ That’s just the next step in making you pay for a test that doesn’t even work yet. They’ll sell you a $500 blood test and then say, ‘Oh, we still need the colonoscopy.’ Classic.
Stop pretending this is science. It’s capitalism in a white coat.
Susan Kwan
February 15, 2026 AT 01:10So let me get this straight - if I’m low risk, I can wait 7 years? That’s longer than my last relationship lasted. And yet somehow, I’m supposed to trust a camera shoved into my colon more than my instincts?
Also, why is it that when a man says ‘I’m scared of colonoscopies,’ he’s brave. When a woman says it, she’s ‘hysterical’? Just saying.
Anyway, I printed this. I’m going to use it as a paperweight. Because I’m not scheduling another one until 2031. And if my doctor says otherwise? I’m bringing this article. With highlights.
Random Guy
February 15, 2026 AT 20:087 to 10 years? Yeah right. I got one small adenoma last year. My doc said 5. I said, ‘But the article says 7–10.’ He looked at me like I just told him I believe in aliens. So now I’m waiting 5. Because I’m tired of arguing with doctors who think they’re the last word on everything.
Also, I’m pretty sure my colon is just a conspiracy theory at this point. I don’t even know what’s real anymore.
Ryan Vargas
February 17, 2026 AT 00:50There’s a deeper pattern here. The medical establishment has always been built on fear - fear of death, fear of ignorance, fear of being wrong. The colonoscopy interval guidelines? They’re not science. They’re a social contract. A ritual of control. Every time you’re told to come back in 5 years, you’re being reminded: you are not in charge of your body. The system is.
And now they want to replace it with blood tests and apps? That’s not progress. That’s surveillance with a stethoscope.
What if the real solution isn’t more scans - but less processed food, less sitting, less anxiety? But we can’t fix capitalism, so we scan your colon instead.
They don’t want you to be healthy. They want you to be monitored.
Tasha Lake
February 18, 2026 AT 00:03As a GI nurse, I see this every day. The biggest barrier isn’t cost or access - it’s misinformation. Patients walk in with outdated brochures from 2015. They’ve been told ‘every 5 years’ so long they think it’s gospel.
The Polyp.app is a game-changer. We’ve started using it in our clinic. It reduces confusion by 70%. Patients leave with a printed summary. It’s beautiful.
Also, the serrated lesion timing update? Huge. We used to lump them all with adenomas. Now we know SSLs behave differently. That’s why we’re seeing fewer interval cancers - because we’re not under-monitoring them anymore.
Sam Dickison
February 19, 2026 AT 07:06Just had my first colonoscopy. One small adenoma. Doc said 5 years. I said, ‘I read online it’s 7–10.’ He shrugged. Said, ‘I’m going with 5.’
So now I’m going to wait 7. And if he calls me? I’m gonna send him this article. Not because I’m rebellious - because I’m informed.
Also, I’m gonna start drinking more water. And maybe walk a mile a day. Just in case. Not because I’m scared. Because I’m curious.
Brett Pouser
February 20, 2026 AT 17:41As someone from a culture where talking about bowel health is taboo, this post feels like a gift. I’ve been trying to convince my cousins to get checked. Now I have real numbers. Real science. Not just ‘your uncle died, so you should go.’
My cousin in Mumbai got diagnosed last year after a stool test. He thought it was hemorrhoids. He didn’t know polyps could be silent. Now he’s got his report. We’re going to the doctor together.
This isn’t just medicine. It’s cultural change.
Karianne Jackson
February 22, 2026 AT 15:36I had one polyp. They said 5 years. I said okay. Now I’m just waiting. I don’t care about the science. I just want to be left alone.