
When a drug production line stops, it’s not just a glitch-it’s a crisis. For patients relying on life-saving medications, a single halt can mean weeks without access. In 2023, the U.S. Food and Drug Administration (FDA) reported over 200 drug shortages linked directly to quality issues, with nearly half of them stemming from manufacturing failures that forced immediate shutdowns. These aren’t rare accidents. They’re systemic risks built into how drugs are made-and they’re getting worse.
Why Quality Problems Force Production to Stop
Pharmaceutical manufacturing is one of the most tightly regulated industries on Earth. Every batch of medicine must meet exacting standards for purity, potency, and safety. A single contaminant, a wrong ingredient ratio, or even a tiny particle in the final product can trigger an automatic halt. Unlike making a car or a smartphone, where a defective unit might be recalled later, a flawed medicine can harm or kill someone. That’s why regulators demand zero tolerance. In 2022, a major antibiotic manufacturer shut down its entire facility after detecting trace amounts of a nitrosamine impurity in a batch. The issue wasn’t the amount-it was that the impurity wasn’t supposed to be there at all. The plant sat idle for six weeks while engineers traced the source to a newly replaced filter. By then, over 300,000 prescriptions had been delayed. This wasn’t a one-off. The FDA’s 2023 inspection report found that 37% of all pharmaceutical violations involved inadequate procedures for handling quality-related halts.How Long Do These Halts Last?
In most factories, a production stoppage might last minutes. In pharma, it’s measured in days or weeks. The average quality-related halt in drug manufacturing lasts 4.7 hours-but that’s just the start. The real clock starts ticking when regulators get involved. Once a problem is found, the company must stop shipping, isolate affected batches, notify the FDA, and submit a full root cause analysis. The FDA then reviews the report, which can take another 10-20 days. During that time, no new product can be released. A 2023 analysis of 89 drug shortages found that 68% of them were caused by halts that lasted longer than 30 days. That’s not a glitch-it’s a bottleneck built into the system.What Causes These Halts?
The reasons vary, but they fall into a few recurring patterns:- Contamination: Microbial growth, foreign particles, or cross-contamination between drugs. A 2022 case in India involved a sterile injectable that contained fibers from a worker’s lab coat. The entire line shut down.
- Equipment failure: A single sensor glitch can trigger a halt. In one facility, a temperature probe that was off by 0.5°C caused 17 consecutive batches to be rejected.
- Supplier issues: Active pharmaceutical ingredients (APIs) often come from overseas. A quality problem with a single API batch can stop production of dozens of drugs. In 2023, a shortage of a key blood pressure medication traced back to a Chinese supplier whose facility was shut for failing cleanliness standards.
- Human error: Wrong labels, incorrect dosing, or misrecorded data. A 2021 incident at a U.S. facility led to 12,000 bottles of insulin being labeled with the wrong concentration. All had to be destroyed.
- Changeover failures: Switching from one drug to another on the same line is risky. If cleaning isn’t perfect, residue from the previous product can contaminate the next. This caused a 14-day halt at a major generic drug maker in 2023.

The Cost of a Single Halt
The financial hit isn’t just lost production. It’s everything that follows:- Lost revenue: A single day of halted production at a top-selling drug can cost $2 million in lost sales.
- Regulatory fines: The FDA can impose penalties for repeated violations. One company paid $1.8 million in 2023 after three quality-related halts in six months.
- Recall costs: If defective product already shipped, recalls can cost 10-20 times more than preventing the issue. A 2022 recall of a cancer drug cost $43 million in logistics, legal fees, and patient compensation.
- Supply chain ripple effects: One halted drug can delay dozens of others that use the same ingredients or packaging. In 2023, a halt in the production of a common antiviral led to delays in 17 combination therapies.
According to McKinsey, quality-related halts in pharmaceutical manufacturing cost the global industry over $42 billion in 2023 alone. That’s more than the entire annual revenue of the top 10 generic drug makers combined.
Why Some Companies Handle This Better
Not all manufacturers suffer the same way. The difference? Preparation. Companies that avoid repeated halts use three key strategies:- Real-time monitoring: Sensors that track temperature, pressure, humidity, and chemical composition in real time. At one facility, this cut quality-related halts by 58% in 18 months.
- Root cause analysis training: Teams trained in methods like 5 Whys and Fishbone diagrams resolve issues faster. One company reduced average halt time from 6.8 hours to 2.1 hours after implementing this.
- Supplier quality partnerships: Instead of treating suppliers as vendors, leading manufacturers co-develop quality protocols. Johnson & Johnson now has engineers stationed at five key API suppliers to audit processes before production even begins.
These companies also empower workers. In 2023, a survey of 300 pharma plants found that those with “stop-work authority” for line operators had 41% fewer recurring quality issues. When a technician sees a problem, they don’t need permission to shut things down. They’re trained, trusted, and protected.
What’s Changing in 2025 and Beyond
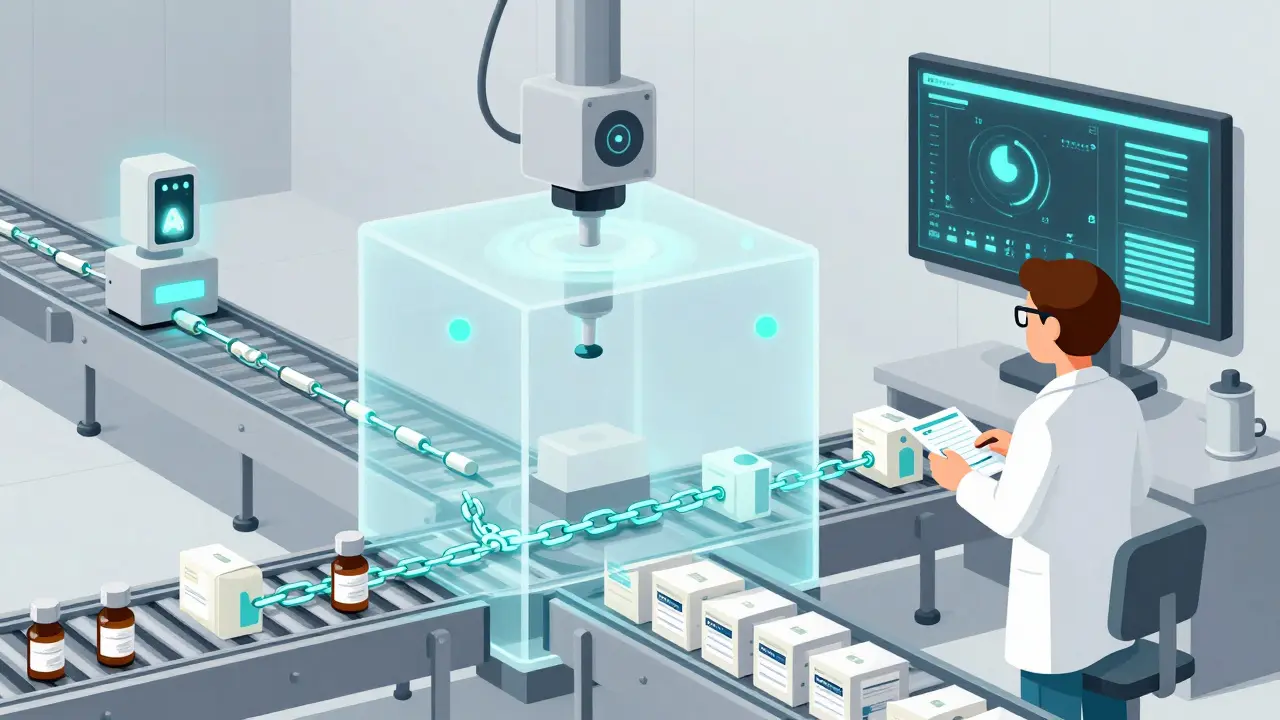
The industry is moving fast. By 2026, 75% of large pharma manufacturers will use AI to predict quality failures before they happen. At Pfizer’s main facility, an AI model now scans production data 17 times per second and flags anomalies that humans would miss. It reduced false halts by 34% and caught real issues 48 hours earlier. Blockchain is also gaining ground. One company now tracks every API shipment from source to final product on a blockchain ledger. If a batch fails, they can trace exactly which supplier, which shift, and which machine was involved-all in under 10 minutes. But there’s a catch. Over-reliance on automation can backfire. A 2023 MIT study found that when factories automated too many quality decisions, minor defects increased by 27%. Human judgment still matters. The best systems combine AI with trained staff who understand context.What Patients and Providers Can Do
Patients can’t fix manufacturing problems-but they can stay informed. The FDA maintains a public Drug Shortages list updated weekly. If your medication is on it, talk to your pharmacist. Often, there’s a therapeutic alternative. Pharmacists and prescribers should track shortages proactively. Many hospitals now use automated alerts tied to the FDA’s database. When a drug is flagged, they switch to backup options before patients run out. And if you’re a healthcare provider, ask your suppliers: “What’s your quality halt protocol?” If they can’t answer clearly, it’s a red flag.The Bottom Line
Drug shortages caused by quality halts aren’t inevitable. They’re the result of systems that prioritize speed over safety-or worse, systems that don’t learn from past mistakes. The technology to prevent them exists. The training is available. The regulations are clear. What’s missing is consistent execution. Every halt should be treated not as a failure, but as a lesson. If we stop treating these shutdowns as emergencies and start treating them as data points, we can build a system that doesn’t just make drugs-but makes them right, every time.Why do drug manufacturing halts take longer than in other industries?
Drug manufacturing halts take longer because they’re governed by strict regulatory protocols. Unlike consumer goods, where a defective product might be pulled from shelves later, pharmaceuticals require immediate isolation of batches, formal reporting to agencies like the FDA, and documented root cause analysis. Regulatory review alone can take 10-20 days. Plus, sterile environments, complex chemistry, and high-stakes safety requirements mean every step must be verified before restarting.
Can AI really prevent drug production halts?
Yes-but not alone. AI models can analyze real-time sensor data to detect subtle anomalies that humans miss, like a 0.3°C temperature drift or a pressure fluctuation that precedes contamination. At Pfizer and Siemens facilities, AI has reduced unnecessary halts by 30-34% and caught true issues 24-48 hours earlier. However, AI still needs human oversight. Too much automation can cause false alarms or ignore context, leading to more defects. The best systems use AI to flag risks, then let trained staff decide whether to halt production.
How do supplier issues cause drug shortages?
Many drugs rely on a single active ingredient made by one overseas supplier. If that supplier has a quality problem-like contamination, equipment failure, or failure to meet cleanliness standards-the entire global supply chain is affected. In 2023, a halt at a single API plant in China caused shortages of 12 different medications in the U.S. because no other supplier could ramp up fast enough. Regulatory delays and long lead times make it hard to switch suppliers quickly, even in emergencies.
What’s stop-work authority, and why does it matter?
Stop-work authority lets any employee-on the line, in QA, or in maintenance-shut down production if they see a quality issue. It removes the need to wait for approval. Companies that use it report 41% fewer recurring quality problems. It works because the people closest to the machines often see problems first. When they’re empowered to act, defects are caught before they become batch-wide failures. It’s not about blame-it’s about safety.
Are drug shortages getting worse?
Yes. The number of drug shortages linked to quality issues has increased 42% since 2020. Factors include aging infrastructure, supply chain fragility, regulatory pressure, and underinvestment in quality systems at mid-sized manufacturers. While large companies are adopting AI and blockchain, many smaller producers still rely on outdated equipment and paper-based logs. Without systemic upgrades, shortages will continue to rise.
What should I do if my medication is on a shortage list?
Don’t stop taking it without talking to your doctor. Contact your pharmacist-they often know about alternative brands or formulations. Many drugs have therapeutically equivalent substitutes. Your provider can also check if a different dosage form (like a liquid instead of a pill) is available. The FDA’s Drug Shortages page lists approved alternatives. Never substitute with unverified sources or overseas suppliers, as quality can’t be guaranteed.
