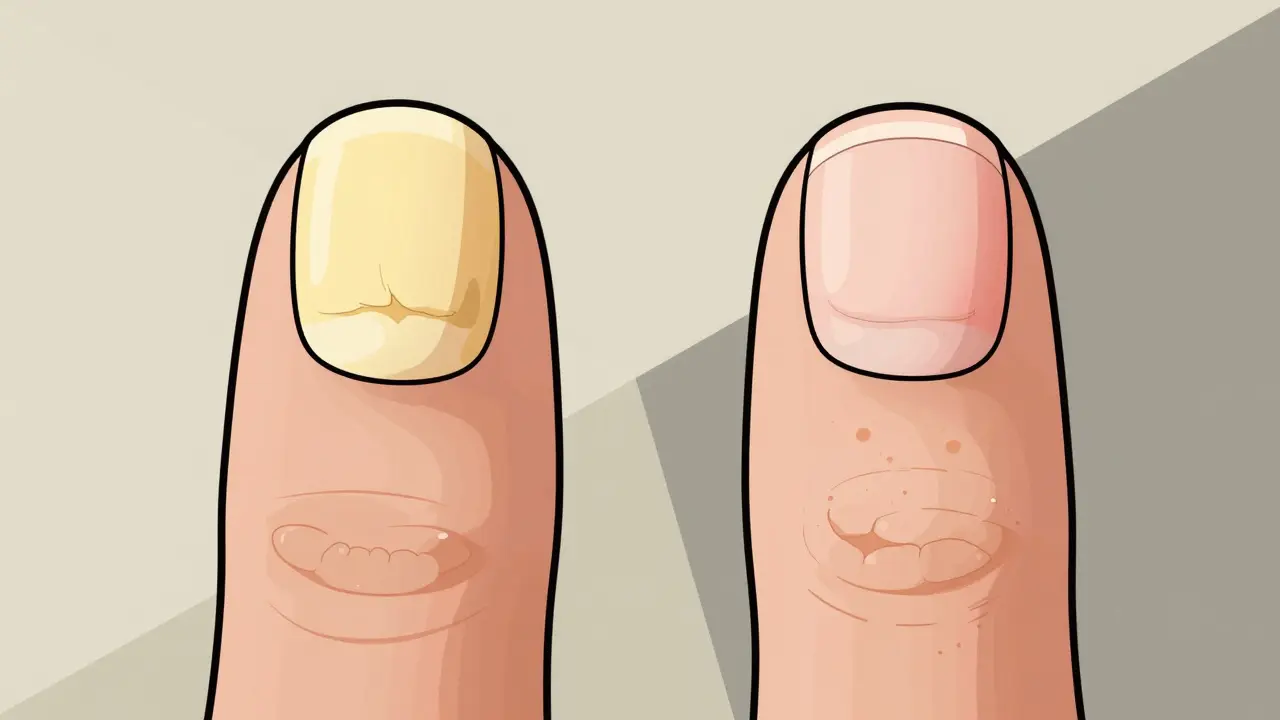
Most people assume that a thick, discolored nail is just a fungal infection. But what if it’s not? What if your nail changes are actually caused by your immune system attacking your own skin? You’re not alone if you’ve spent months treating your nails with antifungal creams - only to see no improvement. Fungal nail infections and nail psoriasis look almost identical to the naked eye. Both cause yellowing, crumbling, and separation from the nail bed. But they’re completely different conditions, and treating them the wrong way can make things worse.
What’s Really Going On With Your Nails?
Fungal nail infections, called onychomycosis, are caused by tiny organisms - usually a type of fungus called Trichophyton rubrum. These invaders live in warm, moist places like locker rooms, public showers, or even your own sweaty shoes. They don’t just sit on the surface. They burrow under your nail, feed on keratin, and slowly take over. The infection starts as a small white or yellow spot near the tip of the nail and creeps toward the cuticle over months. By the time you notice it, the nail is often thickened, brittle, and sometimes smells bad. About 90% of cases turn the nail dark brown or black. The fungus doesn’t care if you’re healthy or not - anyone can get it.
Nail psoriasis, on the other hand, has nothing to do with germs. It’s an autoimmune condition. Your immune system, which normally protects you from infections, mistakenly attacks the nail matrix - the tissue under your cuticle that makes new nail cells. Instead of growing slowly and smoothly over 6 to 12 months, new nail cells form every 3 to 4 days. This rush of cells piles up, distorting the nail’s shape and surface. Nail psoriasis doesn’t appear out of nowhere. Most people who get it already have psoriasis on their skin - often for 10 to 15 years before their nails change. About 80% of people with psoriasis will develop nail symptoms at some point.
Key Differences You Can See at Home
Here’s what sets them apart - and why it matters:
- Nail pitting: Tiny dents in the nail surface, like someone tapped it with a pin. This happens in 70% of nail psoriasis cases. You’ll rarely see this in fungal infections - only about 2% of the time.
- Oil-drop spots: Yellow-brown discolorations that look like a drop of oil trapped under the nail. These are classic for psoriasis and appear in up to half of cases. Fungal infections don’t cause these.
- Foul odor: If your nail smells bad, especially when you trim it, that’s a strong sign of fungus. Psoriasis nails don’t smell. Not even a little.
- How it spreads: Fungal infections usually start on one nail - often a big toe - and spread slowly. Psoriasis often hits multiple nails at once, sometimes all fingers or toes.
- Thickness: Fungal nails get thick - really thick. Often 3 to 5 millimeters. Psoriatic nails thicken too, but usually less - around 2 to 3 millimeters.
One of the most confusing signs is yellowing. About 68% of nail psoriasis cases look just like fungal infections because they turn yellow. That’s why so many people get it wrong.
Why Misdiagnosis Is So Common - and Costly
Even doctors struggle to tell them apart. A 2023 study in JAMA Dermatology found that primary care doctors correctly diagnose these conditions only 52% of the time. Dermatologists get it right 85% of the time - but that still means 1 in 7 patients get the wrong treatment.
What happens when you misdiagnose?
- If you have psoriasis and use antifungal creams, nothing changes. You waste money, time, and hope.
- If you have fungus and get steroid creams (meant for psoriasis), your nail can get even more brittle and start crumbling.
One patient on Reddit said: “I used antifungal treatments for 8 months. My nails got worse. Then I found out it was psoriasis.” Another wrote: “My dermatologist said it was psoriasis, gave me steroids - my nail started falling off.”
The cost of misdiagnosis isn’t just emotional. In the U.S. alone, it leads to about $850 million in wasted healthcare spending each year. That’s because people keep buying antifungals, seeing multiple doctors, and getting unnecessary tests.

How Doctors Actually Diagnose These Conditions
Don’t rely on looks alone. Here’s what real diagnosis looks like:
- Clinical exam: The doctor looks for pitting, oil spots, and whether multiple nails are affected. They check for skin psoriasis elsewhere - elbows, scalp, knees.
- KOH test: A small piece of your nail is scraped off, mixed with potassium hydroxide, and looked at under a microscope. This test finds fungus 70-80% of the time. It’s fast, cheap ($15-$25), and done in the office.
- Fungal culture: If KOH is negative but the doctor still suspects fungus, they send a sample to a lab. This takes weeks but is more accurate - it catches the fungus 95% of the time when it’s there.
- PAS staining: A special dye highlights fungal cells in the nail. It’s 90% sensitive and used when the diagnosis is still unclear.
There’s no single blood test for either condition. Diagnosis is based on signs, tests, and history.
Treatment: What Actually Works
Antifungals won’t fix psoriasis. Steroids won’t kill fungus. Treatment depends entirely on what you have.
For Fungal Nail Infections:
- Oral terbinafine: Taken daily for 6 to 12 weeks (longer for toenails). Clears the infection in about 78% of cases, confirmed by lab tests.
- Topical antifungals: Like efinaconazole (Jublia) or tavaborole (Kerydin). These are applied daily for 48 weeks. They work slowly because nails grow only 0.1mm per day. Good for mild cases or if you can’t take pills.
- Keep nails dry: Fungus thrives in moisture. Wear open shoes, change socks twice a day, use antifungal powder. Humidity below 40% helps prevent recurrence.
For Nail Psoriasis:
- Corticosteroid injections: A tiny shot of steroid right into the nail fold. Shows improvement in 8 to 12 weeks. Reduces swelling and pitting.
- Biologics: Drugs like secukinumab (Cosentyx) or ixekizumab. These target the immune system’s overactive response. In clinical trials, 65% of patients saw major improvement in nail appearance after 24 weeks.
- Emollients: Thick ointments like petroleum jelly applied daily help prevent the nail from lifting away from the bed.
- Avoid trauma: Don’t bite your nails, don’t cut them too short, don’t use harsh chemicals. Injury can trigger worse flare-ups - a phenomenon called the Koebner effect.
What You Can Do at Home
Whether you have fungus or psoriasis, these steps help:
- Take a photo of your nails every month. Use the same lighting and angle. This helps you and your doctor see if things are improving or getting worse.
- Keep your nails trimmed short. Long nails trap more moisture and debris.
- Wear breathable footwear. Avoid tight shoes that crush your toes.
- Don’t share nail clippers or files. Fungus spreads easily.
- If you get a manicure or pedicure, bring your own tools. Salons can be hotspots for fungal spread.
What’s Next? New Science on the Horizon
Research is moving fast. In 2023, Mayo Clinic tested a new tool called reflectance confocal microscopy - a non-invasive scanner that looks at the nail in real time. It correctly told psoriasis and fungus apart in 92% of cases.
Scientists are also studying the microbiome - the tiny bacteria and fungi living on your nails. Early findings show psoriasis nails have more Staphylococcus and less Cutibacterium, while fungal nails are loaded with Trichophyton DNA. In the next few years, a simple swab test might replace invasive scrapings.
Artificial intelligence is being trained to analyze nail photos. The Global Psoriasis Atlas predicts a 22% drop in misdiagnosis by 2027 thanks to AI tools that spot patterns humans miss.
And climate change? It’s making things worse. Warmer, wetter weather is expanding where fungi can live. The International Society for Human and Animal Mycology expects a 15% rise in fungal nail infections over the next decade.
Bottom Line: Don’t Guess - Get Tested
If your nails look strange, don’t assume it’s fungus. Don’t self-treat with over-the-counter creams. Don’t wait months to see if it gets better. See a dermatologist. Ask for a KOH test. Bring photos of your nails over time. If you have psoriasis elsewhere on your body, mention it - even if it’s mild.
Getting the right diagnosis means you stop wasting time and money. You start treating the real problem. And your nails? They’ll finally start to heal.
Can nail psoriasis turn into a fungal infection?
Yes - and it’s more common than you think. Nail psoriasis damages the nail structure, creating cracks and gaps where fungus can sneak in. Between 4.6% and 30% of people with nail psoriasis end up with a secondary fungal infection. That’s why doctors always test for fungus first, even if they suspect psoriasis.
Are over-the-counter antifungals effective for nail psoriasis?
No. Over-the-counter antifungal creams, sprays, or nail polishes won’t help nail psoriasis because the root cause isn’t fungus - it’s your immune system. Using them can delay proper treatment and make your nails worse over time by drying them out or causing irritation.
How long does it take to see improvement with treatment?
It depends. For fungal infections, oral antifungals like terbinafine can show results in 2 to 3 months, but full nail regrowth takes 6 to 12 months because nails grow slowly. For nail psoriasis, steroid injections may improve pitting and thickening in 8 to 12 weeks. Biologics take longer - around 24 weeks - but offer deeper, lasting improvement.
Can I prevent nail psoriasis or fungal infections?
You can’t prevent psoriasis - it’s genetic and autoimmune. But you can reduce flare-ups by managing stress, avoiding trauma to your nails, and using moisturizers. For fungal infections, prevention is easier: keep feet dry, wear sandals in public showers, don’t share nail tools, and change socks daily. Moisture control is your best defense.
Is it possible to have both conditions at the same time?
Absolutely. In fact, it’s not rare. People with nail psoriasis are more likely to develop fungal infections because their nails are already damaged. Doctors call this a “superinfection.” That’s why testing for both is critical - treating just one won’t fix the problem if both are present.

Manan Pandya
December 30, 2025 AT 02:49Great breakdown. I’ve been dealing with this for years and the KOH test was the only thing that finally clarified things. No more guessing games.
Aliza Efraimov
December 31, 2025 AT 12:02I spent $400 on antifungal nail polish for 8 months thinking it was fungus. My dermatologist finally did a biopsy and said it was psoriasis. I cried. Not because it was bad news-but because I finally understood why nothing worked. This post saved me another year of frustration.
Nisha Marwaha
January 1, 2026 AT 22:32From a dermatological perspective, the differential diagnosis between onychomycosis and nail psoriasis hinges on histopathological and microbiological corroboration. The presence of parakeratosis and nail matrix hyperproliferation is pathognomonic for psoriatic etiology, whereas hyphae or fungal spores in PAS-stained sections confirm mycosis. Clinical correlation with cutaneous psoriatic plaques remains indispensable, but advanced modalities like reflectance confocal microscopy are rapidly redefining diagnostic paradigms.
Paige Shipe
January 3, 2026 AT 17:26So people just buy drugstore crap and think it’ll fix their nails? That’s why medicine is broken. You need a real doctor. Not some guy on Reddit telling you to soak your feet in vinegar.
Kevin Lopez
January 3, 2026 AT 22:18Biologics > antifungals for psoriasis. Case closed.
Amy Cannon
January 5, 2026 AT 16:02It is of paramount importance to underscore, with the utmost gravity and solemnity, that the misapplication of topical antifungal agents in the context of autoimmune nail dystrophy not only constitutes a therapeutic misstep of considerable magnitude, but also represents a profound failure in patient education, which, in turn, perpetuates a cycle of iatrogenic exacerbation and economic waste on a scale that is, frankly, unconscionable. One must not underestimate the gravity of this diagnostic conundrum, which, in my professional estimation, is emblematic of a broader systemic deficiency in primary care dermatology training.
Jasmine Yule
January 6, 2026 AT 06:53Thank you for writing this. I’ve been too scared to see a doctor because I thought I’d be judged for not taking better care of my nails. This made me feel seen. I’m booking an appointment tomorrow.
Greg Quinn
January 7, 2026 AT 04:35It’s funny how we treat symptoms like they’re the enemy, when really they’re just the messenger. Your nails are screaming for you to listen. The real question isn’t fungus or psoriasis-it’s what’s going on inside you that made your body react this way.
Lisa Dore
January 7, 2026 AT 14:59I’ve been sharing this with my nail tech friends-now they know to ask clients about skin conditions before doing a pedicure. Small changes, big impact. Keep spreading awareness like this!
Sharleen Luciano
January 9, 2026 AT 05:59Anyone who relies on over-the-counter treatments without a confirmed diagnosis is either dangerously naive or willfully ignorant. This isn’t a beauty blog-it’s a clinical dilemma requiring laboratory validation. If you don’t have the patience for a KOH test, you shouldn’t be self-diagnosing. Period.