When a medical device quality control system is properly implemented, it prevents dangerous defects before they reach patients. Imagine a pacemaker or an insulin pump made in a factory. How do we know it's safe? It's not luck-it's a system of strict standards that every manufacturer must follow. The FDA estimates these systems prevent about 30% of potential device failures that could otherwise harm patients. Let's break down how these standards work in practice.
The Foundation of Medical Device Safety
The Quality System Regulation (QSR) is a set of FDA regulations (21 CFR Part 820) that outline requirements for medical device manufacturing quality systems has evolved significantly. Originally introduced in 1978 as Good Manufacturing Practices (GMPs), it became formalized in 1996. In January 2024, the FDA issued a final rule to harmonize with ISO 13485:2016 the international standard for medical device quality management systems. This change means U.S. manufacturers now follow the same global standard used in the EU and other regions, reducing duplication and improving consistency.
The FDA's Quality Management System Regulation (QMSR) Final Rule became effective February 2, 2026. It eliminates about 30% of redundant documentation requirements for multinational manufacturers. Before this, U.S. companies needed dual compliance systems for domestic and international markets. Now, one system meets both requirements.
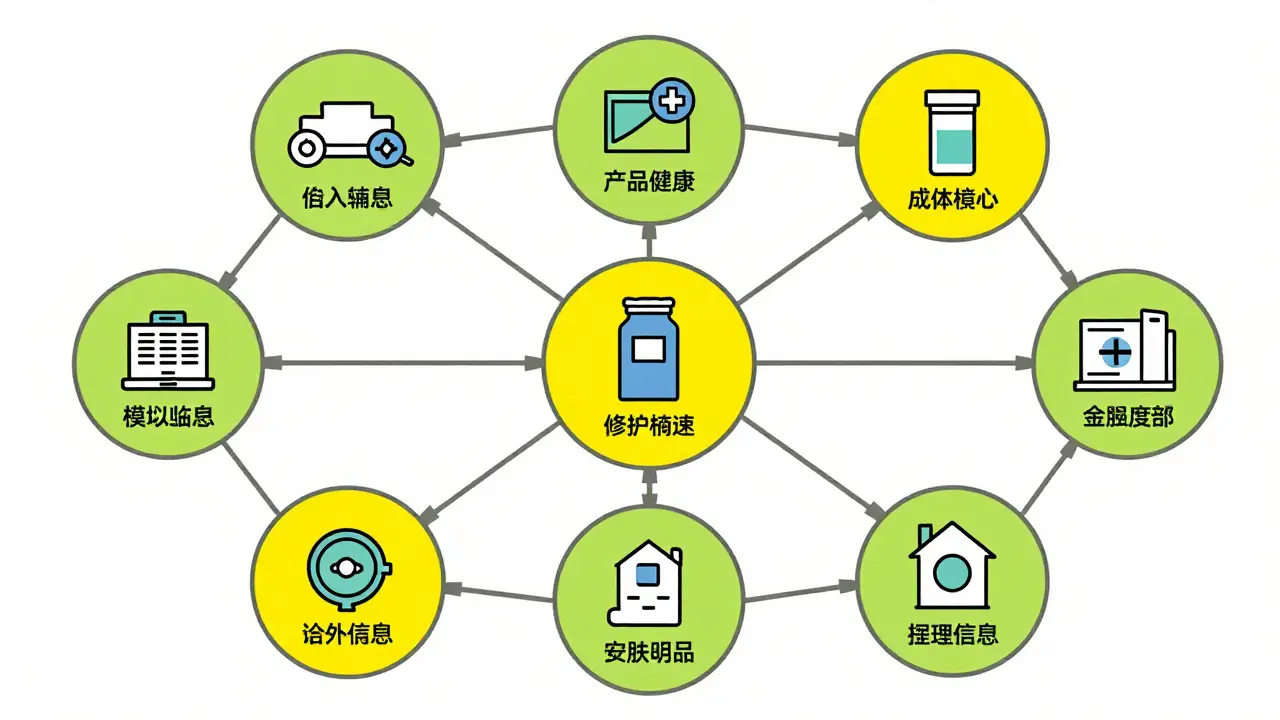
Key Components of Quality Control Systems
| Component | Description | Impact |
|---|---|---|
| Traceability Matrices | Links design inputs to final product features | Prevents recalls by identifying affected devices quickly |
| Risk Management (ISO 14971) | Documents hazards and mitigation strategies | Reduces potential defects by 30% |
| IEC 60601-1 Testing | Electrical safety standards for devices | Ensures 1,500-volt dielectric strength and safe leakage current |
| Statistical Process Control (SPC) | Monitors production variables with data | Reduces errors by up to 45% |
| Corrective and Preventive Action (CAPA) | Systematically fixes and prevents issues | Reduces repeat problems by 50% |
Traceability matrices are crucial. They connect every design input to the final product's features. When a software change in an insulin pump was discovered to be unvalidated, traceability matrices helped identify the issue before 5,000 devices reached patients. Without this system, those devices might have been implanted in patients, causing serious harm.
For electrical devices, IEC 60601-1 a safety standard for medical electrical equipment requires dielectric strength tests of at least 1,500 volts and leakage current limits of 100 microamperes. These tests ensure devices won't shock patients during use. Companies like Domico Med-Device report that standard operating procedures (SOPs) reduce error risks by up to 45%.
Real-World Impact: Preventing Harm Before It Happens
A Director of Quality at a Class III device manufacturer shared how traceability matrices prevented a potential Class I recall. They identified an unvalidated software change affecting 5,000 implanted devices. This example shows how quality control isn't just paperwork-it's lifesaving.
Similarly, when a supplier's component failed testing, traceability allowed the manufacturer to quarantine all affected devices before distribution. This prevented a widespread issue that could have led to patient injuries. The Association for the Advancement of Medical Instrumentation (AAMI) found facilities with mature quality systems achieved 99.97% first-pass yield rates versus 98.2% for minimal compliance-17 times fewer defects.
Challenges and Solutions
Implementing these systems isn't easy. Quality managers report that 68% spend too much time on paperwork instead of improving processes. FDA warning letters often cite supplier audit failures-41% of 2023 letters mentioned this issue. Integrating legacy equipment with modern quality systems is another challenge. 57% of manufacturers struggle with pre-2010 machines connecting to digital platforms.
Solutions exist. Greenlight Guru's QMS software, used by 147 verified medical device users, has a 4.7/5 rating for its FDA-specific templates. It helps reduce audit failures by 32%. Corrective and Preventive Action (CAPA) systems address problems systematically. When an issue arises, CAPA ensures it's fixed and prevented from recurring. This reduces repeat problems and builds trust in the manufacturing process.
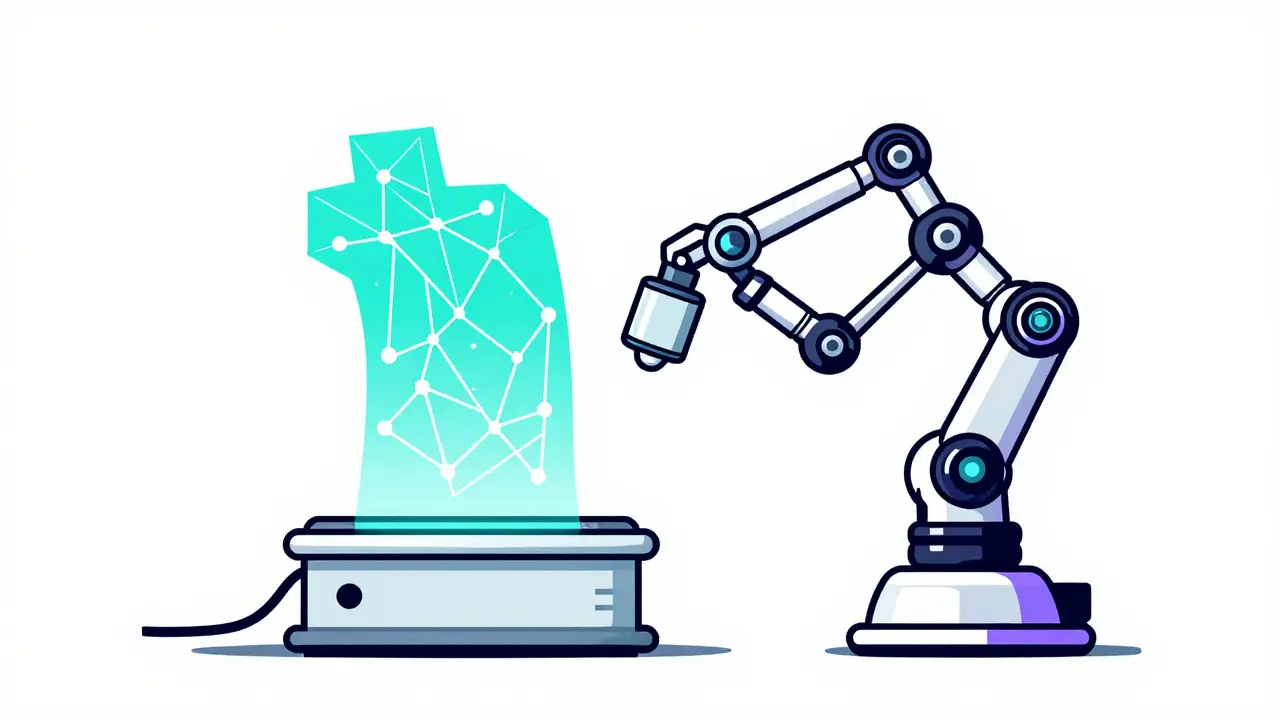
The Future of Medical Device Safety
Artificial intelligence is transforming quality control. Early adopters report 25-40% fewer defects using machine learning to analyze production data. Gartner predicts 60% of medical device quality systems will use AI-driven analytics by 2027, cutting human error by up to 50%.
Cybersecurity is also becoming part of quality standards. Draft ISO 13485:202X updates will address software-as-a-medical-device (SaMD) requirements. This is crucial as more devices connect to networks. The FDA's transition to ISO 13485:2016 saves the industry $400 million annually in compliance costs while keeping patients safe. This harmonization shows how global cooperation strengthens medical device safety.
What is ISO 13485:2016?
ISO 13485:2016 is the international standard for medical device quality management systems. It covers design, development, production, and distribution of medical devices. The standard requires risk management, traceability, and strict documentation. In 2024, the FDA harmonized its regulations with ISO 13485:2016, making it the global benchmark for medical device safety.
How do traceability matrices prevent recalls?
Traceability matrices link every design input to the final product's features. When an issue arises, manufacturers can quickly identify all affected devices. For example, when an unvalidated software change was found in an insulin pump, traceability matrices pinpointed exactly which 5,000 devices were impacted. This allowed immediate quarantine before distribution, preventing a potential Class I recall.
What are the biggest challenges in implementing quality control?
The biggest challenges include excessive paperwork (68% of quality managers report this), integrating legacy equipment (57% struggle with pre-2010 machines), and supplier oversight failures (41% of FDA warning letters cite this). Smaller manufacturers face greater resource constraints, making compliance harder without dedicated quality teams.
How does AI improve medical device quality control?
AI analyzes production data to predict defects before they occur. Early adopters report 25-40% reductions in defect rates by spotting patterns humans miss. For example, machine learning can monitor temperature fluctuations in sterilization processes and adjust parameters in real-time. Gartner predicts 60% of medical device quality systems will incorporate AI analytics by 2027, reducing human error by up to 50%.
Why is supplier quality oversight important?
41% of FDA warning letters in 2023 cited failures in supplier auditing. A single faulty component from a supplier can cause widespread recalls. For example, contaminated raw materials led to a 2022 recall of 100,000 surgical tools. Rigorous supplier audits ensure components meet specifications before they enter production. This prevents cascading failures that endanger patients.

Pamela Power
February 5, 2026 AT 21:52The FDA's 'harmonization' with ISO 13485:2016 is a joke. Real quality isn't about paperwork-it's about actual testing. I've seen manufacturers cut corners, and this 'reduction' in documentation? More like a loophole for negligence. What's next? Abolishing all safety checks? Pathetic.
anjar maike
February 6, 2026 AT 14:26Interesting point 🤔 ISO 13485 helps reduce errors traceability matrices example cool 🔍
Sam Salameh
February 7, 2026 AT 20:19American-made medical devices are the gold standard. FDA regulations ensure top-notch quality. We lead the world in innovation and safety. Proud to be part of this industry.
Joyce cuypers
February 9, 2026 AT 19:01totally agree! but i think the real magic is in the traceability matrices. they saved 5000 devices from being recalled. typos happen but the system works 😊
Carol Woulfe
February 10, 2026 AT 01:48ISO 13485:2016 harmonization? More like a Trojan horse. The FDA and big pharma are colluding to dismantle safety protocols. The 2022 surgical tool recall was no accident-it was engineered. They want you to believe this 'harmonization' is beneficial, but it's a trap. I've seen the data.
Jenna Elliott
February 11, 2026 AT 10:26American devices are best FDA rules keep us safe No need for EU nonsense Our system works better
Elliot Alejo
February 12, 2026 AT 01:43Agreed on American standards but global collaboration is key. ISO 13485:2016 helps align practices worldwide. It's not about competition but safety for all patients.
Danielle Vila
February 13, 2026 AT 03:34Global collaboration? More like a conspiracy to undermine US sovereignty. ISO standards are designed to let foreign manufacturers cut corners. The FDA's move is a surrender. We should enforce strict US-only standards. I've studied this for years and know the truth.
Thorben Westerhuys
February 15, 2026 AT 00:55Carol is absolutely right! The FDA's 'harmonization' is a disaster! It's a complete betrayal of patient safety! And the ISO 13485:2016? It's a tool for corporate greed! The 2022 recall was inevitable! We need to expose this immediately! It's all connected! There's no doubt!
Laissa Peixoto
February 15, 2026 AT 12:57Medical device safety isn't just about regulations-it's a balance between innovation and precaution. The traceability matrices example shows how systematic thinking prevents harm. But we must also consider the human element in quality control. True safety comes from empathy as much as protocols. Manufacturers often focus on meeting standards, but forget the patient's perspective. Every device is someone's lifeline. A failure isn't just a statistic-it's a life. The FDA's harmonization with ISO 13485:2016 is a step forward, but not enough. We need more transparency in supplier audits. The 41% of FDA warning letters citing supplier failures prove that. AI can help predict defects, but it's not a silver bullet. Human oversight is irreplaceable. We must invest in training quality control teams. It's not just about technology-it's about culture. Every employee must feel responsible for patient safety. Only then can we truly prevent harm.