
Have you ever filled a prescription for liquid antibiotics for your child, only to be told you have to throw it away after 10 or 14 days-even if there’s still medicine left? It feels wasteful. It feels confusing. And if you’ve ever used it past that date because "it still looks fine," you’re not alone. But here’s the hard truth: liquid antibiotics don’t last like pills. They break down fast. And using them after they’ve degraded isn’t just ineffective-it can be dangerous.
Why Liquid Antibiotics Don’t Last
Unlike tablets or capsules, liquid antibiotics are mixed with water right before you use them. This is done mostly for kids who can’t swallow pills. But mixing powder with water starts a clock ticking. The active ingredients, especially in beta-lactam antibiotics like amoxicillin and ampicillin, are chemically unstable in water. They start breaking down the moment they’re reconstituted. This isn’t a flaw-it’s science. The molecules that kill bacteria are designed to be reactive. In water, they react with moisture and slowly fall apart.
Studies show that once mixed, these suspensions lose potency over time. The FDA and USP require manufacturers to prove their product stays at least 90% potent until the expiration date printed on the bottle. But that date isn’t printed when the medicine is made-it’s printed after it’s mixed. And that date is short. Why? Because the science says so. No one wants to give someone medicine that’s 30% weaker than it should be. That’s not just a waste-it can lead to treatment failure, antibiotic resistance, or worse.
Amoxicillin vs. Amoxicillin/Clavulanate: A Big Difference
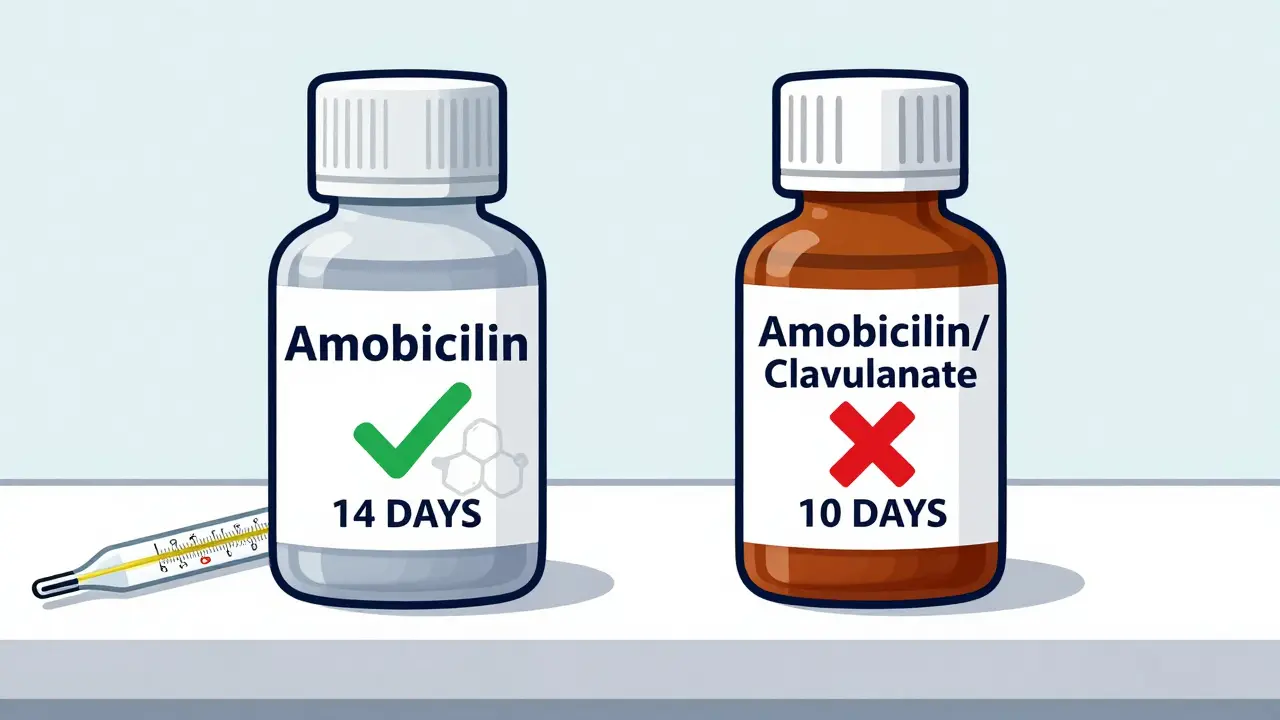
Not all liquid antibiotics expire at the same time. Amoxicillin alone? It’s fairly stable. When refrigerated (between 2°C and 8°C), it keeps at least 90% of its strength for up to 14 days. That’s why many doctors prescribe 14-day courses for ear infections or sinusitis.
But add clavulanate-another ingredient that blocks bacteria from resisting amoxicillin-and everything changes. The combination, sold under names like Augmentin, breaks down much faster. Refrigerated, it only lasts 10 days. At room temperature? Just 5 days. Why? Because clavulanate is even more fragile than amoxicillin. It degrades quickly, especially if the medicine is poured into an oral syringe. One study found clavulanate’s stability dropped from 11 days in the original bottle to under 5 days in a syringe, even when kept cold.
So if your child’s prescription says 14 days but the pharmacy says throw it out after 10, they’re not being overcautious-they’re following the data. The clavulanate is the weak link.
Storage Matters More Than You Think
Temperature is the biggest factor in how long your liquid antibiotic lasts. Every 10°C increase in storage temperature roughly doubles how fast the medicine breaks down. That’s called the Arrhenius effect, and it’s been proven over and over in labs.
Refrigeration (2-8°C) is the gold standard. But many people leave the bottle on the counter. If you do, you cut the shelf life in half. Amoxicillin that should last 14 days? Now it’s good for only 5-7. Amoxicillin/clavulanate? Gone in 2-3 days.
Light and air also matter. Clear bottles exposed to sunlight can speed up degradation. Transferring the medicine to another container-like a plastic cup or syringe-can expose it to more air and contaminants. Some studies show this alone can reduce stability by 30% or more.
Freezing? It sounds like a smart workaround. And it works. Studies from the 1970s showed amoxicillin kept 88% of its potency for 60 days at -10°C. But freezing isn’t recommended. Why? Because when you thaw it, the medicine can separate or become clumpy. The particles might not re-suspend evenly, meaning your child gets too much or too little with each dose. Plus, not all formulations are designed for freezing. The label says “refrigerate,” not “freeze.” Stick to the instructions.
What Happens When It Goes Bad?
You might think, “It still smells fine. It still looks clear. Why can’t I use it?” But degradation isn’t always visible. You won’t see mold or weird colors every time. Sometimes, the medicine just becomes weaker. That’s the real danger.
If the antibiotic isn’t strong enough, it won’t kill all the bacteria. The survivors? They adapt. They become resistant. That’s how superbugs form. You’re not just wasting medicine-you’re making future infections harder to treat.
Some signs of degradation: cloudiness, unusual odor, clumps, or a strange taste. But don’t wait for those. If it’s past the discard date on the label, throw it away. No exceptions.
Real-World Problems: Parents, Pharmacists, and the 14-Day Gap
Here’s the messy reality: prescriptions often call for 10-14 days of treatment. But the liquid suspension expires in 10. That means parents are forced to throw out medicine before the course is done. One parent on a health forum said their child’s infection wasn’t fully treated because they had to toss the bottle on day 10, even though the doctor ordered 14 days.
Pharmacists see this all the time. Many patients return with half-used bottles, scared they’re doing something wrong. Others accidentally use expired medicine because they forgot the date. One survey found 22% of patients have used liquid antibiotics past their discard date.
It’s a system mismatch. The science says 10 days. The medical need says 14. The solution? Better labeling. Pharmacists now write the discard date right on the bottle when they mix it. Some pharmacies use apps that send text reminders: “Your amoxicillin expires tomorrow.” CVS reported an 18% drop in expired medicine use after rolling out this system.

What’s Next? New Tech on the Horizon
The industry knows this is a problem. New formulations are being tested. One 2021 study used microencapsulation to extend amoxicillin/clavulanate stability to 21 days under refrigeration. Pfizer’s upcoming “AmoxiClick” system-set to launch in 2024-keeps the powder and liquid separate until you press a button. Once mixed, it claims 30 days of stability. That’s a game-changer.
But for now, the rules stay the same. Until these new products are widely available, we’re stuck with short shelf lives. And that’s not going to change soon. The chemistry of beta-lactams in water hasn’t been solved. It’s just too unstable.
What You Should Do
- Write the discard date on the bottle the day you mix it. Don’t rely on memory.
- Store it in the fridge at 2-8°C. Never leave it on the counter.
- Don’t transfer it to syringes or cups unless you have to. If you do, use it within 24 hours.
- Check the label. Amoxicillin alone? 14 days refrigerated. Amoxicillin/clavulanate? 10 days.
- If you’re unsure, call your pharmacy. They can tell you exactly how long yours lasts.
- When in doubt, throw it out. Better safe than risking treatment failure or resistance.
Antibiotics are powerful. But they’re not magic. Their strength depends on how you handle them. The short shelf life isn’t a bug-it’s a feature of science. Respect it.
How long does liquid amoxicillin last after being mixed?
When stored in the refrigerator (between 2°C and 8°C), liquid amoxicillin typically remains stable for up to 14 days. At room temperature (above 25°C), its shelf life drops to just 5-7 days. Always check the label on your prescription bottle-some formulations may vary.
Why does amoxicillin/clavulanate expire faster than plain amoxicillin?
The clavulanate component is chemically unstable in water and degrades much faster than amoxicillin. While amoxicillin can last 14 days refrigerated, clavulanate loses potency after just 10 days under the same conditions. This is why combination products like Augmentin have shorter expiration dates. Even storing the medicine in an oral syringe can reduce its stability further.
Can I freeze liquid antibiotics to make them last longer?
While freezing can technically extend shelf life-some studies show up to 60 days of stability at -20°C-it’s not recommended. Freezing can cause the medicine to separate or form clumps. When thawed, it may not mix evenly, leading to inconsistent dosing. Always follow the manufacturer’s storage instructions: refrigerate, don’t freeze.
What happens if I use expired liquid antibiotics?
Using expired liquid antibiotics won’t make you sick directly, but it may not work. The medicine loses potency over time, meaning it won’t kill all the bacteria. This can lead to incomplete treatment, recurring infections, and the development of antibiotic-resistant bacteria. Never use medicine past its discard date.
How do I know if my liquid antibiotic has gone bad?
Signs of degradation include cloudiness, unusual color changes, strange odor, or visible clumps. But don’t wait for these signs-many degraded antibiotics look and smell normal. If it’s past the discard date on the label, throw it away. Visual inspection isn’t reliable.
For parents and caregivers: the goal is to get the full course of antibiotics in. If the bottle expires before the treatment ends, call your pharmacy. They can often provide a new bottle without a new prescription. Don’t risk your child’s health by stretching out an expired dose.

Daniel Dover
February 16, 2026 AT 02:48Store it right. Use it fast. Don't gamble with your kid's health.
Josiah Demara
February 16, 2026 AT 09:27Newsflash: degradation isn't visible until it's too late. You're not saving money-you're breeding superbugs. Congrats.
Erica Banatao Darilag
February 17, 2026 AT 16:55Charlotte Dacre
February 18, 2026 AT 14:40At least the pharmacy labels now say 'DISCARD AFTER 10 DAYS' in neon pink. Progress?
Mandeep Singh
February 19, 2026 AT 16:48Mike Hammer
February 20, 2026 AT 09:46Kapil Verma
February 20, 2026 AT 10:31Kaye Alcaraz
February 22, 2026 AT 04:11Many parents don’t realize how quickly these suspensions degrade. I always write the discard date on the bottle with a Sharpie and set a phone reminder. Small habits save big risks. Keep sharing this kind of info-it makes a difference.
Joe Grushkin
February 23, 2026 AT 02:24Esha Pathak
February 24, 2026 AT 15:42Amoxicillin breaks down because all things must return to their base state. The bottle, the child, the doctor, the pharmacist-we are all just nodes in a transient reaction. The 10-day limit is not a rule. It is a whisper from entropy itself.
And yet... we still try to control it. How beautiful. How tragic.
Virginia Kimball
February 25, 2026 AT 17:24Also-CVS’s text reminder system? GENIUS. All pharmacies should do this. Seriously.
Michael Page
February 26, 2026 AT 00:00Betty Kirby
February 26, 2026 AT 03:20Kaye Alcaraz
February 27, 2026 AT 07:00