Introduction to Imipramine and Urinary Retention
As a blogger, I have come across many health issues that require attention, and one such issue is the relationship between imipramine and urinary retention. Imipramine is a tricyclic antidepressant (TCA) that has been widely prescribed for the treatment of depression, panic disorders, and even bedwetting in children. However, it is important to understand that this medication can sometimes lead to urinary retention, which is the inability to completely empty the bladder. In this article, I will discuss the causes, treatment, and prevention tips for urinary retention associated with imipramine use.
Understanding Imipramine: Its Uses and Side Effects
Imipramine is a medication that belongs to a class of drugs known as tricyclic antidepressants (TCAs). It works by increasing the levels of certain chemicals in the brain, such as serotonin and norepinephrine, which helps to improve mood, reduce anxiety, and alleviate symptoms of depression. Imipramine is commonly prescribed to treat depression, panic disorders, and enuresis (bedwetting) in children who are over six years old. However, it is essential to be aware of the possible side effects associated with imipramine use.
Some common side effects of imipramine include dry mouth, dizziness, drowsiness, constipation, and blurred vision. More serious side effects can include heart palpitations, seizures, and urinary retention. If you experience any of these serious side effects, it is crucial to contact your healthcare provider immediately.
How Imipramine Can Cause Urinary Retention
Urinary retention, or the inability to completely empty the bladder, can occur as a side effect of imipramine use. This happens because imipramine has anticholinergic properties, which means that it can block the action of a neurotransmitter called acetylcholine. Acetylcholine is responsible for regulating the contraction and relaxation of the smooth muscles in the bladder and urinary tract.
When imipramine blocks the action of acetylcholine, it can lead to a relaxation of the bladder muscles, making it difficult for the bladder to contract properly and expel urine. This can result in urinary retention and can become a serious issue if not addressed promptly.
Recognizing the Symptoms of Urinary Retention
It is crucial to recognize the signs and symptoms of urinary retention if you are taking imipramine, as early detection can help prevent complications. Some common signs and symptoms of urinary retention include:
- Difficulty starting a urine stream
- Weak or interrupted urine flow
- A feeling of incomplete bladder emptying
- Frequent urination or an urgent need to urinate
- Pain or discomfort in the lower abdomen
- In severe cases, an inability to urinate at all
If you are experiencing any of these symptoms while taking imipramine, it is important to consult your healthcare provider as soon as possible.
Treatment Options for Imipramine-Induced Urinary Retention
If you are experiencing urinary retention due to imipramine use, your healthcare provider may recommend several treatment options. These may include:
- Discontinuing or reducing the dose of imipramine: In some cases, stopping the medication or lowering the dosage may help alleviate urinary retention symptoms.
- Switching to a different medication: If discontinuing imipramine is not an option, your healthcare provider may recommend switching to a different antidepressant with fewer anticholinergic side effects.
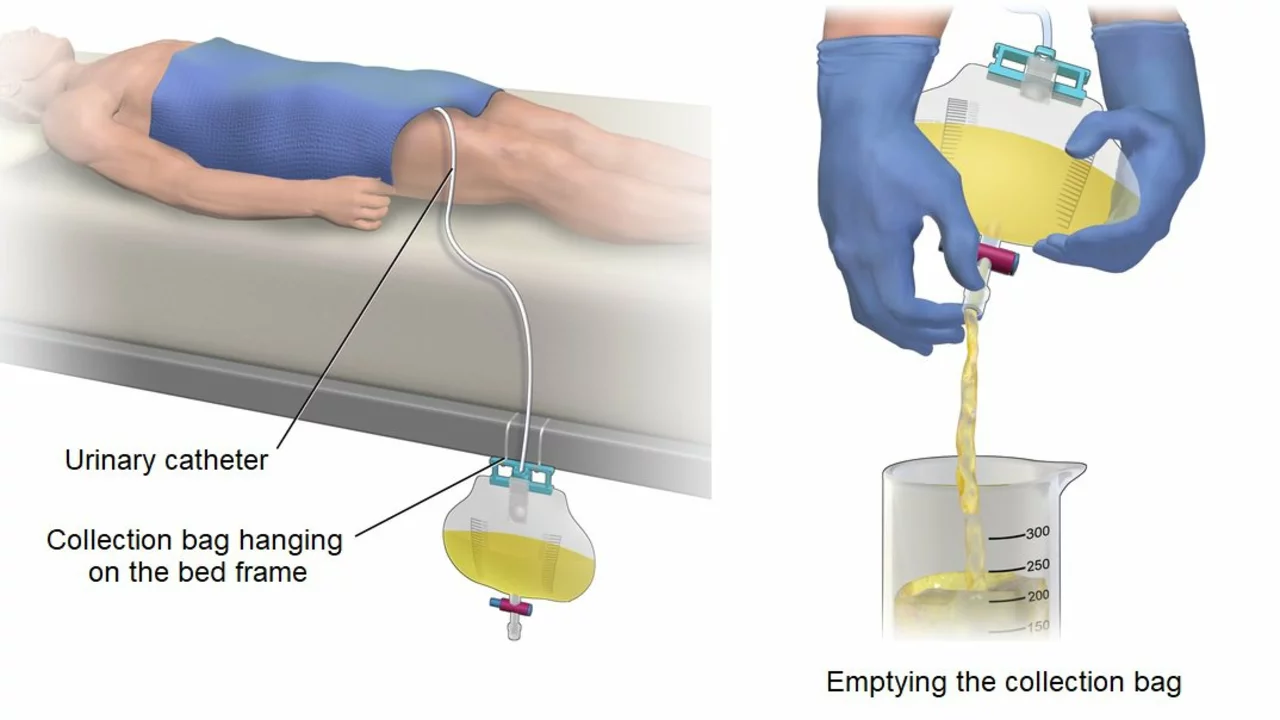
- Catheterization: In severe cases, a catheter may be inserted into the bladder to help drain the urine.
- Medications: Your healthcare provider may prescribe medications that can help relax the bladder muscles and improve urine flow.
It is important to work closely with your healthcare provider to determine the best treatment option for your individual situation.
Prevention Tips for Imipramine-Induced Urinary Retention
While it may not be possible to completely prevent urinary retention caused by imipramine, there are several steps you can take to minimize your risk. Some prevention tips include:
- Discussing your medical history with your healthcare provider: Be sure to inform your healthcare provider about any previous instances of urinary retention or other urinary problems before starting imipramine therapy.
- Staying well-hydrated: Drinking plenty of water can help promote healthy urinary function and may reduce the risk of urinary retention.
- Practicing good bladder habits: Try to urinate regularly and avoid holding in urine for long periods of time.
- Avoiding caffeine and alcohol: Both of these substances can irritate the bladder and may increase the risk of urinary retention.
Monitoring Your Urinary Health While Taking Imipramine
It is important to closely monitor your urinary health while taking imipramine to ensure that any potential issues are detected and addressed promptly. Some ways to monitor your urinary health include:
- Regularly assessing your urinary symptoms: Keep track of any changes in your urinary habits, such as difficulty starting a urine stream or a feeling of incomplete bladder emptying.
- Staying in touch with your healthcare provider: Make sure to attend all scheduled appointments and discuss any concerns or changes in symptoms with your healthcare provider.
- Being proactive about seeking treatment: If you experience any symptoms of urinary retention, contact your healthcare provider immediately to discuss treatment options.
Conclusion: Balancing the Benefits and Risks of Imipramine Use
Imipramine can be a highly effective treatment for depression, panic disorders, and enuresis in children. However, it is essential to be aware of the potential side effects, including urinary retention. By understanding the causes, recognizing the symptoms, and following prevention and treatment strategies, you can minimize your risk of urinary retention and maintain your overall urinary health while benefiting from the therapeutic effects of imipramine.

Keri Shrable
April 29, 2023 AT 03:37I’ve seen patients on imipramine who suddenly start complaining about a “full bladder” feeling and it can be pretty alarming. The anticholinergic kick of the drug really does mess with the smooth muscle tone in the urinary tract. Staying hydrated and keeping a regular bathroom schedule can sometimes offset the grip it has. Keep an eye on any changes and chat with your doc early.
Destiny Hixon
May 8, 2023 AT 16:57Who even trusts foreign meds when they mess up your flow?
mike brown
May 18, 2023 AT 06:17Honestly, the side‑effects list reads like a horror novel-why bother with something that could tie you up?
shawn micheal
May 27, 2023 AT 19:37It’s easy to forget that the brain‑blessing of imipramine comes with a price tag paid by the bladder. The drug’s anticholinergic nature relaxes the detrusor muscle, making it shy about contracting. If you notice a hesitancy to start urinating, that’s a red flag worth noting. A simple trick is to set a timer for bathroom breaks-don’t wait for the urge to build. Also, limiting caffeine and alcohol can keep the bladder from getting too irritated. Talk to your prescriber about dose adjustments before you self‑diagnose.
Stephen Jahl
June 6, 2023 AT 08:57From a pharmacodynamic perspective, the imipramine molecule exerts a high affinity for muscarinic acetylcholine receptors, thus engendering a pronounced anticholinergic syndrome. This syndrome manifests not only as xerostomia and blurred vision but also precipitates a cascade culminating in urinary retention. The detrusor muscle, reliant upon cholinergic stimulation for appropriate contractility, becomes hypo‑responsive. In the absence of adequate parasympathetic tone, the internal sphincter may remain tonically contracted, obstructing urine outflow. Clinically, patients present with incomplete voiding, post‑void residuals, and, occasionally, suprapubic discomfort. The pathophysiological substrate is further complicated by the drug’s potential to induce sedation, which can diminish the patient’s conscious drive to initiate micturition. Consequently, a multidisciplinary approach is warranted-urologists, psychiatrists, and primary care physicians must collaborate to calibrate therapeutic regimens. Dose tapering, substitution with agents of lower anticholinergic burden (such as selective serotonin reuptake inhibitors), or the use of adjunctive antimuscarinic antagonists may ameliorate symptoms. Moreover, intermittent self‑catheterization can serve as a temporizing measure pending pharmacologic optimization. It is imperative to monitor serum drug concentrations where feasible, as elevated levels correlate with heightened adverse effect profiles. In addition to pharmacologic strategies, behavioral modifications-fluid intake timing, bladder training, and pelvic floor physiotherapy-constitute non‑pharmacologic adjuncts. Ultimately, the clinician’s vigilance in recognizing early urinary complaints can forestall complications such as hydronephrosis or chronic bladder dysfunction. The balance between neuropsychiatric benefit and urologic risk remains a nuanced clinical decision, necessitating individualized assessment.
gershwin mkhatshwa
June 15, 2023 AT 22:17That was a solid rundown, thanks for the depth. I’ve had a couple friends who switched to SSRIs and saw a big drop in those bladder issues. Just a heads‑up: keep an eye on any dizziness after the change, it can happen too.
Louis Robert
June 25, 2023 AT 11:37Bottom line: if you feel like you’re constantly holding urine, let your doctor know-there are alternatives.
tim jeurissen
July 5, 2023 AT 00:57While your summary is concise, it omits the critical distinction between acute and chronic retention, which bears on management protocols.
lorna Rickwood
July 14, 2023 AT 14:17Ever wonder why the brain’s chemistry can throw the bladder off‑balance? It’s a reminder that our bodies are all linked in ways we barely grasp.
Mayra Oto
July 24, 2023 AT 03:37From a cultural standpoint, many communities still view urinary problems as taboo, which can delay seeking help.
S. Davidson
August 2, 2023 AT 16:57Technically, the literature cites a 12% incidence of retention with high‑dose imipramine, an important statistic you should highlight.
Haley Porter
August 12, 2023 AT 06:17The interplay between neurotransmitter modulation and peripheral organ function is a classic example of systemic pharmacology. One cannot isolate the mood‑lifting benefits without acknowledging the downstream somatic effects. In practice, this necessitates a holistic evaluation of risk versus reward.
Samantha Kolkowski
August 21, 2023 AT 19:37Totally agree-looking at the whole picture helps patients feel heard and understood.
Nick Ham
August 31, 2023 AT 08:57Short and sweet: monitor, report, adjust.
Jennifer Grant
September 9, 2023 AT 22:17Philosophically speaking, the body’s response to chemical alteration mirrors the broader human experience of adaptation. When a medication intervenes, it not only targets a specific pathology but also reshapes the equilibrium of other physiological circuits. The tension between intended therapeutic outcomes and unintended side effects can be seen as a microcosm of the balance we constantly seek in life. Recognizing this, patients might find solace in the knowledge that their complaints are not isolated anomalies but part of a larger systemic dialogue. Consequently, fostering open communication with healthcare providers becomes an act of self‑advocacy, ensuring that the therapeutic narrative remains collaborative rather than unilateral.
Kenneth Mendez
September 19, 2023 AT 11:37Don’t trust big pharma’s “safe” label when they hide the bladder side‑effects in fine print.
Gabe Crisp
September 29, 2023 AT 00:57Truth is, the only safe path is vigilance and questioning authority.
Paul Bedrule
October 8, 2023 AT 14:17The mechanistic insight into anticholinergic load underscores why some patients develop retention while others do not.
yash Soni
October 18, 2023 AT 03:37Great, another reminder that meds aren’t harmless.