
One in three adults in the U.S. has a condition that puts their kidneys at risk - and most don’t even know it. Chronic kidney disease (CKD) doesn’t come with warning signs until it’s advanced. By then, damage is often irreversible. But here’s the truth: kidney disease prevention isn’t about complex treatments or expensive drugs. It’s about everyday choices - what you eat, how you move, and what you avoid. The good news? Up to 85% of cases can be prevented or delayed with simple, consistent habits.
What Really Puts Your Kidneys at Risk?
Your kidneys filter about 120 to 150 quarts of blood every day. That’s a lot of work. When something strains that system long-term, damage builds silently. The biggest threats aren’t mysterious toxins or rare illnesses. They’re common conditions most people treat as normal.
Diabetes is the number one cause of kidney failure. About 40% of people with diabetes will develop kidney disease. High blood sugar slowly scars the tiny filters in your kidneys, making them leak protein and lose function. If your A1C stays above 7% for years, your kidneys pay the price.
Hypertension is the second major culprit. About 68% of people with CKD have high blood pressure. When your blood pressure stays above 140/90 mm Hg, it damages the blood vessels in your kidneys. Over time, they can’t filter waste properly. The goal? Keep it at or below 120/80 mm Hg. That’s not just a number - it’s your kidney’s lifeline.
Obesity doesn’t just affect your waistline. Extra weight forces your kidneys to work harder, increases inflammation, and raises your odds of developing diabetes and high blood pressure. Losing just 5 kg (about 11 pounds) can cut your risk of kidney disease by 25-30%.
And then there’s smoking. Smokers have a 50% higher chance of kidney function decline than non-smokers. Smoking narrows blood vessels, reduces blood flow to the kidneys, and speeds up scarring. Quitting doesn’t just help your lungs - it gives your kidneys a chance to recover.
What You Eat Matters More Than You Think
Food isn’t just fuel. For your kidneys, it’s either protection or poison. The standard American diet - high in salt, sugar, and processed foods - is a silent killer for renal health.
Sodium is the biggest dietary offender. Most people eat over 3,400 mg a day. The target? Under 2,300 mg. That’s about one teaspoon of salt. But most of that salt isn’t from the shaker. It’s in bread, canned soup, deli meats, frozen meals, and restaurant food. Switch to fresh ingredients. Cook at home. Read labels. Even cutting out one processed snack a day can drop your sodium by 500 mg.
Sugar is another hidden threat. Sugary drinks - soda, energy drinks, sweetened teas - make up 7% of daily calories for most American adults. That sugar doesn’t just cause weight gain. It spikes insulin, increases fat around organs, and damages blood vessels, including those in your kidneys. Swap soda for water, sparkling water, or unsweetened tea. You’ll lower your diabetes risk and protect your kidneys at the same time.
Protein isn’t the enemy - but too much can be. If you’re healthy, your body handles normal protein intake fine. But if you already have early kidney damage, eating more than 1.2 grams of protein per kilogram of body weight can overload your kidneys. That’s about 80-90 grams for a 70 kg person. Focus on lean sources: fish, chicken, beans, lentils. Cut back on red meat and processed meats like bacon and sausages.
And don’t forget fruits and vegetables. Aim for at least five portions a day. They’re packed with antioxidants, fiber, and potassium - all of which help lower blood pressure and reduce inflammation. A banana, an apple, spinach in your salad, carrots as a snack - these aren’t just healthy choices. They’re kidney-saving ones.
Move More, Sit Less
You don’t need to run marathons to protect your kidneys. You just need to move regularly.
The CDC and NHS both agree: 150 minutes of moderate exercise each week - that’s 30 minutes, five days a week - makes a real difference. Brisk walking, cycling, swimming, dancing - anything that gets your heart pumping. Add strength training twice a week. Squats, lunges, resistance bands, or even carrying groceries can build muscle and improve insulin sensitivity.
Why does this matter? Exercise helps control blood pressure, lowers blood sugar, reduces body fat, and improves circulation. All of these directly protect your kidneys. And it’s not all about the gym. Take the stairs. Walk after dinner. Park farther away. Stand up every hour. These small shifts add up.
One study showed that people who started walking 30 minutes a day cut their risk of developing diabetes by 26% over three years. Since diabetes causes 40% of kidney failure, that’s a powerful chain reaction.

Medications, Supplements, and What to Avoid
Some of the most common over-the-counter drugs can quietly harm your kidneys. NSAIDs like ibuprofen, naproxen, and aspirin - taken daily for headaches or back pain - are responsible for 3-5% of new kidney disease cases each year. They reduce blood flow to the kidneys, especially if you’re dehydrated or already have high blood pressure.
If you need pain relief, talk to your doctor about safer options. Acetaminophen (Tylenol) is usually gentler on kidneys - but don’t exceed the daily limit. Always check labels. Some cold medicines, supplements, and herbal remedies contain hidden NSAIDs or kidney-toxic ingredients.
Alcohol isn’t off the hook either. More than one drink a day for women or two for men increases blood pressure and can lead to liver damage - which also stresses your kidneys. Stick to moderate limits. If you’re diabetic or hypertensive, even one drink might be too much.
And don’t skip your vaccines. People with kidney disease are 3-5 times more likely to get seriously ill from the flu. An annual flu shot isn’t optional - it’s part of kidney protection.
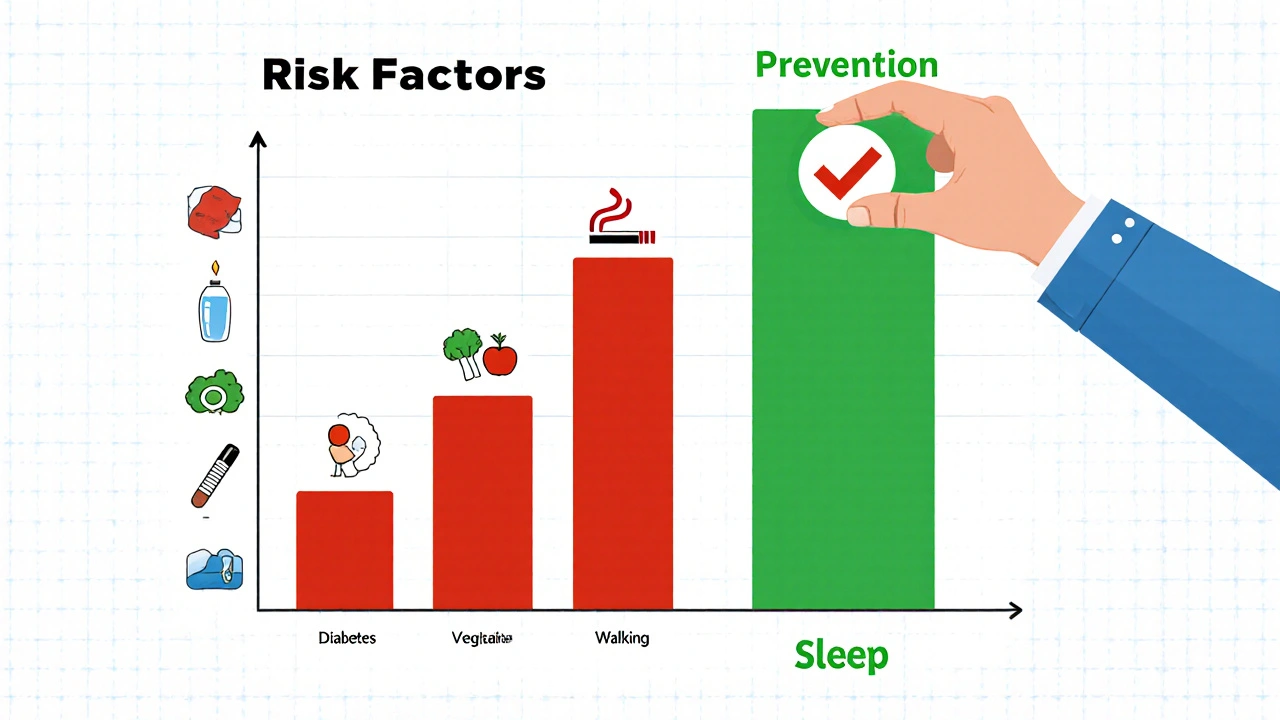
Stress, Sleep, and the Hidden Factors
Chronic stress doesn’t just make you feel overwhelmed - it raises cortisol, which increases blood pressure and blood sugar. A Johns Hopkins study found that people who practiced mindfulness, meditation, or deep breathing for 10-15 minutes a day slowed kidney disease progression by 15%.
Sleep matters too. Poor sleep disrupts hormones that regulate blood pressure and glucose. If you’re snoring, waking up tired, or feeling sleepy during the day, get checked for sleep apnea. It’s common in people with kidney disease and makes both conditions worse.
Even small changes here help. Try turning off screens an hour before bed. Keep a consistent sleep schedule. Create a calm bedtime routine. Your kidneys will thank you.
Screening: The Most Important Step You Might Be Skipping
Here’s the hard truth: early kidney disease has no symptoms. No pain. No swelling. No warning. That’s why 90% of people with CKD don’t know they have it.
If you have diabetes, high blood pressure, heart disease, obesity, or a family history of kidney failure - you need screening. It’s simple: a blood test for creatinine (to calculate GFR) and a urine test for albumin. Both take minutes. Both are covered by insurance.
Get tested at least once a year. If you’re over 60, get tested even if you feel fine. Early detection means you can stop the damage before it’s too late. And if you’re already diagnosed with early-stage CKD (Stages 1-2), lifestyle changes can reverse or halt progression in up to 40% of cases.
Real People, Real Results
Meet Maria, 58, from Sydney. She had prediabetes and high blood pressure. Her doctor told her she was at high risk for kidney disease. She didn’t want to wait for symptoms. So she started walking 30 minutes every morning. She swapped soda for sparkling water. She cooked meals with less salt. In six months, her A1C dropped from 6.2% to 5.4%. Her blood pressure fell from 142/88 to 118/76. Her kidney function stayed stable - and she lost 8 kg.
Or James, 62, who smoked for 40 years. He was diagnosed with early CKD. He quit smoking cold turkey. He started eating more vegetables. He got his blood pressure under control. Two years later, his GFR improved by 12 points - a rare reversal in kidney disease.
These aren’t miracles. They’re the result of consistent, doable changes.
What’s Next?
Preventing kidney disease isn’t about perfection. It’s about progress. You don’t have to overhaul your life overnight. Start with one thing: track your sodium intake for a week. Swap one sugary drink for water. Take a 15-minute walk after dinner. Get your blood pressure checked.
The system is designed to make you sick. Processed food, sedentary jobs, stress, and delayed care - they all stack up. But you have power. Every healthy choice is a shield for your kidneys.
And if you’re reading this, you’re already on the right path. The next step? Talk to your doctor. Get screened. Make a plan. Your kidneys are working for you every minute. It’s time to work for them.
Can kidney disease be reversed?
Early-stage kidney disease (Stages 1-2) can often be stabilized or even improved with lifestyle changes. Losing weight, controlling blood pressure and blood sugar, reducing sodium, and quitting smoking can slow or reverse damage. But once scarring sets in (Stage 3 and beyond), the damage is usually permanent. The goal shifts from reversal to slowing progression and preventing complications.
What foods should I avoid if I want to protect my kidneys?
Avoid processed foods high in sodium - think canned soups, frozen meals, deli meats, and salty snacks. Cut back on sugary drinks like soda and sweetened teas. Limit red and processed meats. Watch out for hidden salt in bread and condiments. Also, avoid herbal supplements like aristolochic acid, which are known to damage kidneys. Stick to whole, unprocessed foods: fresh vegetables, fruits, lean proteins, and whole grains.
How much water should I drink daily for kidney health?
There’s no one-size-fits-all number. Most healthy adults need about 1.5 to 2 liters (6-8 cups) of fluid daily. But if you have heart failure, advanced kidney disease, or take certain medications, your doctor may advise limits. The best rule? Drink when you’re thirsty, and check your urine color. Pale yellow means you’re well-hydrated. Dark yellow or amber means you need more fluid.
Are over-the-counter painkillers safe for kidneys?
Regular use of NSAIDs like ibuprofen (Advil, Motrin) or naproxen (Aleve) can damage kidneys, especially if taken daily or if you’re dehydrated, older, or have existing kidney issues. Occasional use for short-term pain is usually fine. But if you need pain relief often, talk to your doctor. Acetaminophen (Tylenol) is generally safer for kidneys, but don’t exceed 3,000 mg per day.
Who should get tested for kidney disease?
Anyone with diabetes, high blood pressure, heart disease, obesity, or a family history of kidney failure should get tested annually. People over 60, Black or Hispanic individuals (who have higher risk), and those with autoimmune conditions should also be screened. Testing is simple: a blood test for creatinine and a urine test for albumin. Both are covered by most insurance plans.
Can stress really affect kidney function?
Yes. Chronic stress raises cortisol and adrenaline, which increase blood pressure and blood sugar - both major drivers of kidney damage. Studies show that people who practice mindfulness, meditation, or deep breathing for just 10-15 minutes a day can slow kidney disease progression by up to 15%. Stress management isn’t a luxury - it’s part of kidney protection.
Is kidney disease hereditary?
Some forms of kidney disease, like polycystic kidney disease, are directly inherited. But more commonly, family history increases risk through shared habits - poor diet, inactivity, uncontrolled diabetes or high blood pressure - rather than genetics alone. If a close relative had kidney failure, you’re at higher risk, but lifestyle changes can still significantly lower your chances.
How does smoking damage the kidneys?
Smoking narrows and hardens the blood vessels, reducing blood flow to the kidneys. It also increases inflammation and speeds up scarring in kidney tissue. Smokers are 50% more likely to lose kidney function over time. Quitting slows this damage - even after years of smoking. Within a year of quitting, kidney function decline begins to slow significantly.

Rachel Wusowicz
November 15, 2025 AT 04:53Okay, but have you ever stopped to think that the FDA, Big Pharma, and the kidney industry are ALL in cahoots?? I mean, why else would they make you believe you need to "eat more vegetables" and "drink water"?? It's all a distraction from the real culprit: fluoridated water!! They're poisoning us slowly through the pipes, and this article? It's a placebo for the sheeple. I've been drinking distilled water with lemon and Himalayan salt for 7 years-my kidneys are humming like a Tesla engine. They don't want you to know this.
Oyejobi Olufemi
November 15, 2025 AT 21:54You people are delusional. This entire post is a capitalist lie dressed up as wellness. Kidney disease isn't caused by soda or salt-it's caused by the systemic collapse of the American healthcare model, the erosion of ancestral diets, and the deliberate suppression of traditional healing systems. Your "150 minutes of exercise" is a Band-Aid on a severed artery. The real solution? Abolish the medical-industrial complex and return to ancestral fasting, herbal kidney tonics, and communal living. Until then, you're just rearranging deck chairs on the Titanic-and your "GFR" is just a number they invented to sell you more tests.
Daniel Stewart
November 17, 2025 AT 16:08There's a beautiful irony here. We're told to "eat less salt" while the entire food system is engineered to make us crave it. But the real tragedy isn't sodium-it's the loss of meaning. We don't cook anymore. We don't sit with our meals. We don't honor the body as a temple, just a machine to be optimized. The kidneys aren't failing because of sugar-they're failing because we've forgotten how to be human. And no amount of kale smoothies will fix that.
Jamie Watts
November 18, 2025 AT 12:12John Mwalwala
November 18, 2025 AT 16:42Let me drop some nephrology jargon on you. The renin-angiotensin-aldosterone system (RAAS) is the real villain here. ACE inhibitors and ARBs aren't just for BP-they're renoprotective. And guess what? Most people don't even know what RAAS stands for. The diet stuff? It's adjunctive. The real game-changer? Pharmacologic intervention + early screening. That's why I always tell my patients: don't wait for symptoms. Get your urine albumin-to-creatinine ratio tested. It's the most sensitive early marker. And yes, I'm a nephrologist. No, I don't take supplements. Yes, I drink water. But I also prescribe lisinopril. Just saying.
Deepak Mishra
November 20, 2025 AT 07:54OMG I JUST REALIZED I ATE A BAG OF CHIPS YESTERDAY AND I'M GONNA DIE FROM KIDNEY FAILURE 😭😭😭 I SWORE I'D STOP BUT THE SALT IS TOO GOOD 😭 I'M SO SORRY TO MY KIDNEYS 😭 THEY'VE BEEN WORKING SO HARD 😭 I'M GOING TO START DRINKING WATER AND EATING BROCCOLI TOMORROW I PROMISE 😭🙏🫶
Diane Tomaszewski
November 21, 2025 AT 10:57I just started walking after dinner and swapping soda for sparkling water. It's not perfect but it feels right. I used to think I had to change everything at once but now I see it's just one small thing after another. My mom had kidney issues and I didn't want to end up like her. So I'm trying. Not because it's trendy. Just because I care. And if I can do it, anyone can.
Dan Angles
November 22, 2025 AT 11:49While the recommendations presented are broadly aligned with current clinical guidelines from the National Kidney Foundation and the American Heart Association, I would respectfully underscore the critical importance of individualized risk stratification. The population-level data cited must be contextualized within socioeconomic determinants of health, access to nutritious food, and structural barriers to preventive care. Lifestyle modification, while essential, is insufficient without systemic support. We must advocate for policy-level interventions alongside individual behavior change.
David Rooksby
November 24, 2025 AT 00:32Okay so here's the thing nobody's saying: the whole kidney disease thing is just a scam to get people to buy expensive blood tests and fancy supplements. I did a deep dive into the CDC data and guess what? The rise in CKD diagnoses tracks *exactly* with the rise in Medicare billing codes for renal panels. Coincidence? I think not. Also, who decided that 120/80 is the magic number? Some guy in a lab coat in 1998? My grandpa was 150/90 and lived to 92 drinking whiskey and eating bacon. Maybe we're over-medicalizing normal life. And why is no one talking about how glyphosate in our food is the real killer? They don't want you to know that.
Melanie Taylor
November 25, 2025 AT 07:21Just wanted to say thank you for this post!! 🙏 I'm from a culture where kidney health isn't talked about at all and I didn't even know you could prevent it!! I'm sharing this with my family in Nigeria and we're all going to start drinking more water and cutting back on the salted fish 😊 I'm so grateful for people who share real info like this!! 💚🫶
Teresa Smith
November 25, 2025 AT 21:04Let me be clear: this isn't about willpower. It's about access. You can't "eat fresh vegetables" if you live in a food desert. You can't "walk 30 minutes" if you work two jobs and your neighborhood is unsafe. This article reads like it was written for people who have time, money, and privilege. I appreciate the intent, but the tone ignores reality. Prevention requires policy-subsidized healthy food, safe public spaces, affordable healthcare-not just "swap soda for water." We need systemic change, not individual guilt trips.
ZAK SCHADER
November 27, 2025 AT 19:13Look I'm not some hippie but this whole thing is just another way for the government to control us. Kidney disease? More like kidney fraud. They want you scared so you'll take their pills and get their tests. I'm American. I eat what I want. I don't need some doctor telling me how to live. If my kidneys go? Fine. At least I lived. This is why America's weak. Everyone's afraid of a little salt. Get tough.
Danish dan iwan Adventure
November 28, 2025 AT 16:16Protein overload = glomerular hyperfiltration. Early CKD = RAS blockade + low sodium + glycemic control. No fluff. Data only. You're welcome.