Drug Reaction Risk Calculator
This tool helps you understand if your medication reaction is likely dose-related (Type A) or non-dose-related (Type B) based on key factors. Remember: Always consult your doctor for medical advice.
Enter information above to see risk assessment
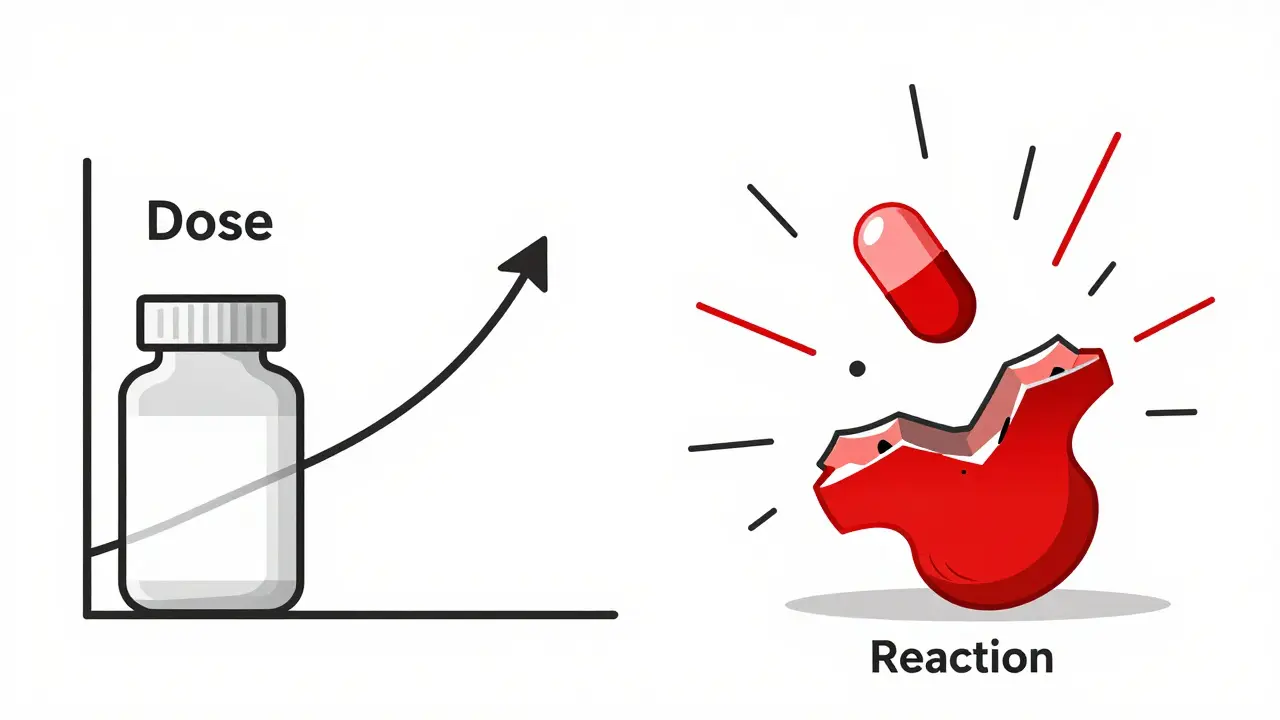
When you take a pill, you expect it to help. But sometimes, it causes harm. Not all side effects are the same. Some happen because you took too much. Others strike out of nowhere, even at the lowest dose. Understanding the difference between dose-related and non-dose-related side effects isn’t just for doctors - it’s critical for anyone taking medication regularly.
What Are Dose-Related Side Effects?
Dose-related side effects, also called Type A reactions, are predictable. They’re just an extension of how the drug is supposed to work - but turned up too high. Think of it like turning a dimmer switch too far. The light gets brighter, but if you go past the limit, it blows. These reactions follow the basic law of pharmacology: more drug = stronger effect. They’re common - about 80% of all adverse drug reactions fall into this category. And they’re usually not surprising. If you’re on blood pressure meds and your blood pressure drops too low, that’s a dose-related reaction. Same with low blood sugar from insulin, or bleeding from warfarin when your INR climbs above 4.0. Drugs with a narrow therapeutic index are especially risky. That means the gap between the right dose and the dangerous dose is tiny. Digoxin, used for heart failure, has a therapeutic range of 0.5 to 0.9 ng/mL. Go above 2.0 ng/mL, and you’re in toxicity territory. Lithium, used for bipolar disorder, is the same - 0.6 to 1.0 mmol/L is safe; above 1.2, and you risk tremors, confusion, or even seizures. These reactions often show up in older adults or people with kidney or liver problems. If your kidneys aren’t clearing the drug well, it builds up. A 65-year-old on diazepam might process it 30-40% slower than a 30-year-old. Or take a statin with clarithromycin - that combo can spike statin levels five to ten times, leading to muscle damage. These aren’t accidents. They’re preventable with dose adjustments and monitoring.What Are Non-Dose-Related Side Effects?
Non-dose-related side effects, or Type B reactions, are the opposite. They’re unpredictable. They don’t follow the rules of pharmacology. You can take the exact right dose - and still get a life-threatening reaction. These are rare - only 15-20% of all side effects - but they cause 70-80% of serious hospitalizations. Why? Because they’re often immune-driven. Your body sees the drug as an invader and attacks. That’s what happens in anaphylaxis after penicillin, or Stevens-Johnson syndrome from lamotrigine. You might have taken the drug before without issue. Then, out of nowhere, your skin blisters, your airway swells, or your liver shuts down. These reactions don’t get worse with higher doses. They either happen or they don’t. Once your immune system is sensitized, even a tiny amount - like one 500mg pill of amoxicillin - can trigger a massive response. That’s why patients who’ve had a severe reaction are told to carry an epinephrine auto-injector. The dose doesn’t matter anymore. The trigger does. Some Type B reactions are tied to your genes. Take abacavir, an HIV drug. If you carry the HLA-B*57:01 gene variant, your risk of a severe hypersensitivity reaction jumps from less than 1% to over 50%. That’s why doctors now test for this gene before prescribing. The test costs around $200 - but it prevents a reaction that could kill you.Why the Confusion? The Dose Paradox
You might hear someone say, “There’s no such thing as a non-dose-related reaction.” And technically, they’re right. Every drug has a dose-response curve. So why do some reactions seem to ignore it? The answer lies in individual variation. Some people are so sensitive that even the smallest dose triggers a reaction. Others need ten times the normal amount. In population studies, these differences blur the line. A reaction that occurs at 5mg in one person and 150mg in another looks like it has no dose pattern - but it’s just hidden by variability. Experts like Dr. Jeffrey K. Aronson explain that Type B reactions aren’t truly dose-independent. They’re dose-unrelated in practice. The threshold is so low or so variable that it’s impossible to predict who will react and at what level. That’s why we treat them as if dose doesn’t matter - because for the individual, it often doesn’t.How Doctors Tell the Difference
In the clinic, the distinction guides treatment. For dose-related reactions, the fix is simple: lower the dose, monitor levels, or stop interacting drugs. If your INR is too high on warfarin, you cut the dose. If your creatinine clearance drops, you reduce metformin. Therapeutic drug monitoring - checking blood levels of drugs like vancomycin, phenytoin, or lithium - is routine for these cases. For non-dose-related reactions, the only safe move is to stop the drug - forever. No dose adjustment will help. You can’t “build tolerance.” And you can’t try a lower dose next time. Even a tiny amount can trigger the same reaction. That’s why patients with a history of Stevens-Johnson syndrome or anaphylaxis are given medical alert bracelets and strict avoidance lists. Genetic testing is changing the game. Before giving carbamazepine to someone of Asian descent, many hospitals now test for HLA-B*15:02 - a gene variant linked to a 97% risk of Stevens-Johnson syndrome. The test is cheap, fast, and saves lives. The FDA now lists pharmacogenomic testing requirements on 28 drug labels, including abacavir, clopidogrel, and codeine.Who’s at Risk?
Dose-related reactions hit older adults hardest. Why? Slower metabolism, reduced kidney function, and taking five or more medications. Anticoagulants, insulin, and oral diabetes drugs cause 67% of emergency visits for side effects in people over 65. Non-dose-related reactions can strike anyone - but they’re more common in people with autoimmune conditions, a history of allergies, or certain genetic backgrounds. Women are more likely to develop drug-induced liver injury. People with HIV or hepatitis are at higher risk for severe skin reactions. The real danger? Mislabeling. A patient develops a rash after amoxicillin. The doctor says, “It’s not the dose - it’s an allergy.” But what if they’ve never taken it before? What if the rash was caused by a viral infection? Misdiagnosing a Type B reaction as a true allergy leads to unnecessary avoidance of entire drug classes - and worse alternatives.
What This Means for You
If you’re on long-term medication, know your risks.- Keep a list of all your meds - including supplements - and share it with every provider.
- Ask: “Is this drug known for side effects that get worse with higher doses?”
- If you’ve had a serious reaction before, tell every doctor, every time. Don’t assume they’ll check your records.
- Ask about genetic testing if you’re prescribed abacavir, carbamazepine, or thiopurines.
- Don’t ignore a rash, fever, or swelling - even if it seems minor. Type B reactions can escalate fast.
The Bigger Picture
The global pharmacogenomics market is growing fast - projected to hit nearly $18 billion by 2030. Why? Because we’re moving from one-size-fits-all dosing to personalized medicine. Algorithms now predict Type A reactions with 82% accuracy. But Type B? Only 63%. That gap tells us something important: we’re getting better at managing the predictable. The unpredictable? That’s the next frontier. Regulators are responding. The FDA now requires Risk Evaluation and Mitigation Strategies (REMS) for 71 drugs with high Type B risks. The EMA has updated guidelines to distinguish between “dose-independent” and “dose-unrelated” reactions - acknowledging that even immune reactions may have hidden thresholds. This isn’t just science. It’s safety. And it’s personal.Can a dose-related side effect become non-dose-related over time?
No. A dose-related reaction stays dose-related. If you develop a new reaction that doesn’t respond to dose changes, it’s likely a different mechanism - possibly a new Type B reaction. For example, someone on long-term lithium might develop tremors (Type A) and later develop a rash (Type B). These are two separate events, not a progression.
Are non-dose-related side effects always allergic reactions?
No. While many Type B reactions are immune-mediated (like anaphylaxis or Stevens-Johnson syndrome), others aren’t. Drug-induced liver injury or agranulocytosis from clozapine can be idiosyncratic - meaning they’re caused by unknown biological mechanisms, not classic allergies. Not all Type B reactions involve IgE antibodies or histamine release.
Can you outgrow a non-dose-related side effect?
Almost never. Once your immune system or metabolism has reacted to a drug in a Type B way, the risk remains. Re-exposure can trigger the same or worse reaction. Even if you haven’t taken the drug for years, your body remembers. Avoidance is the only safe strategy.
Do all drugs have both types of side effects?
No. Some drugs are mostly Type A - like insulin or warfarin. Others are mostly Type B - like allopurinol or sulfonamides. Most drugs have a mix, but one type usually dominates. The key is knowing which one your drug leans toward so you know what to watch for.
If I have a side effect, should I always stop the drug?
Not always. For mild dose-related side effects - like nausea from metformin or dizziness from blood pressure meds - your doctor may adjust the dose or timing. But if you develop a rash, swelling, fever, or breathing trouble, stop the drug and seek help immediately. Don’t wait to see if it gets worse. Type B reactions can turn deadly in hours.

Christina Widodo
January 12, 2026 AT 10:47Had a rash after amoxicillin once and they labeled it an allergy - turned out it was a virus. Now I’m paranoid every time I get a skin thing. Why do doctors jump to ‘allergy’ so fast?
Katherine Carlock
January 13, 2026 AT 01:30This is such a clear breakdown 😍 I’ve been on lithium for years and never knew how thin that safety line was. My doc just says ‘take it’ - now I’m gonna ask for the blood test.
Sumit Sharma
January 13, 2026 AT 19:59It is imperative to recognize that Type B reactions are not merely ‘allergies’ - they represent idiosyncratic pharmacodynamic disruptions often mediated by HLA haplotypes. The clinical implications are profound, particularly in populations with high HLA-B*15:02 prevalence such as Southeast Asians. Failure to implement preemptive genotyping constitutes a breach of standard-of-care.
Sona Chandra
January 15, 2026 AT 02:46MY BEST FRIEND DIED FROM STEVENS-JOHNSON AFTER A SIMPLE AMOXICILLIN PRESCRIPTION. NO ONE TOLD HER IT COULD HAPPEN. THIS ISN’T JUST ‘SCIENCE’ - IT’S MURDER BY NEGLIGENCE.
Lelia Battle
January 16, 2026 AT 13:15There’s something almost poetic about the duality here - one side of medicine is mathematics, predictable as gravity. The other is mystery, like a whisper from the body’s hidden chambers. We measure, we model, we chart - but sometimes, the body simply says ‘no’ without reason. And in that silence, we confront the limits of control.
Perhaps the real question isn’t whether side effects are dose-related or not - but whether we’re listening closely enough when the body speaks in ways we don’t yet understand.
George Bridges
January 18, 2026 AT 00:44My mom took warfarin for years. One day she got a nosebleed that wouldn’t stop. They said it was the dose. But what if it was something else? I wish they’d tested her more before assuming it was just ‘normal’.
Jay Powers
January 18, 2026 AT 14:16People don’t realize how often they’re misdiagnosed with drug allergies. I had a rash after sulfa and was told never to take it again. Turns out I’ve taken it twice since - no problem. It was just heat rash. Don’t let a label stick if it doesn’t fit
Prachi Chauhan
January 19, 2026 AT 13:46My cousin got sick after carbamazepine. They said it was ‘bad luck’. But if they tested her gene first, maybe she’d still be here. Why wait for death to do the right thing?
Jennifer Phelps
January 20, 2026 AT 09:06My doctor never mentioned genetic testing for clopidogrel. I had a stroke last year. Now I’m wondering if it was because my body couldn’t process it. Should’ve asked sooner
Bryan Wolfe
January 21, 2026 AT 12:19Look, I get it - medicine is complex, and we’re all just trying to stay alive. But here’s the thing: if your doctor isn’t talking to you about dose risks vs. weird immune reactions, you need to push harder. Ask for the blood levels. Ask about genes. Ask what the worst-case scenario is. You’re not being ‘difficult’ - you’re being smart. And if they roll their eyes? Find a new doctor. Your life isn’t a guess.
Also - if you’ve ever had a rash, swelling, or fever after a med? Write it down. Keep it in your phone. Show it to every new provider. Don’t assume they’ll find it. They won’t. I learned this the hard way. You’re your own best advocate.
beth cordell
January 21, 2026 AT 21:53Thank you for this 🙏 I just started abacavir and got the HLA test - it came back negative. I cried. I didn’t even know that was a thing. This post saved me. ❤️