Key Takeaways
- Diltiazem HCL is a calcium‑channel blocker that eases angina by widening coronary arteries.
- It works best for stable angina and can be combined with nitroglycerin or beta‑blockers when needed.
- Typical dosing starts at 60 mg once daily, with gradual titration based on response and blood pressure.
- Common side effects include headache, flushing, and a slower heart rate; serious reactions are rare.
- Regular monitoring of blood pressure, heart rate, and liver function helps keep therapy safe.
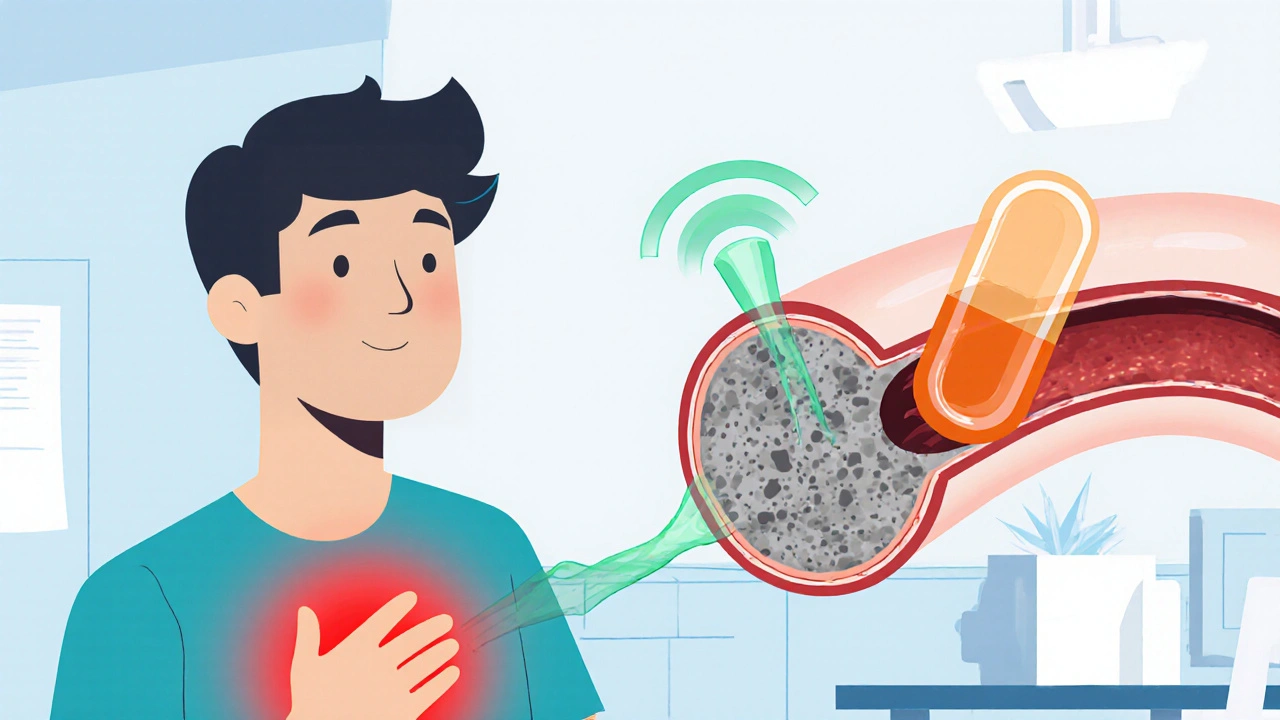
When you feel that squeezing sensation in your chest, you’re probably experiencing angina - the heart’s warning sign that it isn’t getting enough oxygen. One of the most proven ways to calm that pain is Diltiazem HCL is a calcium‑channel blocker medication used to treat angina and certain heart rhythm disorders. In this guide we’ll break down exactly how Diltiazem works, who should take it, how to use it safely, and what to expect along the way.
What Is Angina and Why Does It Hurt?
Angina pectoris is chest discomfort caused by reduced blood flow through the coronary arteries. The most common trigger is atherosclerosis - plaque buildup that narrows the vessel lumen. When the heart tries to pump harder during activity or stress, the narrowed arteries can’t deliver enough oxygen, leading to the classic pressure or burning feeling.
There are two main types:
- Stable angina: Predictable, usually triggered by exertion and relieved by rest or medication.
- Unstable angina: Occurs at rest, lasts longer, and signals a higher risk of heart attack.
Understanding the type matters because it guides which drugs will be most effective.
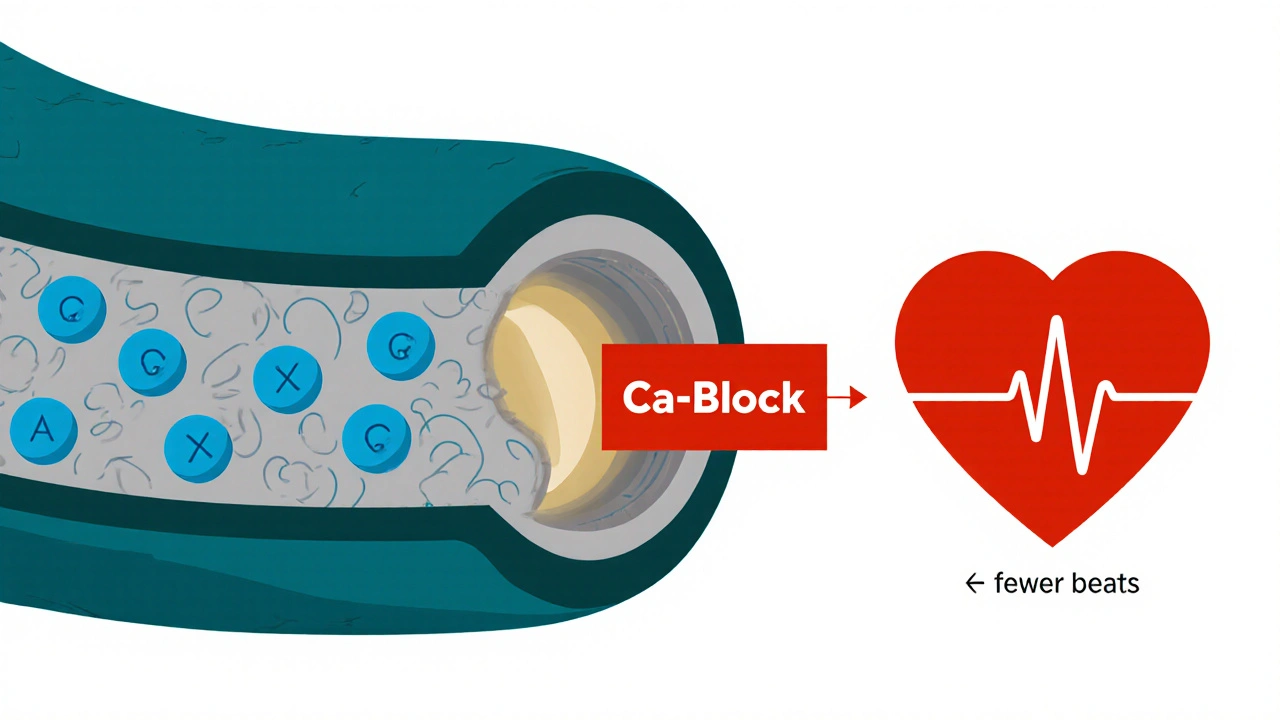
How Diltiazem HCL Works - The Calcium‑Channel Blocker Angle
Calcium ions are essential for muscle contraction, including the heart and the smooth muscle lining blood vessels. Calcium Channel Blocker (CCB) medicines prevent calcium from entering these cells. By doing so, they achieve two things that directly help angina:
- Vasodilation: The coronary arteries relax, widening the passage for blood and oxygen.
- Heart‑rate reduction: A slower heart beats uses less oxygen, lowering the heart’s demand.
Diltiazem belongs to the non‑dihydropyridine subclass of CCBs, which has a stronger effect on the heart’s electrical system than pure vasodilators like nifedipine. This dual action makes it especially useful for patients who need both relief of chest pain and control of irregular heart rhythms.
When Doctors Choose Diltiazem Over Other Angina Drugs
Several drug families treat angina: CCBs, beta‑blockers, nitrates, and ranolazine. Diltiazem shines in these scenarios:
- Patients who cannot tolerate beta‑blockers because of asthma or severe depression.
- Those with co‑existing atrial fibrillation where rate control is needed.
- Individuals who experience “rebound” chest pain after stopping short‑acting nitrates.
In many guidelines, Diltiazem sits alongside Nifedipine as a first‑line CCB for stable angina. The choice often comes down to side‑effect profiles and the patient’s heart‑rate target.
Dosage, Formulations, and How to Take It
Doctors typically start patients on 60 mg once daily (extended‑release tablets). If the response is inadequate and blood pressure permits, the dose can be increased in 30 mg increments up to 360 mg per day, split into once‑daily or twice‑daily dosing.
Key points for safe administration:
- Take the tablet with a full glass of water, preferably at the same time each day.
- Avoid grapefruit juice - it interferes with the drug’s metabolism and can raise plasma levels.
- Do not abruptly stop the medication; taper under medical supervision to prevent rebound angina.
Extended‑release capsules should be swallowed whole; crushing or chewing destroys the controlled‑release mechanism and may cause a sudden drop in blood pressure.
What to Expect - Benefits and Timeline
Most patients report noticeable relief within 1-2 weeks of consistent dosing. The drug’s half‑life (around 3-5 hours for the immediate form, longer for extended‑release) means steady blood levels are achieved after about 4-5 days. Benefits include:
- Reduced frequency of chest pain episodes during exercise.
- Lower resting heart rate (often 5-10 beats per minute).
- Improved exercise tolerance measured by treadmill tests.
Long‑term studies, such as the 2022 FDA‑approved clinical trial database, show that continued Diltiazem use lowers the risk of hospitalization for angina by roughly 15 % compared with placebo.
Possible Side Effects and When to Call the Doctor
Like any medication, Diltiazem carries a side‑effect profile. Most are mild and transient:
- Headache (due to vasodilation)
- Flushing or warmth in the face and neck
- Dizziness, especially when standing up quickly
- Peripheral edema (swelling in ankles)
Serious, though rare, reactions include:
- Bradycardia - heart rate below 50 bpm
- Severe hypotension - systolic BP under 90 mmHg
- Allergic skin rash or hepatitis
If you experience any of the serious signs, seek medical attention immediately. Routine labs (liver enzymes, electrolytes) every 6-12 months help catch issues early.
Comparing Diltiazem with Other Angina Medications
| Feature | Diltiazem HCL | Nifedipine | Metoprolol (β‑blocker) | Nitroglycerin (short‑acting) |
|---|---|---|---|---|
| Drug class | Non‑dihydropyridine CCB | Dihydropyridine CCB | Beta‑blocker | Nitrate |
| Primary action | Vasodilation + heart‑rate reduction | Strong vasodilation | Heart‑rate & contractility reduction | Rapid vasodilation |
| Best for | Stable angina with HR control needs | Patients needing pure vasodilation | Athletes with high HR or arrhythmia | Acute chest pain episodes |
| Common side effects | Headache, edema, bradycardia | Flushing, peripheral edema | Fatigue, cold extremities | Headache, hypotension |
| Typical dose | 60‑360 mg daily (ER) | 30‑90 mg daily | 50‑200 mg daily | 0.3‑0.6 mg sublingual PRN |
| Contra‑indications | Severe AV block, untreated heart failure | Severe hypotension | Severe asthma, bradycardia | Phosphodiesterase inhibitor use |
Choosing the right drug often involves balancing the need for blood‑pressure control, heart‑rate management, and side‑effect tolerance. Your cardiologist will weigh these factors along with your overall health picture.
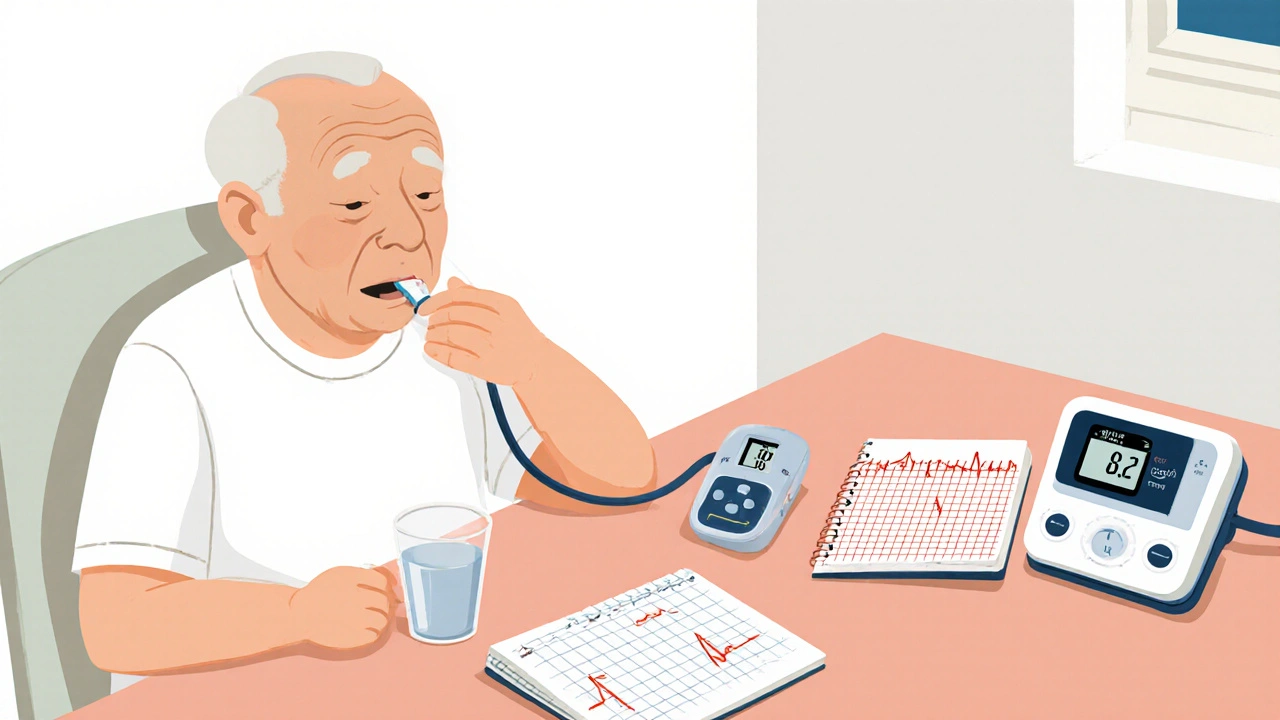
Monitoring and Follow‑Up - Keeping Therapy on Track
Continuous assessment ensures the medication stays effective and safe:
- Blood pressure & heart rate: Check at each visit; target < 130/80 mmHg and 60‑80 bpm if not on other rate‑controlling drugs.
- Electrocardiogram (ECG): Baseline and yearly to spot conduction changes.
- Lab work: Liver function tests and electrolytes every 6-12 months.
- Symptom diary: Record chest pain episodes, activity level, and any side effects.
Adjustments are made based on these data points. If pain persists despite maximal tolerated Diltiazem, adding a low‑dose nitrate or switching to a different CCB may be considered.
Special Populations - What About the Elderly, Pregnant Women, and Kids?
Evidence shows Diltiazem can be used safely in older adults, but start at the lowest dose (30 mg) and titrate slowly due to reduced renal clearance. In pregnancy, it is classified as Category C - animal studies show risk, but human data are limited. It’s only prescribed when benefits outweigh potential fetal harm. Diltiazem is not approved for children under 12; pediatric angina is rare and typically managed with other agents.
Frequently Asked Questions
Can I take Diltiazem with nitroglycerin?
Yes, many doctors prescribe both. Diltiazem provides long‑term control, while nitroglycerin is used for immediate relief. However, monitor blood pressure closely because the combo can cause a drop.
How long does it take for Diltiazem to start working?
Most patients notice reduced chest pain after 1‑2 weeks of regular dosing. Full steady‑state levels are reached in about 4‑5 days.
What should I do if I miss a dose?
Take the missed tablet as soon as you remember, unless it’s almost time for the next dose. In that case, skip the missed one - don’t double‑dose.
Are there any foods or drinks I must avoid?
Grapefruit juice can raise Diltiazem levels, increasing side‑effects. Stick to regular fruit juices and avoid alcohol excess, which can also lower blood pressure.
Can Diltiazem cause heart failure?
In patients with severe existing heart failure, non‑dihydropyridine CCBs may worsen symptoms, so doctors use caution. For most stable angina patients without significant left‑ventricular dysfunction, it’s safe.
Bottom Line
Diltiazem HCL remains a cornerstone for managing stable angina because it tackles both the supply side (widening coronary vessels) and the demand side (slowing the heart). When used correctly-right dose, proper monitoring, and awareness of interactions-it can dramatically cut the frequency of chest‑pain episodes and improve quality of life. Talk to your healthcare provider about whether Diltiazem fits into your angina‑management plan.

Carolyn Cameron
October 26, 2025 AT 16:58Undoubtedly, Diltiazem remains a cornerstone in angina management.
Holly Kress
October 27, 2025 AT 20:45While the pharmacology is clear, patients should also consider lifestyle adjustments; regular exercise and a heart‑healthy diet can synergize with medication to reduce episode frequency.
Chris L
October 29, 2025 AT 03:18For anyone starting Diltiazem, it’s helpful to track heart rate and blood pressure at home; a simple journal can alert you and your doctor to trends before they become problematic.
Charlene Gabriel
October 30, 2025 AT 12:38Diltiazem, as a non‑dihydropyridine calcium‑channel blocker, offers a dual mechanism that is especially valuable for patients juggling both angina and rhythm issues. First, by inhibiting calcium influx into vascular smooth muscle, it promotes coronary vasodilation, effectively widening the vessels that supply the myocardium. Second, its negative chronotropic effect slows the sinus node, reducing myocardial oxygen demand. When you think about why some clinicians gravitate toward it over a pure vasodilator like nifedipine, the answer often lies in that heart‑rate control. Moreover, the extended‑release formulation smooths out plasma concentrations, minimizing peaks that could provoke hypotension or reflex tachycardia. Starting doses of 60 mg once daily are modest, yet they frequently produce noticeable symptom relief within a week or two. Titration should proceed in 30‑mg increments, but only if blood pressure remains above 110/70 mmHg and the patient tolerates the initial dose without dizziness. Side‑effects such as peripheral edema or mild headaches are common, but they often abate after the first month as the body adapts. In rare cases, clinicians must watch for bradycardia below 50 bpm, especially when combined with beta‑blockers. Laboratory monitoring-particularly liver enzymes-should occur every six to twelve months because Diltiazem is metabolized hepatically via CYP3A4. Grapefruit juice should be avoided, as it can significantly increase serum levels and precipitate adverse events. If a patient needs acute relief, short‑acting nitrates can be used concurrently, but close surveillance of blood pressure is essential to prevent excessive drops. Finally, for elderly patients or those with reduced renal clearance, starting at 30 mg and titrating slowly is prudent to mitigate the risk of accumulation. In sum, Diltiazem’s blend of vasodilatory and chronotropic actions makes it a versatile tool in the cardiologist’s armamentarium, especially when angina coexists with atrial fibrillation or when beta‑blockers are contraindicated.
renee granados
November 1, 2025 AT 00:45They don’t tell you that big pharma pushes Diltiazem to keep you dependent on endless prescriptions.
Stephen Lenzovich
November 2, 2025 AT 15:38One must acknowledge that while pharmaceutical motives are complex, Diltiazem’s clinical data demonstrate genuine efficacy in reducing anginal episodes, which cannot be dismissed outright.
abidemi adekitan
November 4, 2025 AT 09:18Yo, if you’re vibing with Diltiazem, remember to keep an eye on that heart‑rate; dropping too low can make you feel like you’ve run a marathon while sitting still.
Barbara Ventura
November 6, 2025 AT 05:45Indeed-monitoring is key; check pulse every morning, before meals, and after any new activity; also, stay hydrated, avoid excessive alcohol, and keep a log-this helps your doc fine‑tune dosage.
laura balfour
November 8, 2025 AT 04:58Honestly, I think the biggest mistake is overlooking how diet can amplify the drug’s effect-like, eating too much salty food can counteract the vasodilation and leave you feeling groggy.
Ramesh Kumar
November 10, 2025 AT 06:58That’s spot on! In fact, studies show that a Mediterranean‑style diet combined with Diltiazem can improve endothelial function more than medication alone. Adding omega‑3 rich fish, nuts, and plenty of veggies helps maintain healthy arterial tone, while reducing the required dose over time.
Barna Buxbaum
November 12, 2025 AT 11:45For anyone troubleshooting side‑effects, a quick tip is to split the dose into morning and evening if you’re experiencing morning dizziness; the steadier plasma level often eases that symptom.
asha aurell
November 14, 2025 AT 19:18Split dosing can smooth peaks, reducing orthostatic drops.
naoki doe
November 17, 2025 AT 05:38Another approach worth noting is to pair Diltiazem with a low‑dose ACE inhibitor; this combo can further lower blood pressure without excessive bradycardia, but only under physician guidance.