It’s easy to think that if a drug makes you feel bad, you’re allergic to it. But that’s not always true-and mixing up side effects with true allergies can cost you more than just discomfort. It can limit your treatment options, raise your medical bills, and even put your health at risk. The difference isn’t just technical; it’s life-changing.
What Are Medication Side Effects?
Side effects are predictable, known reactions that come from how a drug works in your body. They’re not your immune system going haywire. They’re just the drug doing its job a little too well-or in the wrong place.
Take statins, for example. These drugs lower cholesterol, but they can also cause muscle aches in about 5-10% of people. That’s not an allergy. It’s the drug affecting muscle cells as a side effect of its main action. Or metformin, used for diabetes: up to 30% of users get stomach upset, diarrhea, or nausea. Again, not an immune response. Just the drug interacting with your gut.
These reactions usually show up within hours or days of starting the medication. They’re often mild and get better over time. About 70-80% of common side effects fade within two to four weeks as your body adjusts. Doctors even have tricks to manage them: taking metformin with food cuts GI side effects in 60% of people. Lowering the dose or switching to a different version of the drug can help too.
The FDA requires every prescription drug label to list side effects with exact numbers. If a drug says, “Nausea occurs in 15% of users,” that’s not a guess. It’s based on real clinical trial data. These aren’t rare surprises-they’re expected, documented, and often manageable.
What Is a True Allergic Drug Reaction?
A true drug allergy is your immune system treating the medication like a dangerous invader. It’s not about how the drug works-it’s about your body’s overreaction to it. This is where things get serious.
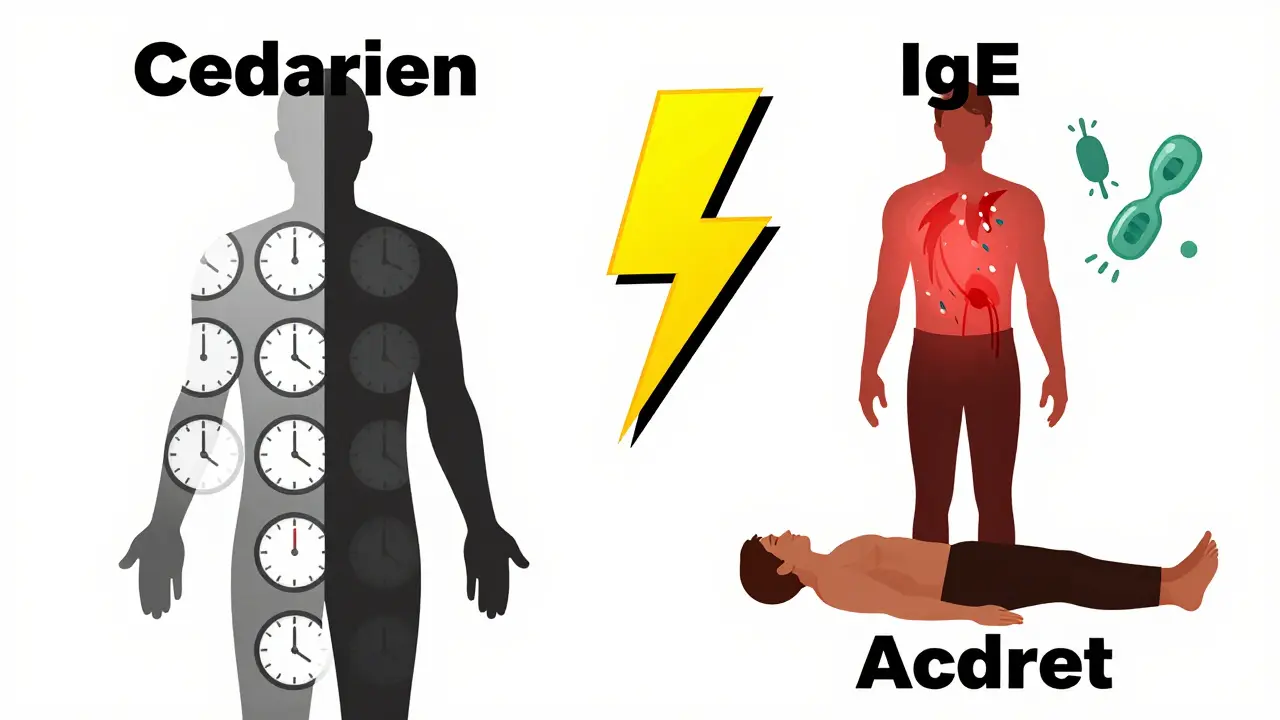
When you have a true allergy, your body produces IgE antibodies against the drug. These antibodies trigger mast cells to release histamine and other chemicals. That’s what causes hives, swelling, wheezing, or even anaphylaxis-the life-threatening reaction that shuts down your airway and drops your blood pressure.
These reactions happen fast. If you’re allergic to penicillin, symptoms like itching, rash, or trouble breathing can appear within minutes to two hours after taking it. Delayed reactions, like a skin rash that shows up a week later, are caused by T-cells, not IgE. But even those are immune-driven.
Penicillin is the most common culprit-responsible for 80% of severe drug allergies. Sulfonamides, NSAIDs like ibuprofen, and certain antibiotics also trigger allergies often. But here’s the kicker: only 5-10% of all adverse drug reactions are true allergies. The rest? Side effects.
Unlike side effects, you can’t manage an allergy with a lower dose. You have to avoid the drug completely-and often, similar ones too. For example, if you’re allergic to penicillin, you may also react to amoxicillin or other beta-lactam antibiotics. Desensitization is possible in rare cases, like when you need penicillin for a life-threatening infection, but it’s risky and only works about 70-80% of the time.
How to Tell the Difference
Here’s the quick way to tell them apart:
- Side effects are dose-related, predictable, and don’t involve your immune system. They’re listed on the drug label.
- Allergic reactions are immune-driven, can happen at any dose, and involve symptoms like hives, swelling, wheezing, or anaphylaxis.
Timing matters too. If you got a rash two weeks after starting a new antibiotic, it’s likely a delayed allergic reaction. If you got nausea the first day and it got better after a week? That’s a side effect.
Another clue: side effects often happen to many people taking the same drug. Allergies are personal. Your friend might take amoxicillin with no issues, but you break out in hives. That’s not common-it’s your immune system.
And here’s the big one: side effects can be tolerated or worked around. Allergies can’t. If you’ve ever been told you’re allergic to a drug because you got a stomach ache, you’re probably misinformed. That’s not an allergy. That’s a side effect.
Why It Matters: The Real Cost of Mislabeling
Here’s where things get dangerous. About 80-90% of people who say they’re allergic to penicillin aren’t. When doctors believe the label, they switch to broader-spectrum antibiotics like vancomycin or fluoroquinolones. These drugs are more expensive, harder on your gut, and increase your risk of dangerous infections like MRSA.
Research from Brigham and Women’s Hospital shows that mislabeling penicillin allergy adds about $4,000 per patient in extra healthcare costs each year. The American Medical Association says improper documentation of drug reactions leads to $1.5 billion in wasted spending annually.
And it’s not just money. A 2022 study in Annals of Internal Medicine found that 40% of people with mislabeled drug allergies had treatments delayed or denied because doctors thought they couldn’t use certain medications. That’s not just inconvenient-it’s life-threatening in some cases.
Dr. Elina Jerschow of the American College of Allergy, Asthma & Immunology says mislabeling side effects as allergies contributes directly to antibiotic resistance. That’s not a small problem. That’s a global health crisis.
How Doctors Test for True Allergies
If you think you’re allergic to a drug, you don’t have to live with that label forever. Testing can clear you.
For penicillin, the standard is a three-step process:
- History review-Doctors ask about timing, symptoms, and how long ago it happened. About 60% of people can be cleared just by talking.
- Skin testing-A tiny amount of the drug is placed under the skin. If you’re allergic, a red, itchy bump appears. This test is 97% accurate at ruling out penicillin allergy.
- Oral challenge-If skin testing is negative, you take a small dose under supervision. Less than 0.2% of low-risk patients react.
Newer tests like the basophil activation test (BAT) are now FDA-approved and can detect penicillin allergies with 85-95% accuracy. These are especially useful when skin testing isn’t available.
For other drugs, testing is trickier. But if your reaction was severe-like anaphylaxis or a blistering skin rash-seeing an allergist is essential. Don’t assume you’re allergic. Get tested.
What You Can Do Right Now
If you’ve ever said, “I’m allergic to this drug,” stop and think: What actually happened?
- Did you get a rash, swelling, or trouble breathing? That could be an allergy.
- Did you get a headache, nausea, or dizziness? That’s probably a side effect.
Don’t rely on memory. Many people can’t accurately recall reactions from years ago. If you’re unsure, ask your doctor for a referral to an allergist. Most insurance covers it.
Check your medical records. If your chart says “penicillin allergy” without any test results, ask: Was this ever confirmed? If not, it might be wrong.
And if you’ve avoided a drug because you thought you were allergic-don’t assume you still are. Allergies can fade. Up to 80% of people lose their penicillin allergy after 10 years without exposure.
What About Other Drugs?
Penicillin gets the most attention, but other drugs cause real allergies too:
- Sulfonamides (like Bactrim): Can cause severe skin reactions.
- NSAIDs (ibuprofen, naproxen): Can trigger asthma or hives in sensitive people.
- Chemotherapy drugs: Often cause delayed rashes that look like allergies but aren’t always immune-mediated.
- Aspirin: Can cause reactions that mimic allergies, especially in people with asthma.
But again-most reactions to these drugs are side effects. If you got a stomach ache from ibuprofen, that’s not an allergy. If you broke out in hives or your throat closed up, that’s a different story.
And don’t forget: some reactions are neither side effects nor allergies. They’re idiosyncratic-rare, unpredictable, and not well understood. These are different from both and require expert evaluation.
Final Thought: Don’t Assume. Ask.
Medications save lives. But fear of side effects-and confusion with allergies-can stop them from working when you need them most.
You don’t need to be a doctor to understand the difference. You just need to ask: Was this reaction immune-related? Was it life-threatening? Was it tested?
Getting it right means you get the right treatment. It means fewer antibiotics that hurt your gut. It means lower bills. And it means your next infection doesn’t become a crisis because you were mislabeled.
Don’t let a label from 10 years ago limit your health today. Ask for a test. Ask for clarity. Your body-and your future self-will thank you.
Can you outgrow a drug allergy?
Yes, especially with penicillin. Studies show up to 80% of people lose their penicillin allergy after 10 years without exposure. But you shouldn’t assume you’re no longer allergic. Get tested by an allergist before taking the drug again.
Is a rash always a sign of a drug allergy?
No. Many rashes from medications are side effects or non-allergic reactions. A rash that appears a week after starting a drug and isn’t itchy or swollen is often a benign reaction, not an allergy. True allergic rashes are usually raised, itchy, and appear quickly. But only testing can confirm.
Can you have an allergic reaction the first time you take a drug?
Yes. Unlike some allergies that need prior exposure, drug allergies can happen on the first dose. Your immune system may have been sensitized by something else-like a similar molecule in food or the environment-that cross-reacts with the drug.
What should I do if I think I’m having a drug allergy?
Stop taking the drug immediately. If you have trouble breathing, swelling of the face or throat, or dizziness, call emergency services. For milder reactions like a rash or itching, contact your doctor. Don’t self-diagnose. Get evaluated by an allergist to confirm whether it’s a true allergy.
Can side effects turn into allergies?
No. Side effects and allergies are different biological processes. A stomach ache from metformin won’t become an allergy. But repeated exposure to a drug can sometimes trigger a new immune response-even if you never had one before. That’s why it’s important to report any new symptoms, even if they seem minor.
Are over-the-counter drugs less likely to cause allergies?
No. Allergies can happen with any drug, even aspirin or ibuprofen. In fact, NSAIDs are among the top causes of drug allergies. Just because a drug is available without a prescription doesn’t mean it’s safer. Always pay attention to how your body reacts.
Why do so many people think they’re allergic to penicillin?
Because they had a side effect-like nausea or a mild rash-and were told it was an allergy. Many people get labeled as allergic after a childhood reaction that was never tested. Today, we know that 90% of those labels are wrong. Testing can clear you-and open up better treatment options.

kenneth pillet
January 19, 2026 AT 04:42My grandma was labeled penicillin-allergic in the 60s after a rash. Took the test last year-negative. Now she’s on the right meds for her heart. Don’t let old labels kill your options.
Pat Dean
January 19, 2026 AT 06:02Of course the medical industry wants you to think you’re allergic-it keeps you on expensive antibiotics they profit off. Wake up. They don’t care if you get MRSA because they’ll just sell you another drug.
Jay Clarke
January 20, 2026 AT 20:45Let me get this straight-we’re supposed to trust a 20-year-old doctor’s scribble on a chart more than our own body? I had a rash after amoxicillin at 8. Now I’m 34 and my skin’s fine. But nope, I’m still ‘allergic’ because bureaucracy > biology. This system is broken.
Selina Warren
January 21, 2026 AT 23:06THIS. IS. LIFE-CHANGING. I spent YEARS avoiding every antibiotic because I thought I was allergic after a stomachache from amoxicillin. Turns out? Side effect. Got tested. Now I’m not scared of penicillin anymore. I feel like I got my health back. You don’t need to live in fear-ask for the test. Seriously. Do it.
Robert Davis
January 23, 2026 AT 07:42Interesting. But have you considered that maybe the immune system is just more sensitive now because of glyphosate in the water? Or that the pharmaceutical industry has been poisoning our microbiomes for decades? The ‘side effect’ label feels like a band-aid on a hemorrhage.
Andrew McLarren
January 24, 2026 AT 10:43While the distinction between side effects and true allergic reactions is clinically vital, the real challenge lies in systemic implementation. Primary care providers often lack time, training, or access to allergists to properly evaluate patient-reported reactions. Until standardized protocols and reimbursement structures are established, mislabeling will persist as a structural, not merely individual, failure.
christian Espinola
January 26, 2026 AT 02:59Penicillin allergy? 90% false. But who benefits? The CDC? Pharma? The hospital billing department? Look at the numbers: $1.5 billion wasted annually. Coincidence? Or is this a feature, not a bug? They don’t want you to know you can get tested. They want you afraid. Stay vigilant.
Chuck Dickson
January 27, 2026 AT 08:13Hey, if you’ve ever been told you’re allergic to a drug because you got a little nausea or a rash-please, go get tested. Seriously. It’s not scary. It’s not expensive. And it could save your life next time you’re sick. I did it. My doctor laughed, but I got cleared. Now I take meds like a normal human. You can too.
Naomi Keyes
January 27, 2026 AT 09:41Let’s be precise: the term ‘allergy’ is misused in 80–90% of cases, as cited by the American College of Allergy, Asthma & Immunology. Yet, medical records are immutable, and clinicians rely on them-often without questioning. This is not anecdotal; it’s a documented, systemic diagnostic error with quantifiable morbidity and mortality implications. You are not ‘allergic’ to ibuprofen because you got a headache. You experienced a pharmacological side effect. Please, update your chart.
Jodi Harding
January 29, 2026 AT 06:08My mom got labeled allergic after a rash. Turned out it was the dye in the pill. Not the drug. Now she’s on a different brand. No test needed. Just common sense.
Stacey Marsengill
January 30, 2026 AT 15:28I used to be the person who said, ‘I’m allergic to everything.’ Then I got a rash after a Z-pack and panicked. Turns out? It was stress + heat + the antibiotic. All three. I cried when the allergist told me I wasn’t allergic. I’d spent ten years avoiding meds like they were poison. I’m still mad. But now I’m free.
Aysha Siera
February 1, 2026 AT 14:03They’re hiding something. Why do they make testing so hard? Why do they keep pushing expensive antibiotics? Who owns the labs? Who profits when you get MRSA? Think about it.
rachel bellet
February 2, 2026 AT 11:34It’s not merely a diagnostic misclassification-it’s a pathological failure of epistemic humility within clinical practice. The conflation of pharmacodynamic adverse effects with immunoglobulin E-mediated hypersensitivity reflects a profound epistemological deficit in primary care education, perpetuated by institutional inertia and a lack of standardized allergological triage protocols. The result? A cascade of iatrogenic harm driven by diagnostic laziness.