
Medication Cost-Saving Calculator
Estimated Savings
Medication costs are rising faster than almost any other part of healthcare. In Australia, prescription drug spending climbed by 9.4% in 2023 alone, according to the Pharmaceutical Benefits Scheme. Yet, cutting corners on medication safety doesn’t just risk lives-it can cost hospitals and patients far more in the long run. A single preventable medication error can lead to extended hospital stays, legal claims, or even death. The good news? You don’t have to choose between saving money and keeping patients safe. In fact, the smartest cost-saving moves are the ones that make medication use safer.
Start with Generic Medications
Generic drugs are not second-rate. They contain the same active ingredients, work the same way, and meet the same strict quality standards as brand-name drugs. Yet they cost 30% to 80% less. In the U.S., 82.2% of patients already use generics. In Australia, the PBS encourages their use by lowering co-payments. Switching a patient from a brand-name statin like Lipitor to its generic version, atorvastatin, can save over $1,200 per year per person. That’s money that stays in the patient’s pocket and reduces pressure on public health budgets.
But here’s the catch: not all generics are created equal. For drugs with a narrow therapeutic index-like warfarin, levothyroxine, or phenytoin-small differences in absorption can cause harm. That’s why pharmacists must verify bioequivalence and monitor patients closely after switching. When done right, switching to generics reduces costs without a single added risk.
Use Pharmacist-Led Medication Reviews
Imagine a hospital where a pharmacist sits with every patient on rounds, not just to check prescriptions, but to ask: Are you still taking this? Does it make sense? Are you having side effects? That’s not a luxury-it’s a cost-saver.
A 390-bed community hospital in Victoria found that daily pharmacist-led medication reviews cut 30-day readmissions by 38%. Each avoided readmission saved about $5,652. That’s not just a win for the budget-it’s a win for the patient. These pharmacists didn’t just catch duplicate prescriptions. They spotted drugs that were no longer needed, identified harmful interactions, and caught dosing errors before they caused harm.
Studies from Walter Reed Army Medical Center show that every dollar spent on clinical pharmacists returns $6.03 in savings. That’s because pharmacists don’t just count pills-they change outcomes. They reduce hospital stays, prevent emergency visits, and stop costly complications before they start.
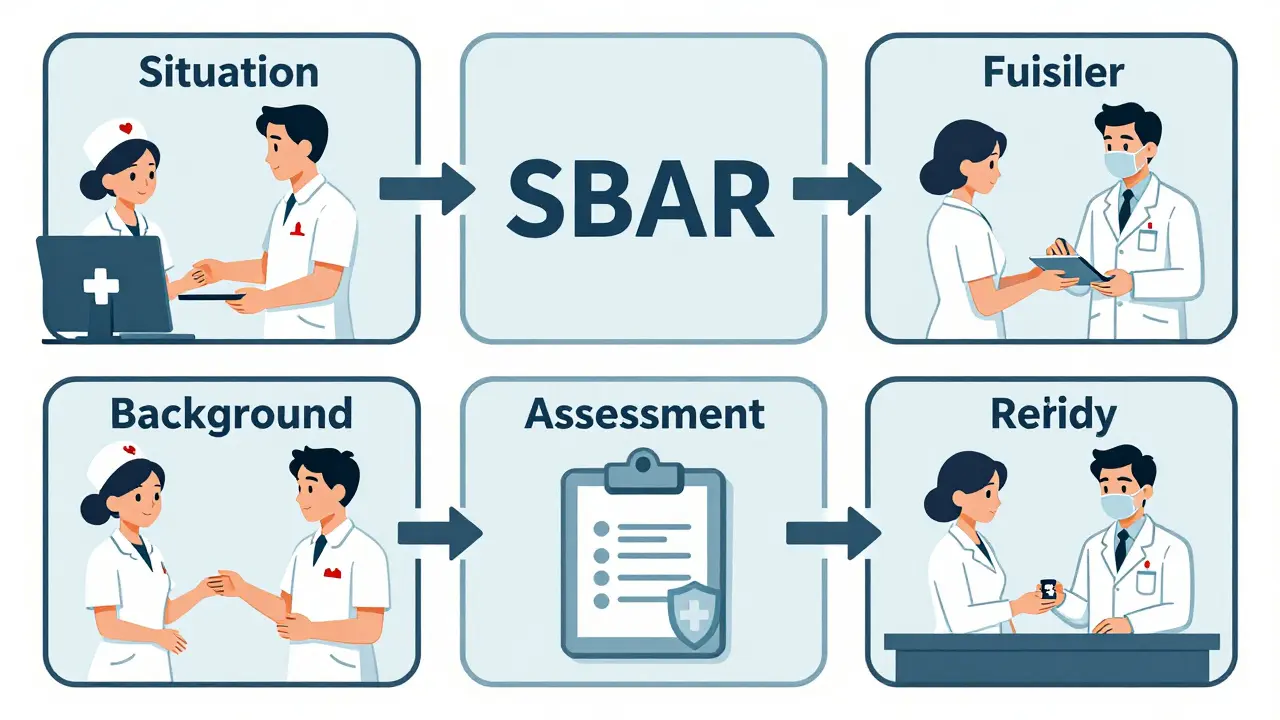
Adopt SBAR for Clear Communication
One of the most dangerous moments in a hospital is when a patient moves from one team to another. That’s when information gets lost. A simple tool called SBAR (Situation-Background-Assessment-Recommendation) fixes this. It’s not fancy. It’s just a structured way to hand off patient info.
One Sydney hospital implemented SBAR for all medication transitions. Within six months, medication-related adverse events dropped by 50%. The cost? A few hours of training. No new software. No expensive hardware. Just better communication.
Nurses and pharmacists who use SBAR report fewer misunderstandings. Doctors get clearer requests. Patients get safer care. And hospitals save money by avoiding preventable errors. It’s one of the lowest-cost, highest-impact safety strategies available.
Switch to Ready-to-Administer (RTA) Products
Preparing IV medications manually takes time, increases risk, and leads to waste. A nurse might draw up a dose, spill some, or misread the label. RTA products-pre-measured, pre-mixed medications in ready-to-use containers-eliminate those risks.
A Melbourne hospital switched 12 common IV drugs to RTA packaging. They saw a 30% drop in preparation errors and a 22% reduction in drug waste. Even though RTA products cost 15-20% more upfront, they saved the hospital over $200,000 in a year by reducing nursing time, avoiding adverse events, and cutting waste.
It’s counterintuitive: paying more per unit saves money overall. But when you factor in labor, error-related care, and lost time, RTA products pay for themselves.
Embrace Antimicrobial Stewardship
Antibiotics are one of the most overused-and misused-classes of drugs. Giving the wrong one, for too long, or at the wrong dose doesn’t just waste money-it breeds superbugs.
Antimicrobial Stewardship Programs (AMS) use pharmacists to review antibiotic orders daily. They ask: Is this really needed? Can we switch from IV to oral? Can we stop it early? A hospital in Adelaide cut its antibiotic use by 28% in 12 months. That saved $2 million in drug costs alone. But the real win? A 40% drop in C. difficile infections, which cost hospitals over $15,000 per case to treat.
AMS doesn’t mean withholding antibiotics. It means using them smarter. And that’s where pharmacists make the difference.
Use Technology Wisely-But Don’t Rely on It Alone
Barcode scanning, e-prescribing, and automated dispensing systems help. Barcode systems reduce administration errors by 41%. E-prescribing cuts prescribing errors by 55%. But they’re not magic.
A hospital in Perth installed a new e-prescribing system. Errors dropped-but not as much as expected. Why? Because the system didn’t catch a doctor prescribing two drugs that interact dangerously. A pharmacist on the team spotted it. Technology reduces errors. People prevent them.
The best systems combine tech with clinical judgment. A pharmacist reviewing a patient’s full medication list can spot a problem no algorithm will catch-like a drug that’s no longer needed, or a dose that’s too high for an aging kidney.
Involve Patients in Their Own Safety
Patients aren’t passive recipients of care. They’re key players in safety. Studies show that 37.5% of patients use mail-order pharmacies to save money. 29.8% get free samples. 39.6% use at least one cost-saving strategy.
But many don’t know how to ask the right questions. Teach patients to ask: Is there a cheaper version? Do I really need this? What happens if I skip it?
Hospitals that give patients printed medication lists, teach them to check their pills against the label, and encourage them to bring all their meds to appointments see better adherence and fewer errors. A simple conversation can prevent a trip to the ER.

What Happens When You Cut Corners?
Some hospitals try to save money by cutting pharmacy staff. One hospital in Queensland reduced its pharmacy technicians by 30%. Three months later, medication errors jumped 22%. The cost? $1.2 million in extended stays and legal fees.
Another tried to save by switching all drugs to the cheapest generic-even for narrow therapeutic index drugs. Patients had seizures. Others had strokes. The hospital paid out settlements and lost its accreditation.
Cost-cutting without safety is not smart. It’s dangerous. And it always costs more in the end.
What Works Best?
The most successful hospitals combine:
- Pharmacist-led medication reviews
- SBAR for handoffs
- RTA packaging for high-risk drugs
- Antimicrobial stewardship
- Generic substitution with monitoring
- Patient education
These aren’t just safety tools. They’re financial tools. Together, they reduce waste, prevent errors, and cut readmissions. The result? Lower costs and better outcomes.
Looking Ahead
The Australian government is investing in pharmacist-led care models. The Medicare Benefits Schedule now funds medication reviews for high-risk patients. The federal government’s 2025 health budget includes funding for clinical pharmacists in aged care and rural clinics.
By 2027, experts predict that 75% of Australian hospitals will have pharmacists embedded in care teams. That’s not because it’s trendy. It’s because it works.
Can switching to generic drugs really be safe?
Yes-when done correctly. Generic drugs must meet the same standards as brand-name drugs. For most medications, they’re identical in effectiveness and safety. But for drugs like warfarin or thyroid hormones, even small differences in absorption can matter. That’s why pharmacists monitor patients closely after switching. With proper oversight, generics are not only safe-they’re the smartest way to cut costs.
Do pharmacist-led programs cost too much to implement?
The upfront cost of hiring pharmacists may seem high, but the return is clear. Every dollar invested in clinical pharmacists returns $6.03 in savings, according to studies from Walter Reed and the Journal of the American College of Clinical Pharmacy. Savings come from fewer hospital readmissions, less drug waste, and lower rates of adverse events. In fact, hospitals that cut pharmacy staff to save money often end up spending far more later on due to errors and complications.
Are RTA products worth the higher price?
Yes, if you look at the full picture. RTA products cost more per unit, but they save time, reduce errors, and cut waste. One hospital saved $200,000 in a year by switching to RTA IV drugs-even after paying more for the products. Nurses spent less time preparing doses, and there were zero preparation-related errors. When you factor in labor costs and avoided complications, RTA products pay for themselves.
Can patients really help prevent medication errors?
Absolutely. Patients who know their medications, ask questions, and bring all their pills to appointments make fewer mistakes. Studies show that when patients are educated and involved, medication errors drop by up to 30%. Simple actions-like checking the name on the label or asking if a drug is still needed-can prevent serious harm.
Why do some hospitals fail at cost-saving and safety?
They focus only on the price tag, not the full cost. Cutting staff, skipping pharmacist reviews, or forcing generic switches without monitoring may look cheaper on paper. But they lead to errors, readmissions, lawsuits, and lost trust. The hospitals that succeed treat safety as an investment-not an expense. They use data, involve frontline staff, and let pharmacists lead.
The future of healthcare isn’t about choosing between affordability and safety. It’s about building systems where safety is the most cost-effective strategy. The tools are here. The evidence is clear. The only question is: who will act first?

Gloria Ricky
February 11, 2026 AT 12:53OMG this post is everything. I work in a clinic and we switched to generics last year-like, holy cow, the savings were insane. One lady was on $800/month for her blood pressure med, switched to generic, now pays $12. She cried. I cried. We all cried. And no side effects. Like, who knew saving money could feel this good? 🙌
Jason Pascoe
February 11, 2026 AT 19:10As an Aussie pharmacist, I can confirm-PBS generics work. We’ve been doing this for years. The key is not just switching, but monitoring. I’ve seen patients on levothyroxine go from 100mcg to 112mcg because the generic brand had slightly different fillers. Not a big deal if you’re tracking TSH. But if you don’t? Yeah. That’s where things go sideways. Pharmacists aren’t just pill counters-we’re safety nets.
Sonja Stoces
February 13, 2026 AT 04:51LMAO ‘smartest cost-saving moves are the ones that make medication use safer’? 🤡 Come on. This is just corporate speak for ‘we’re gonna make you pay more for the same thing under a different name.’ RTA products cost 20% more? That’s a scam. Nurses are already overworked-why not just hire more? Oh wait, that’d cost money. This whole post is a sales pitch for pharmacy vendors disguised as public health advice. #WakeUp
Annie Joyce
February 14, 2026 AT 14:31Let me tell you about the time I caught a med error on a 78-year-old man on three antihypertensives-two of which were duplicates, one was for a condition he’d had surgery to fix 3 years prior. The doc didn’t even notice. I flagged it. The pharmacist said, ‘Good catch, Annie.’ We switched him to two meds, saved $300/month, and he stopped feeling like a zombie. That’s the magic. Not tech. Not generics. It’s a human being who actually looks at the chart. And yeah, that’s why pharmacist-led reviews aren’t ‘nice to have’-they’re the backbone of safe, affordable care. 🏥💙
Luke Trouten
February 16, 2026 AT 00:39There’s a deeper philosophical point here that deserves more attention: safety as an investment, not an expense. We live in a culture that treats cost-cutting as a virtue, even when it’s self-defeating. But if you look at systems theory, you’ll see that every intervention mentioned here-SBAR, RTA, AMS-isn’t just reducing errors, it’s reinforcing system resilience. That’s not just fiscal wisdom. It’s epistemological humility. We stop pretending we can outsource care to algorithms or cheap generics, and instead invest in the human infrastructure that actually understands context. That’s the real paradigm shift.
Kristin Jarecki
February 16, 2026 AT 22:45While the general thrust of this article is commendable, it is imperative to underscore that the implementation of pharmacist-led initiatives must be accompanied by rigorous outcome metrics and longitudinal data tracking. The cited figures, while encouraging, lack methodological transparency regarding control groups, confounding variables, and statistical significance. Furthermore, the assertion that RTA packaging yields net savings must be contextualized within regional supply chain dynamics and formulary constraints. A one-size-fits-all approach risks unintended consequences in underserved or rural settings where logistics may not support such procurement models. Rigorous evaluation remains non-negotiable.
Jonathan Noe
February 18, 2026 AT 14:17Y’all are underestimating the power of tech. I’ve seen hospitals go all-in on barcode scanning and e-prescribing and cut staff. Guess what? Errors dropped 60%. Pharmacists? Still there, but now they’re doing clinical work instead of counting pills. SBAR? Cute. But if you’ve got an AI that auto-suggests alternatives based on drug interactions, patient history, and lab values? That’s the future. You don’t need a pharmacist to catch every error-just one who’s overseeing the system. And yeah, I said it-tech > humans. Sorry not sorry.
Suzette Smith
February 20, 2026 AT 06:24Wait, so you’re saying we should pay MORE for RTA products to save money? That’s like buying a $1000 mattress to avoid back pain. I’m not buying it. 😅