
Diabetes Medication Comparison Tool
Which Medication Is Right for You?
Compare key features of common diabetes medications including Precose (acarbose) and alternatives. Select up to 3 medications to view a side-by-side comparison.
Select Medications to Compare
Comparison Results
Select up to 3 medications to view comparison.
Managing type 2 diabetes isn’t just about taking a pill-it’s about finding the right one that fits your life, your body, and your daily routine. Precose (acarbose) has been around for decades as an alpha-glucosidase inhibitor, slowing down how fast your body breaks down carbs to keep blood sugar from spiking after meals. But is it still the best choice today? With newer drugs, better side effect profiles, and more options on the shelf, many people are asking: what else is out there?
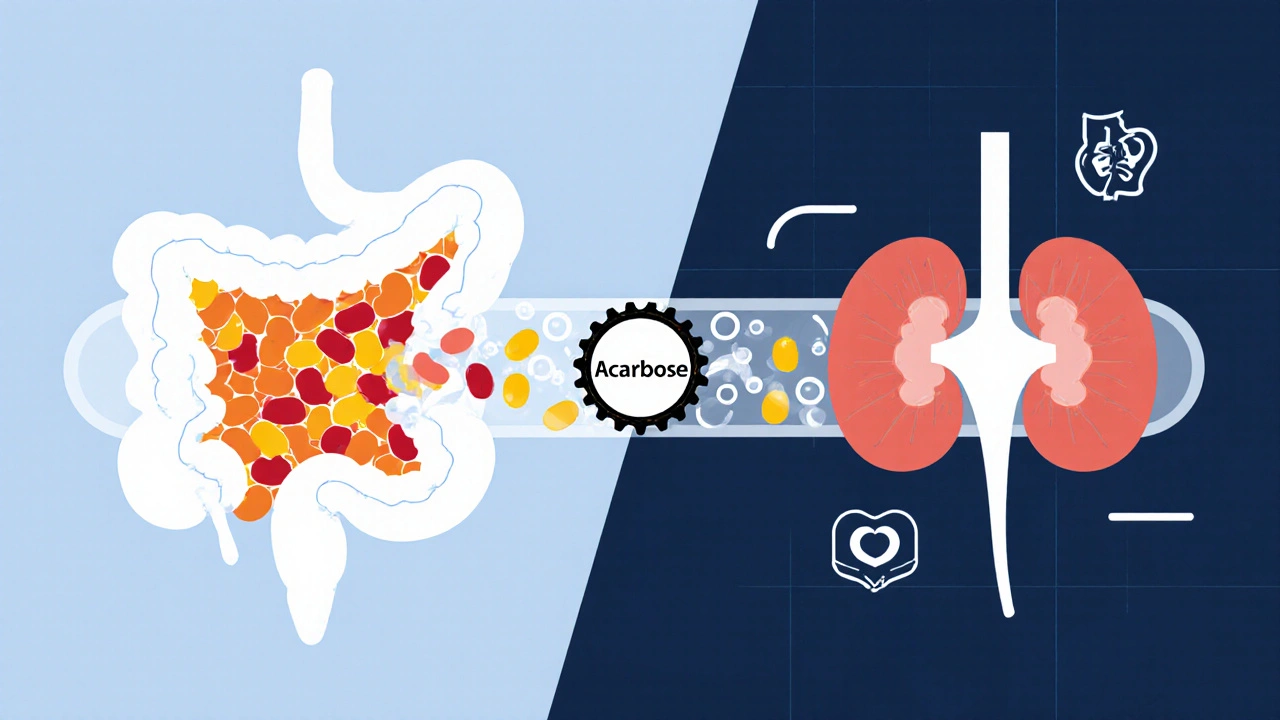
How Precose (Acarbose) Works
Precose doesn’t make your body produce more insulin or make cells more sensitive to it. Instead, it blocks enzymes in your small intestine-alpha-glucosidase-that break down complex carbs into simple sugars like glucose. This means carbs pass through your gut slower, so glucose enters your bloodstream gradually instead of all at once. That helps avoid those sharp post-meal spikes that can be hard to manage.
It’s taken right before meals, usually three times a day. The starting dose is low-25 mg-and slowly increased based on tolerance and blood sugar results. Most people end up on 50 to 100 mg per meal. It works best with meals that contain carbohydrates, so it’s not useful if you’re eating a low-carb diet.
Studies show Precose can lower HbA1c by about 0.5% to 1%. That’s modest compared to some newer drugs, but it’s consistent and doesn’t cause weight gain or low blood sugar on its own. The catch? It’s hard on the gut.
Common Side Effects of Precose
If you’ve ever taken Precose, you know why many people stop. Gas, bloating, stomach cramps, and diarrhea are common-up to 70% of users report them, especially in the first few weeks. These side effects happen because undigested carbs reach your colon, where bacteria ferment them, producing gas. The good news? They usually improve over time as your gut adjusts. The bad news? For some, they never go away.
Some people try to reduce side effects by cutting back on carbs, but that defeats the purpose of the drug. Others switch to a different medication entirely. If you’re someone who eats a lot of rice, bread, or pasta, Precose might be a tough fit.
Alternatives to Precose: What’s Available Now
Since Precose came out in the 1990s, diabetes treatment has changed dramatically. Today, there are at least six major classes of oral and injectable medications with better side effect profiles and stronger results. Here are the most common alternatives.
Metformin: The First-Line Standard
Metformin is still the most prescribed drug for type 2 diabetes worldwide. It works by reducing sugar production in the liver and improving insulin sensitivity. Unlike Precose, it doesn’t cause gas or bloating. Instead, its main side effects are mild nausea and diarrhea-usually temporary and manageable with extended-release versions.
Metformin lowers HbA1c by 1% to 2%, helps with weight loss (not gain), and has been linked to lower heart disease risk. It’s cheap, widely available, and recommended as the first step by the American Diabetes Association. If you haven’t tried metformin yet, it’s usually the place to start.
SGLT2 Inhibitors: Canagliflozin, Dapagliflozin, Empagliflozin
These drugs make your kidneys flush out extra sugar through urine. They’re called SGLT2 inhibitors. They don’t just lower blood sugar-they also help with weight loss and reduce the risk of heart failure and kidney disease.
Empagliflozin, for example, showed a 38% drop in heart-related deaths in high-risk patients in the EMPA-REG OUTCOME trial. Dapagliflozin and canagliflozin have similar results. Side effects include yeast infections and increased urination, but these are usually mild. Unlike Precose, these drugs work regardless of what you eat.
GLP-1 Receptor Agonists: Semaglutide, Liraglutide, Dulaglutide
These are injectables, but they’re now the most powerful tools for blood sugar control and weight loss. Semaglutide (Ozempic, Wegovy) can lower HbA1c by up to 1.8% and help people lose 10-15% of their body weight. That’s more than any other oral drug.
They mimic a natural hormone that slows digestion, reduces appetite, and tells the pancreas to release insulin only when needed. Side effects include nausea and vomiting, especially at first, but these often fade. They’re more expensive than Precose, but many insurance plans cover them now for people with heart disease or obesity.
DPP-4 Inhibitors: Sitagliptin, Saxagliptin, Linagliptin
These are oral pills that boost your body’s own GLP-1 hormone. They’re mild-lower HbA1c by 0.5% to 0.8%-but they’re weight-neutral and don’t cause low blood sugar unless combined with insulin or sulfonylureas.
Sitagliptin is one of the most prescribed. It’s well tolerated, with no major gut issues. If you can’t handle the gas from Precose but need something gentler than metformin, this could be a good middle ground.
Sulfonylureas: Glimepiride, Glyburide
These older drugs force your pancreas to release more insulin. They’re cheap and effective-lowering HbA1c by 1% to 2%-but they carry a high risk of low blood sugar (hypoglycemia), especially in older adults or those with irregular meals.
They also cause weight gain. For someone trying to lose weight or avoid low blood sugar episodes, these are rarely the first choice anymore. But in low-income settings or when cost is the main barrier, they’re still used.
Thiazolidinediones: Pioglitazone
Pioglitazone makes cells more sensitive to insulin. It lowers HbA1c by about 1% and has a long-lasting effect. But it can cause weight gain, fluid retention (leading to swelling or heart failure in some), and a small increased risk of bladder cancer.
It’s rarely used today unless other options have failed and the patient has no heart or bladder issues.
Comparison Table: Precose vs. Top Alternatives
| Medication | Class | HbA1c Reduction | Weight Effect | Common Side Effects | Cardiovascular Benefit | Cost (Monthly, AUD) |
|---|---|---|---|---|---|---|
| Precose (Acarbose) | Alpha-glucosidase inhibitor | 0.5%-1% | Neutral | Gas, bloating, diarrhea | No proven benefit | $25-$40 |
| Metformin | Biguanide | 1%-2% | Loss | Nausea, diarrhea (usually mild) | Possible benefit | $5-$15 |
| Empagliflozin | SGLT2 inhibitor | 0.7%-1% | Loss (2-4 kg) | Yeast infections, frequent urination | Yes (reduced heart death) | $80-$120 |
| Semaglutide | GLP-1 agonist | 1.5%-1.8% | Loss (5-10 kg) | Nausea, vomiting (improves over time) | Yes | $150-$200 |
| Sitagliptin | DPP-4 inhibitor | 0.5%-0.8% | Neutral | Headache, mild upper respiratory | Neutral | $90-$130 |
| Glimepiride | Sulfonylurea | 1%-2% | Gain | Low blood sugar, weight gain | No proven benefit | $10-$20 |
Who Should Stick With Precose?
Precose isn’t dead. It still has a place-for specific people. If you’re someone who:
- Eats high-carb meals regularly (rice, noodles, bread, potatoes)
- Can’t tolerate metformin due to stomach issues (and don’t want injections)
- Want to avoid weight gain or low blood sugar
- Have access to low-cost generics and can tolerate the gas
Then Precose might still be a reasonable option. Some older patients in rural areas use it because it’s cheap and doesn’t require frequent blood sugar checks.
But if you’re young, active, or trying to lose weight, or if you’re already on multiple medications, Precose adds complexity without much benefit.
When to Consider Switching
Consider switching from Precose if:
- Your side effects haven’t improved after 3 months
- Your HbA1c is still above 7% despite taking the max dose
- You’re struggling to stick with your diet because of bloating
- You have heart disease, kidney issues, or obesity-options like SGLT2 inhibitors or GLP-1 agonists offer proven protection
Don’t stop Precose suddenly. Talk to your doctor. You might need to switch gradually to avoid blood sugar swings.
Real-World Experience: What Patients Say
One patient in Brisbane, 62, switched from Precose to metformin after six months of constant bloating. "I could eat a bowl of pasta without feeling like my stomach was going to explode. My HbA1c didn’t go up-it actually dropped a bit. Why didn’t I switch sooner?"
Another, a 48-year-old teacher in Melbourne, tried semaglutide after failing with metformin and sitagliptin. "I lost 11 kg in four months. My energy is better. I don’t think about food as much. I didn’t expect that from a diabetes drug."
These aren’t outliers. They’re common stories now. The diabetes toolkit has expanded. You don’t have to live with gas and discomfort if there’s a better way.
Final Thoughts: It’s Not One Size Fits All
Precose was a step forward in the 90s. Today, it’s a relic for some, a last resort for others. The goal isn’t just to lower blood sugar-it’s to do it safely, comfortably, and with long-term health in mind.
If you’re on Precose and it’s working without major side effects, great. But if you’re struggling, it’s worth having a conversation with your doctor about alternatives. There are now options that do more than just slow carbs-they protect your heart, help you lose weight, and let you eat without fear.
Your diabetes management should fit your life-not the other way around.
Is Precose still used today?
Yes, but rarely as a first choice. Precose is still prescribed in some cases, especially for people who eat high-carb diets and can’t tolerate metformin or don’t want injectables. However, newer drugs with better side effect profiles and added health benefits are now preferred by most doctors.
Does Precose cause low blood sugar?
No, Precose alone doesn’t cause low blood sugar (hypoglycemia). It works by slowing carb digestion, not by increasing insulin. But if you take it with insulin or sulfonylureas, you can still get low blood sugar. In that case, you need to treat it with glucose tablets or juice-not regular sugar, because Precose blocks the breakdown of table sugar.
Can I take Precose with metformin?
Yes, many people take both together. Metformin reduces liver sugar output, and Precose slows carb absorption. Together, they can give better blood sugar control than either alone. But combining them increases the risk of stomach side effects like gas and diarrhea. Starting with low doses and increasing slowly helps.
Are there natural alternatives to Precose?
No natural supplement works like Precose. Some herbs like cinnamon or berberine may slightly lower blood sugar, but they don’t block carb-digesting enzymes. They’re not regulated like prescription drugs, and their effects are inconsistent. Don’t replace Precose with supplements without talking to your doctor.
Why is Precose cheaper than newer drugs?
Precose is a generic drug that’s been around for decades. Its patent expired long ago, so many manufacturers make it, driving the price down. Newer drugs like semaglutide and SGLT2 inhibitors are still under patent protection or have limited generic versions, making them much more expensive.
What’s the best alternative to Precose for someone with kidney problems?
Metformin is often avoided in advanced kidney disease. In that case, DPP-4 inhibitors like linagliptin or GLP-1 agonists like semaglutide are safer options. SGLT2 inhibitors also have kidney benefits but require monitoring. Always check kidney function before starting any new diabetes drug.
Can Precose help with prediabetes?
Yes, studies show Precose can delay or prevent the progression from prediabetes to type 2 diabetes, especially in people with high post-meal glucose spikes. But lifestyle changes-weight loss and exercise-are still the most effective first step. Precose is sometimes used if lifestyle changes aren’t enough.
If you’re on Precose and feeling stuck, don’t assume it’s your only option. Diabetes care has evolved. There are now treatments that don’t just manage blood sugar-they improve your overall health. Talk to your doctor. Ask about alternatives. Your next step might be simpler-and more comfortable-than you think.

Shiv Sivaguru
October 29, 2025 AT 09:49Precose? Bro, I took that for 3 months and my gut sounded like a balloon factory during a heatwave. I switched to metformin and now I can eat biryani without feeling like I’m about to explode. Why do doctors still push this ancient relic?!
Gavin McMurdo
October 30, 2025 AT 21:28Oh, so now we’re romanticizing 1990s pharmacology? Let me get this straight-you’d rather have your colon stage a protest than take a GLP-1 agonist that literally saves lives? I mean, sure, if you think ‘gas’ is a valid trade-off for ‘not dying of heart failure.’
Jesse Weinberger
October 31, 2025 AT 10:44metformin is just a gateway drug to big pharma. They made it cheap so you’d get hooked. Then they hit you with the $200 ozempic. It’s all a scam. Precose is the only real medicine. The FDA is in bed with the pharma giants. I’ve read the studies. They’re faked. Also, I eat keto now so I don’t need any of this.
Emilie Bronsard
November 1, 2025 AT 04:48I switched from Precose to semaglutide last year. The nausea was rough at first, but the weight loss and energy boost were worth it. No more bloating after lunch. Just… peace.
John Bob
November 2, 2025 AT 09:17Are you aware that SGLT2 inhibitors have been linked to Fournier’s gangrene? The FDA has issued multiple warnings. Yet you’re casually recommending them like they’re Advil? This isn’t medicine-it’s corporate roulette.
Alex Grizzell
November 3, 2025 AT 07:46Metformin changed my life. No more post-meal crashes. No more bloating. Just steady energy. I wish I’d known sooner. Seriously, if you’re still on Precose and it’s killing your digestion-talk to your doc. You deserve better
George Johnson
November 5, 2025 AT 06:56Classic. Guy writes a 2000-word essay on diabetes meds, and the comments are just people screaming about their guts. We’ve all been there. I still dream about that one time I ate naan and immediately regretted every life choice.
Rodrigo Ferguson
November 6, 2025 AT 17:28It is profoundly disconcerting to observe the contemporary medical establishment’s capitulation to pharmaceutical marketing imperatives. The elevation of GLP-1 agonists as panaceas-while ignoring the long-term epigenetic implications and the erosion of metabolic autonomy-is not therapeutic; it is totalitarian.
Mickey Murray
November 8, 2025 AT 04:45People act like Precose is some villain, but let’s be real-you’re the one eating pizza at 11pm and then wondering why your blood sugar’s in the stratosphere. No drug fixes bad habits. Metformin? Sure. Ozempic? Maybe. But you still gotta stop eating like a raccoon in a dumpster.
Kevin McAllister
November 8, 2025 AT 21:12Who the hell wrote this? Big Pharma shill? They didn’t mention the fact that SGLT2 inhibitors cause amputations! And GLP-1s? They’re making people lose so much weight they look like skeletons! This isn’t healthcare-it’s a eugenics experiment disguised as science!
Marcia Martins
November 9, 2025 AT 17:11My dad was on Precose for years. He hated it. When he switched to sitagliptin, he said he felt like he could breathe again. I’m so glad he listened to his doctor. Sometimes the best medicine is just… less misery.
Robert Bowser
November 10, 2025 AT 07:52There’s no one-size-fits-all. I’ve tried metformin, Precose, and now I’m on a low-dose SGLT2. Each had pros and cons. The key is working with your doctor, tracking your numbers, and not letting fear or hype drive your choices. It’s a marathon, not a sprint.