Chronic pancreatitis isn't just a diagnosis-it's a daily battle. For most people living with it, pain doesn't come and go. It waits. It pulses under the ribs. It flares after meals, after stress, sometimes even at 3 a.m. And it doesn’t care if you’ve taken your pills, eaten your bland food, or avoided alcohol for years. This isn’t a condition you recover from. It’s one you learn to live with-by understanding how to control the pain, how enzymes really work, and what your body actually needs to survive.
Pain That Doesn’t Quit
Eight out of ten people with chronic pancreatitis have ongoing pain. Not occasional discomfort. Not a bad day after a fatty meal. Constant, deep, burning pain that can last for hours or days. It’s not just in the belly-it radiates to the back. It wakes you up. It makes you cancel plans. It turns groceries into a chore and work into a nightmare. The first step in managing this pain isn’t strong drugs. It’s starting low. Acetaminophen (paracetamol) at 4,000 mg a day is the baseline. It’s not magic, but for mild cases, it cuts pain by 30-40%. If that fails, doctors turn to gabapentin or pregabalin. These aren’t painkillers in the traditional sense. They calm overactive nerves. One patient in Sydney told me, “After eight different meds, gabapentin at 2,400 mg a day was the first thing that didn’t make me feel like I was drowning.” For moderate to severe pain, tramadol is often the go-to opioid. It’s less addictive than oxycodone, but still carries risks. About one in four people get nausea or constipation from it. That’s why many avoid it until they have no other choice. And that’s the problem: too many wait too long. Antidepressants like amitriptyline, usually prescribed for depression, are surprisingly effective for nerve-related pain. Doses as low as 10 mg at night can reduce pain by half for some. It’s not about mood-it’s about how the brain processes pain signals. NSAIDs like ibuprofen? Avoid them. They can damage your kidneys and gut, both already stressed from pancreatitis. And while opioids might seem like the answer, 25-30% of long-term users develop dependence. That’s why specialists now push for non-drug options: yoga, acupuncture, and even cognitive behavioral therapy (CBT) have shown real results. One study found biweekly yoga improved quality of life by 35% over 12 weeks.Enzyme Therapy: More Than Just Pills
Your pancreas used to make digestive enzymes. Now it doesn’t. That means food doesn’t break down. Fat passes through undigested-greasy stools, bloating, weight loss. That’s where pancreatic enzyme replacement therapy (PERT) comes in. You don’t just take enzymes when you feel bloated. You take them with the first bite of every meal. Miss the timing, and they’re useless. A typical dose is 25,000 to 80,000 lipase units per meal. That’s not one pill. That’s often six to twelve, depending on how fatty the meal is. A steak dinner? You’ll need more than a salad. Brands like Creon, Zenpep, and Pancreaze are the main options. But they’re expensive-$300 to $1,200 a month. Insurance often fights coverage. Many patients skip doses because they can’t afford it. That’s a mistake. Studies show high-dose PERT reduces pain in 45% of people-not because it treats pain directly, but because undigested fat triggers inflammation in the pancreas. Less fat floating around = less flare-ups. If you’re on a non-enteric coated enzyme, you also need a proton pump inhibitor (PPI) like omeprazole. Why? Stomach acid kills the enzymes before they reach the intestine. PPIs shut down acid production so the enzymes can do their job. It’s a two-part system: enzyme + acid blocker. And here’s the catch: PERT works best in early-stage disease. If your pancreas is already scarred and shriveled, enzymes help less. That’s why starting early matters. Waiting until you’re losing weight and getting jaundiced means you’ve already lost ground.Nutrition: What to Eat, What to Avoid
There’s no one-size-fits-all diet for chronic pancreatitis. But there are rules. First, fat. Most guidelines recommend 40-50 grams a day. That’s not zero fat-it’s smart fat. Avoid fried food, butter, cream, fatty meats. But you still need fat. Medium-chain triglycerides (MCTs) are the exception. They don’t need pancreatic enzymes to digest. You’ll find them in specialized formulas like Peptamen or in MCT oil you can add to smoothies. One small study showed patients who drank three cans of MCT formula daily for ten weeks cut their pain by 30%. Second, protein. You need it to repair tissue and prevent muscle loss. Lean chicken, fish, tofu, eggs. Avoid heavy sauces. Grill or steam instead of frying. Third, vitamins. Fat-soluble vitamins A, D, E, and K are almost always low. You’ll need supplements-high-dose, taken with your enzymes. A blood test every six months will tell you if you’re still deficient. Antioxidants? There’s real data here. A daily mix of selenium (100 mcg), vitamin C (180 mg), vitamin E (90 mg), beta-carotene (1.5 mg), and methionine (400 mg) reduced pain in over half of patients in a six-month trial. It’s not a cure. But for some, it’s the difference between tolerable and unbearable. And then there’s alcohol and smoking. No gray area here. If you’re still drinking, your pain won’t get better. Ever. Quitting cuts pain by 40-50% within six months. Smoking? It doubles your risk of complications and makes pain worse. Quitting isn’t optional-it’s survival.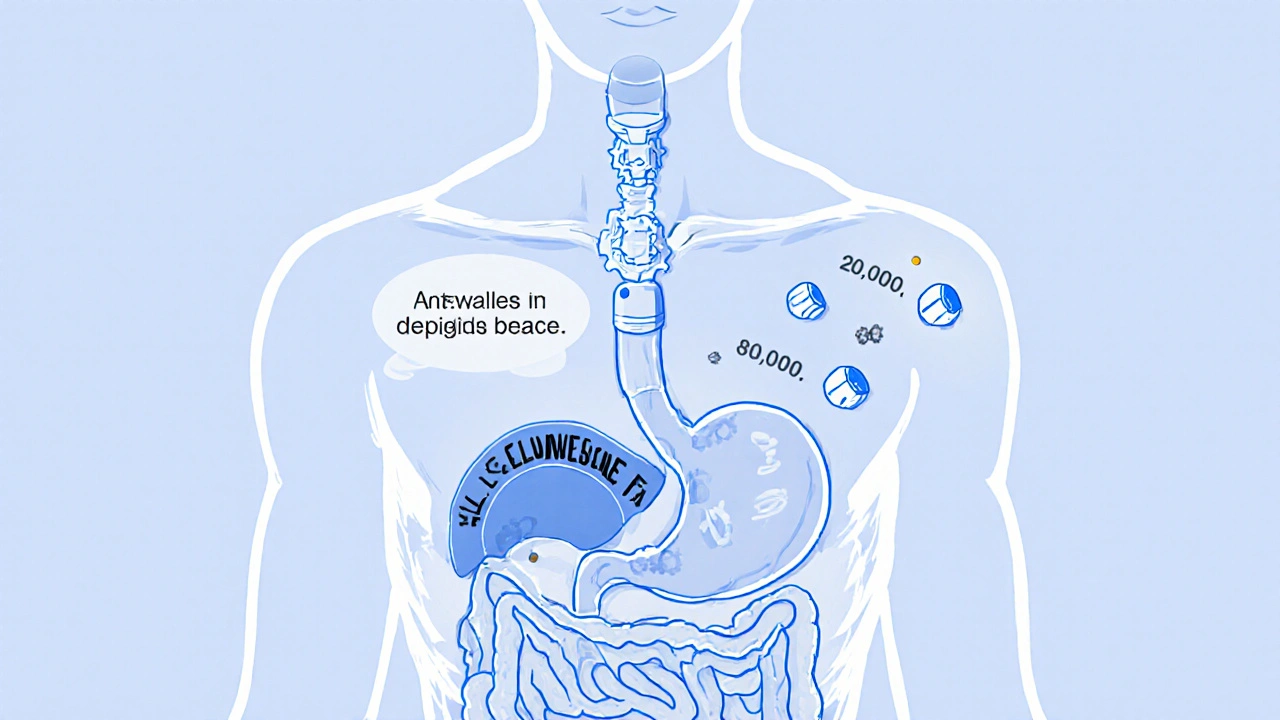
When Medications Fail: The Next Steps
Not everyone responds to pills and diet. When pain becomes unmanageable, it’s time to consider procedures. Endoscopic procedures like ERCP with stents can help if the pancreatic duct is blocked. About 60-70% get relief-but half of them are back in pain within a year. Celiac plexus blocks are another option. A needle injects alcohol or steroids near the nerves carrying pain signals from the pancreas. It doesn’t cure anything. But for some, it gives 6-9 months of near-complete relief. One patient in Melbourne said, “After two years of constant agony, the block gave me my life back.” Surgery is the last resort, but sometimes the best. The Frey procedure removes part of the pancreas and opens the duct. It gives 70-80% long-term pain relief. Total pancreatectomy with islet autotransplantation (TPIAT) removes the whole pancreas but saves insulin-producing cells. It’s 85-90% effective at stopping pain-but you’ll need insulin for life. These aren’t decisions made lightly. They’re made after months of failed meds, after losing jobs, after relationships fracture under the weight of pain. But for some, they’re the only path to a life that doesn’t revolve around a pill schedule.The Hidden Struggle: Mental Health and Access
No one talks about this enough. Chronic pancreatitis doesn’t just hurt your body. It eats your mind. Sixty-five percent of patients say their pain isn’t controlled by standard treatment. Forty-two percent say it’s constant and severe. Many feel dismissed by doctors who say, “It’s just pain.” But this isn’t psychosomatic. It’s real. And it’s relentless. Insurance battles over enzyme therapy are common. One patient spent 18 months fighting for coverage. Another had to choose between paying for enzymes or rent. The cost isn’t just money-it’s dignity. And the diagnostic delay? On average, people wait 2-3 years before getting a proper diagnosis. By then, the pancreas is already damaged. Early detection saves function. But most GPs don’t think of pancreatitis when someone says, “My stomach hurts after eating.” Specialized pancreas clinics-like those in major hospitals-offer multidisciplinary care: gastroenterologists, dietitians, pain specialists, counselors. But only 25% of community hospitals have these teams. Most patients are left to navigate this alone.
What’s Changing? What’s Next?
The field is slowly evolving. A new enzyme formulation called LipiGesic™, with pH-sensitive coating, is showing 20% better fat absorption in trials. That means fewer pills, better results. The NIH just launched a $15 million research initiative focused on non-opioid pain control. Trials are underway for drugs like cenobamate and dorsal root ganglion stimulation-nerve-targeting tech that’s already helping with chronic back pain. Genetic testing is also becoming part of care. Some people have mutations that make them more likely to develop severe pain. Knowing that early can change how aggressively you treat. The goal isn’t just to manage pain. It’s to stop it from becoming chronic in the first place. That means catching it early, quitting alcohol and smoking right away, and starting enzyme therapy before the pancreas gives up entirely. This isn’t a condition you conquer. It’s one you adapt to. With the right tools-medication, enzymes, nutrition, and support-you can still live. Not just survive. Live.Can chronic pancreatitis be cured?
No, chronic pancreatitis cannot be cured. The damage to the pancreas is permanent. But with proper treatment-pain management, enzyme therapy, nutrition, and lifestyle changes-most people can control symptoms and live full, active lives. Early intervention is key to slowing progression and preserving function.
Do I need to take enzymes with every meal, even snacks?
Yes. Take enzymes with every meal or snack that contains fat or protein-even a handful of nuts or a yogurt. Enzymes only work when they’re in the stomach at the same time as food. Taking them after eating means they won’t help. Always take them with the first bite.
Why am I still losing weight even though I take enzymes?
If you’re still losing weight, your enzyme dose may be too low, or you’re not taking them correctly. You might also have a vitamin deficiency or undiagnosed diabetes. Talk to your dietitian about adjusting your dose, checking your fat-soluble vitamin levels (A, D, E, K), and testing for type 3c diabetes. Weight loss isn’t normal-it’s a warning sign.
Is a low-fat diet always necessary for chronic pancreatitis?
Not always. While a low-fat diet (40-50g/day) helps many people reduce pain, some patients do better with moderate fat if they take enough enzymes. The key is matching your fat intake to your enzyme dose. Work with a dietitian to find your personal balance. MCT oils can also help because they don’t require enzymes to digest.
Can I drink alcohol occasionally if I have chronic pancreatitis?
No. Even small amounts of alcohol can trigger flare-ups and speed up pancreatic damage. Studies show that quitting alcohol cuts pain by 40-50% within six months. There is no safe level. Abstinence isn’t a recommendation-it’s non-negotiable for long-term health.
How do I know if my enzyme dose is right?
You’ll know if your symptoms improve: fewer greasy stools, less bloating, stable weight, less pain after meals. Your doctor may also check your fecal elastase-1 level or fat in your stool. If you’re still having symptoms, your dose may need to be increased-especially with high-fat meals. Don’t guess. Adjust under medical supervision.
Are there any new treatments on the horizon?
Yes. New enzyme formulations with better acid resistance are coming. Clinical trials are testing non-opioid nerve pain drugs and nerve stimulation devices like dorsal root ganglion stimulation. Genetic testing is also becoming more common to predict who will develop severe pain. The focus is shifting from managing symptoms to preventing chronic pain before it starts.
What should I do if my doctor doesn’t take my pain seriously?
Get a second opinion. Chronic pancreatitis pain is real and measurable. Look for a specialist in pancreatic diseases or a multidisciplinary pancreas clinic. Bring records of your symptoms, diet, medications, and pain diary. If your doctor dismisses you, you’re not being dramatic-you’re being ignored by someone who hasn’t seen enough cases. Don’t settle. Your quality of life depends on being heard.
Next Steps: What to Do Today
If you have chronic pancreatitis, start here:- Track your meals and pain for one week. Note what you ate, when you took enzymes, and your pain level.
- Ask your doctor for a blood test to check vitamins A, D, E, K, and fasting glucose.
- If you’re still drinking or smoking, make a plan to quit. Talk to your doctor about support programs.
- Request a referral to a dietitian who specializes in pancreatic disease.
- Ask if your enzyme dose is appropriate for your meals. Many people are underdosed.
- Look for a pain management specialist or pancreas clinic in your area. You don’t have to do this alone.

Asha Jijen
November 28, 2025 AT 06:11Alex Hess
November 29, 2025 AT 10:21Cecily Bogsprocket
November 29, 2025 AT 15:14Allison Turner
November 29, 2025 AT 19:23Iives Perl
November 30, 2025 AT 09:30Savakrit Singh
December 1, 2025 AT 11:32Jebari Lewis
December 1, 2025 AT 14:03Emma louise
December 2, 2025 AT 17:51Lauren Zableckis
December 3, 2025 AT 07:52Savakrit Singh
December 4, 2025 AT 23:35Cecily Bogsprocket
December 5, 2025 AT 22:39