
For years, people with chronic insomnia were told to just sleep hygiene-no caffeine after noon, keep the room cool, avoid screens before bed. Sounds simple, right? But if you’ve been lying awake for months, even years, you know that’s not enough. Sleep hygiene might help a little, but it won’t fix chronic insomnia. And that’s not your fault. It’s just not how the brain works when insomnia becomes deep-rooted.
What Chronic Insomnia Really Means
Chronic insomnia isn’t just having a bad night or two. It’s defined by the American Academy of Sleep Medicine as trouble falling asleep, staying asleep, or waking up feeling unrefreshed-happening at least three nights a week for three months or longer. This isn’t stress-related sleeplessness. It’s a persistent disruption in your body’s natural sleep rhythm, often locked in by habits, thoughts, and anxiety that have become automatic.
Think of it like a car stuck in mud. Pushing harder (lying in bed longer, trying harder to sleep) just makes it worse. You need the right tools to get out. That’s where CBT-I comes in.
Why Sleep Hygiene Isn’t Enough
Sleep hygiene is the set of habits that support good sleep: keeping your bedroom dark, quiet, and cool (around 65°F or 18.3°C), avoiding alcohol and caffeine late in the day, not eating heavy meals before bed. These things matter. But here’s the truth: studies show sleep hygiene alone helps less than 20% of people with chronic insomnia. The American Academy of Sleep Medicine gives it only moderate evidence-not strong.
Why? Because chronic insomnia isn’t just about your environment. It’s about your brain. Over time, your brain starts associating your bed with worry, frustration, and wakefulness. You lie there thinking, “I have to sleep. What if I don’t? I’ll be useless tomorrow.” That anxiety becomes part of the problem. No amount of blackout curtains will fix that.
Dr. Jack D. Edinger, one of the leading researchers in this field, says it plainly: “Sleep hygiene education alone is minimally effective for chronic insomnia and should not be offered as standalone treatment.” If you’ve been doing all the right things and still can’t sleep, you’re not failing. You just need a different approach.
What Is CBT-I-and Why It Works
Cognitive Behavioral Therapy for Insomnia, or CBT-I, is the only treatment recommended as first-line by the American College of Physicians, the American Academy of Sleep Medicine, and every major sleep organization worldwide. It’s not a pill. It’s a structured, evidence-based program that rewires how your brain thinks about sleep.
CBT-I typically runs for 6 to 8 weeks, with weekly sessions. But even short, two-session versions have shown real results. It doesn’t just help you fall asleep faster-it helps you stop fearing sleeplessness. And the effects last. Unlike sleeping pills, which wear off after a few weeks and can lead to dependence, CBT-I’s benefits stick around for years.
Here’s what the data says: 70 to 80% of people who complete CBT-I see clinically meaningful improvement. In one study, patients reduced their time to fall asleep by 18 minutes and cut nighttime wakefulness by 27 minutes. Compare that to sleeping pills, which only shaved off 12 and 16 minutes respectively-and only while you’re taking them.
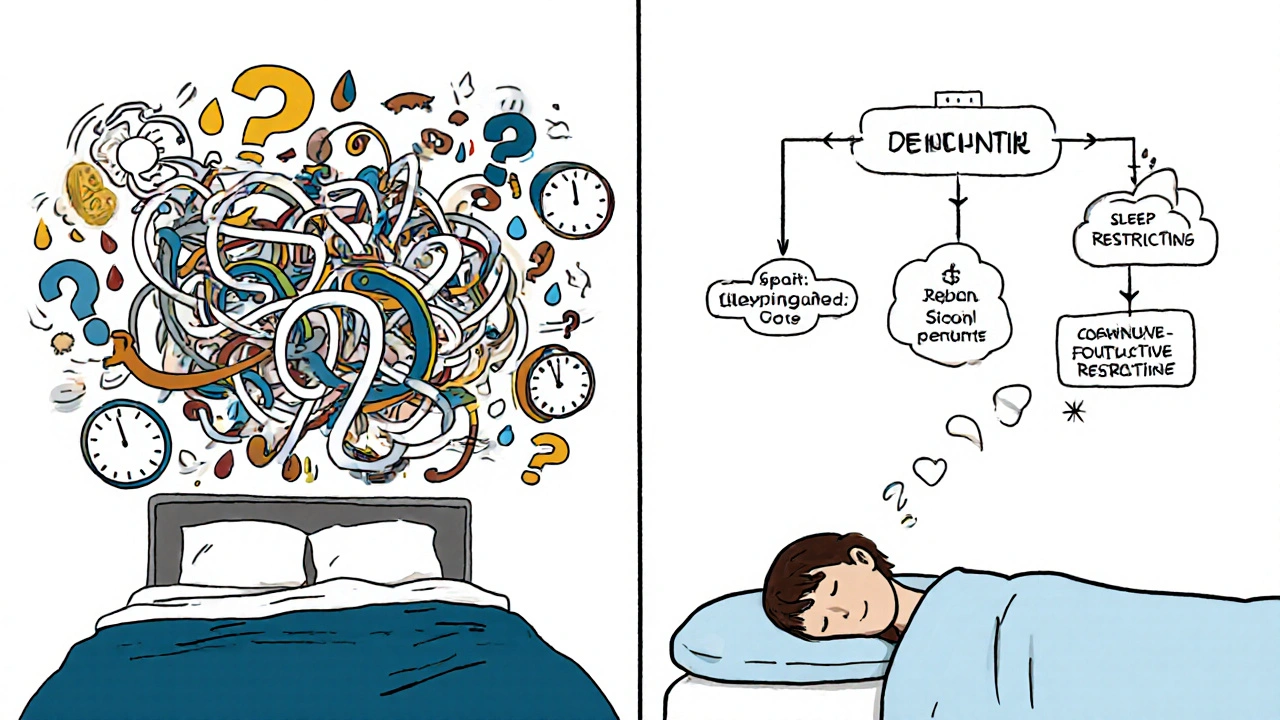
The Five Core Pieces of CBT-I
CBT-I isn’t one trick. It’s five tools working together.
- Stimulus Control: Your bed is only for sleep and sex. If you’re not asleep in 15-20 minutes, get up. Go to another room, sit quietly in dim light, and come back only when sleepy. This breaks the mental link between bed and frustration.
- Sleep Restriction: You’re probably spending too much time in bed. If you’re only sleeping 5 hours a night but lying in bed for 8, your brain doesn’t associate bed with deep sleep. CBT-I cuts your time in bed to match your actual sleep. It’s brutal at first-you’ll feel tired. But after a few weeks, your sleep efficiency shoots up. One Reddit user reported going from 68% sleep efficiency to 89% after 8 weeks.
- Cognitive Restructuring: This targets the thoughts that keep you awake: “I need 8 hours or I’ll collapse.” “If I don’t sleep tonight, my whole week is ruined.” These thoughts create anxiety, which keeps you awake. CBT-I helps you replace them with realistic, calming thoughts: “My body still recovers even if I sleep less tonight.” Studies show this reduces sleep anxiety in 65% of patients.
- Relaxation Training: Your body is stuck in high alert. Techniques like diaphragmatic breathing, progressive muscle relaxation, or mindfulness help lower your nervous system’s activity before bed.
- Sleep Hygiene: Yes, it’s still part of the package-but now it’s used as a supporting tool, not the main fix.
Real People, Real Results
Online communities like Reddit’s r/insomnia have over 15,000 members sharing their CBT-I journeys. Many say the first two weeks of sleep restriction were the hardest. One wrote: “I felt like a zombie. But after week three, I started sleeping. Not perfectly-but better than in years.” Another said: “I stopped checking the clock. That one change alone cut my anxiety in half.”
But it’s not all easy. A common complaint? Access. In the U.S., there are only about 0.5 CBT-I-trained therapists per 100,000 people. Insurance often covers only 3-4 sessions, even though 6-8 are recommended. Some people quit because they can’t find a provider, or their employer’s wellness program won’t pay for it.
That’s where digital CBT-I comes in. Apps like Sleepio and SHUTi have been tested in clinical trials and shown to work just as well as in-person therapy. One 2021 JAMA study found 50-60% of users achieved remission from insomnia after using these apps-compared to just 15-20% in control groups. The FDA has even cleared prescription digital therapeutics like Somryst, which showed 55.4% remission rates in trials.
What to Expect-And When
Don’t expect miracles in a week. CBT-I is a process. Most people notice small improvements around week 2-3. By week 6, many report falling asleep faster, waking up less, and feeling less anxious about sleep. Full benefits usually show up between 8 and 12 weeks.
Here’s what you’ll need to track:
- Bedtime and wake-up time (even on weekends)
- Time to fall asleep
- Number of awakenings
- How rested you feel
You can use a notebook, a simple app, or even your phone’s notes. This data helps you and your therapist adjust your plan. The Insomnia Severity Index (ISI) is the gold standard tool-scores above 15 mean moderate insomnia, above 22 mean severe. If you’re in that range, you need CBT-I, not just advice.
Why CBT-I Beats Pills-Every Time
Medications like zolpidem, eszopiclone, or suvorexant might help you sleep for a few nights. But after 4-6 weeks, their effect fades. Worse, you can become dependent. Withdrawal can make insomnia worse than before.
CBT-I doesn’t have side effects. No drowsiness. No memory issues. No risk of overdose. And the improvements last. A 2020 meta-analysis found CBT-I’s benefits remained strong even 12 months after treatment ended. Medication benefits? Gone the moment you stopped taking them.
Dr. Rachel Manber from Stanford puts it perfectly: “CBT-I changes the relationship with sleep, whereas medications merely mask the symptoms.”
Where to Start
If you’re ready to try CBT-I:
- Ask your doctor for a referral to a certified CBT-I therapist. Look for someone with training from the Society of Behavioral Sleep Medicine.
- If therapy isn’t accessible, try a digital program. Sleepio, SHUTi, and Somryst are all backed by research and available via app or web.
- Track your sleep for two weeks before starting. This gives you a baseline.
- Be patient. The first few weeks are the hardest. That’s normal.
- Don’t quit if you have a bad night. One rough night doesn’t undo progress.
And if you’re still relying on sleep meds? Talk to your doctor about tapering off while starting CBT-I. Many people successfully switch.
What’s Next for Insomnia Treatment
The future is bright. Wearables like Fitbit are now incorporating CBT-I principles into their sleep tracking. AI-driven apps are learning your patterns and personalizing therapy in real time. Pear Therapeutics’ reSET-S app, currently in Phase 3 trials, is showing 63% response rates. Experts predict CBT-I will become the standard for 90% of chronic insomnia cases within the next decade.
But right now, the most powerful tool you have is already here. You don’t need a miracle. You need a plan. And CBT-I is the only one proven to work long-term.
Can sleep hygiene cure chronic insomnia on its own?
No. While good sleep hygiene helps support healthy sleep, it’s not enough to fix chronic insomnia. Studies show it helps fewer than 20% of people with long-term sleep problems. The American Academy of Sleep Medicine and leading experts agree: sleep hygiene should be part of a broader plan, not the main treatment.
How long does CBT-I take to work?
Most people start seeing small improvements in 2-4 weeks. Significant changes-like falling asleep faster and waking up less-usually happen by week 6-8. Full benefits, including reduced anxiety about sleep and better daytime energy, typically show up after 8-12 weeks of consistent practice. The first two weeks of sleep restriction can feel tough, but that’s when the brain starts resetting.
Is CBT-I better than sleeping pills?
Yes, for chronic insomnia. Sleeping pills work for a few nights but lose effectiveness after 4-6 weeks and carry risks like dependence, memory issues, and rebound insomnia. CBT-I has no side effects, doesn’t cause dependence, and its benefits last for years after treatment ends. Clinical trials show CBT-I reduces sleep onset latency by 18 minutes and nighttime wakefulness by 27 minutes-better than any medication.
Can I do CBT-I on my own?
Yes, with the right tools. While working with a therapist is ideal, several digital programs-like Sleepio, SHUTi, and Somryst-are FDA-cleared and backed by clinical trials. These apps guide you through all the core components of CBT-I with daily exercises, sleep tracking, and personalized feedback. Many people see the same results as those who work with a therapist.
What if I can’t find a CBT-I therapist?
Therapist shortages are real-especially in rural areas. But digital CBT-I apps are widely available and often covered by insurance or employer wellness programs. Check with your health plan for approved apps. Some, like Somryst, require a prescription but are reimbursable. You can also ask your doctor for a referral to a telehealth provider who specializes in sleep.
Does CBT-I work for older adults?
Yes. Research shows CBT-I is just as effective for older adults as it is for younger people. In fact, it’s often preferred over medications because older adults are more sensitive to side effects like dizziness and confusion. Dr. Daniel Buysse’s studies show CBT-I produces large clinical improvements in seniors, with effect sizes of 1.0-1.3 on the Insomnia Severity Index-meaning real, noticeable changes in sleep and daily function.

jamie sigler
December 1, 2025 AT 10:15I’ve been doing all the sleep hygiene stuff for years. Dark room, no screens, cool temp, herbal tea at 7 PM like a good little sleep zombie. Still wide awake at 2 AM thinking about how I’m going to fail at life tomorrow. Guess I’m just broken.
Why does it feel like my brain’s holding a grudge against sleep?
Bernie Terrien
December 1, 2025 AT 20:45Sleep hygiene is the placebo of the sleep world. A Band-Aid on a severed artery. CBT-I? That’s the tourniquet. The scalpel. The goddamn miracle.
They hand you a pamphlet on ‘good habits’ while your nervous system’s screaming in the dark. Pathetic.
Subhash Singh
December 2, 2025 AT 08:16It is indeed a matter of considerable scientific interest that sleep hygiene, while beneficial in promoting optimal sleep conditions, fails to address the neurocognitive perpetuation of chronic insomnia. The cognitive-behavioral model, grounded in empirical evidence, offers a mechanistic intervention that targets maladaptive thought patterns and conditioned arousal. I commend the thoroughness of the presented framework.
However, one must inquire: to what extent does socioeconomic accessibility to digital CBT-I platforms mitigate or exacerbate health disparities in non-Western populations?
Geoff Heredia
December 3, 2025 AT 09:51They don’t want you to sleep. That’s why they sell you pillows and melatonin. CBT-I? It’s a front. The real solution is shutting off the 5G towers that sync your brainwaves to the government’s sleep suppression network. I’ve been using aluminum foil hats and grounding mats since 2019. My sleep efficiency went from 41% to 87% after I stopped letting my toaster near my bed.
They’re coming for your REM cycles next. Watch the clock. They’re watching too.
Andrew Keh
December 5, 2025 AT 04:59I appreciate this breakdown. I tried sleep hygiene for months and felt worse because I was so focused on ‘doing it right.’ CBT-I made me stop trying so hard. The idea of getting out of bed if I wasn’t sleepy felt impossible at first-but now it’s the only thing that works.
It’s not magic. It’s just smarter than fighting your own brain.
Peter Lubem Ause
December 6, 2025 AT 13:30Let me tell you something-this isn’t just about sleep. This is about reclaiming your life. You’ve been lied to. Told to just ‘relax’ like sleep is a switch you can flip. But your brain? It’s been trained to panic in the dark. CBT-I doesn’t just fix sleep-it rewires your relationship with rest. I was a mess for seven years. Woke up every day like I’d been dragged through a gravel pit. Then I did sleep restriction. Week one? I cried every night. Week three? I slept six hours straight. Not perfect. Not magical. But real. And now I don’t fear the night anymore. You can do this. One step. One night. One breath at a time.
And yes, you’re not broken. You’re just stuck. And stuck things can be unstuck.
linda wood
December 6, 2025 AT 18:31So let me get this straight… you’re telling me the entire sleep industry made millions selling me $80 pillows and lavender sprays while the real fix was a 6-week mental reboot that costs $0 if I use an app?
And I’m supposed to feel bad for not knowing this because I was too busy being told to ‘drink chamomile and count sheep’?
Wow. I feel so seen. And also, slightly scammed.
LINDA PUSPITASARI
December 8, 2025 AT 07:06OMG YES I DID CBT-I AND IT CHANGED MY LIFE 🙌 I used Sleepio and I was skeptical but like… week 2 I actually fell asleep without checking the clock once 😭 I used to think if I didn’t sleep 8 hours I’d die. Now I’m like ‘meh, 5 is fine, my body’s chill’
Also the sleep restriction part felt like torture but it’s like your brain needed a reboot 🤯 I’m not saying it’s easy but it’s worth it. You got this 💪
PS: if you’re scared of apps, try the free version first. No pressure. Just breathe. You’re not alone.
gerardo beaudoin
December 8, 2025 AT 07:21I tried CBT-I through my employer’s wellness program. Took me three months to finish because I kept skipping sessions. But I stuck with it. The part that clicked for me? Getting up when I couldn’t sleep. I used to lie there for hours thinking, ‘I have to sleep.’ Turns out, the more I told myself that, the more awake I got.
Now I read in another room. No phone. Just a dim lamp. And I don’t feel guilty about it. Weirdly, I sleep better now.
Thanks for writing this. It’s nice to know I’m not the only one who thought I was failing.
Joy Aniekwe
December 9, 2025 AT 23:35So you’re telling me the reason I’ve been awake since 2018 isn’t because I’m ‘too stressed’ or ‘have bad habits’… but because my brain learned to hate my bed?
And the solution is… not to fight it?
Wow. That’s actually kind of poetic.
Also, I’m still not sleeping. But at least now I’m not blaming myself. Progress, I guess.