Most people don’t think about their bones until they break. But osteoporosis doesn’t come with warning signs. It’s silent. By the time a hip or spine fracture happens, the damage is already done. That’s why DEXA scan results matter - they can catch bone loss before it leads to a life-altering injury.
What Is a DEXA Scan and Why Does It Matter?
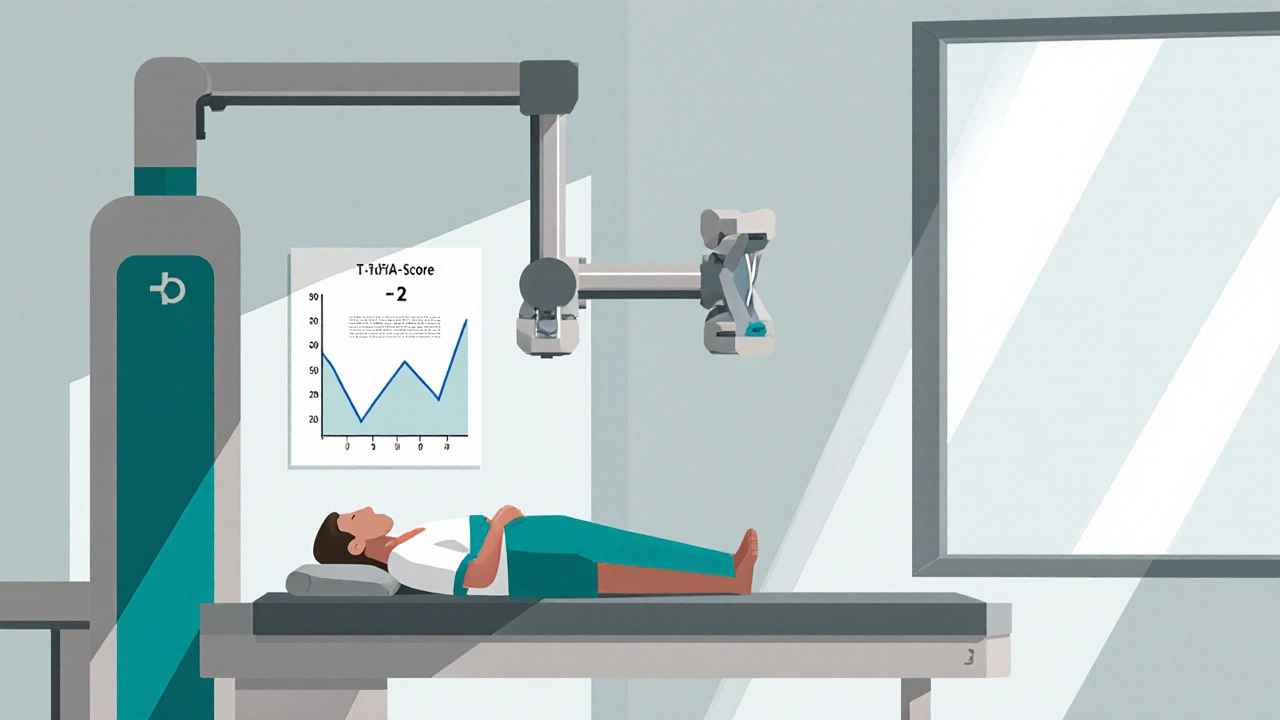
A DEXA scan - short for dual-energy X-ray absorptiometry - is the most accurate, widely used test to measure bone mineral density. It’s not a regular X-ray. It uses two very low-dose X-ray beams to calculate how much mineral is packed into your bones, especially in the spine and hip. The radiation you get from one scan is less than what you’d naturally absorb from the sun in two days. You lie still on a table for about 10 minutes. No needles. No fasting. No pain.
It’s not just a convenience. DEXA is the only bone density test recommended by the U.S. Preventive Services Task Force for routine screening. Over 15 million scans are done in the U.S. every year. And for good reason: it’s been proven over decades to predict who’s at risk for fractures better than any other tool.
Reading Your DEXA Results: T-Score Explained
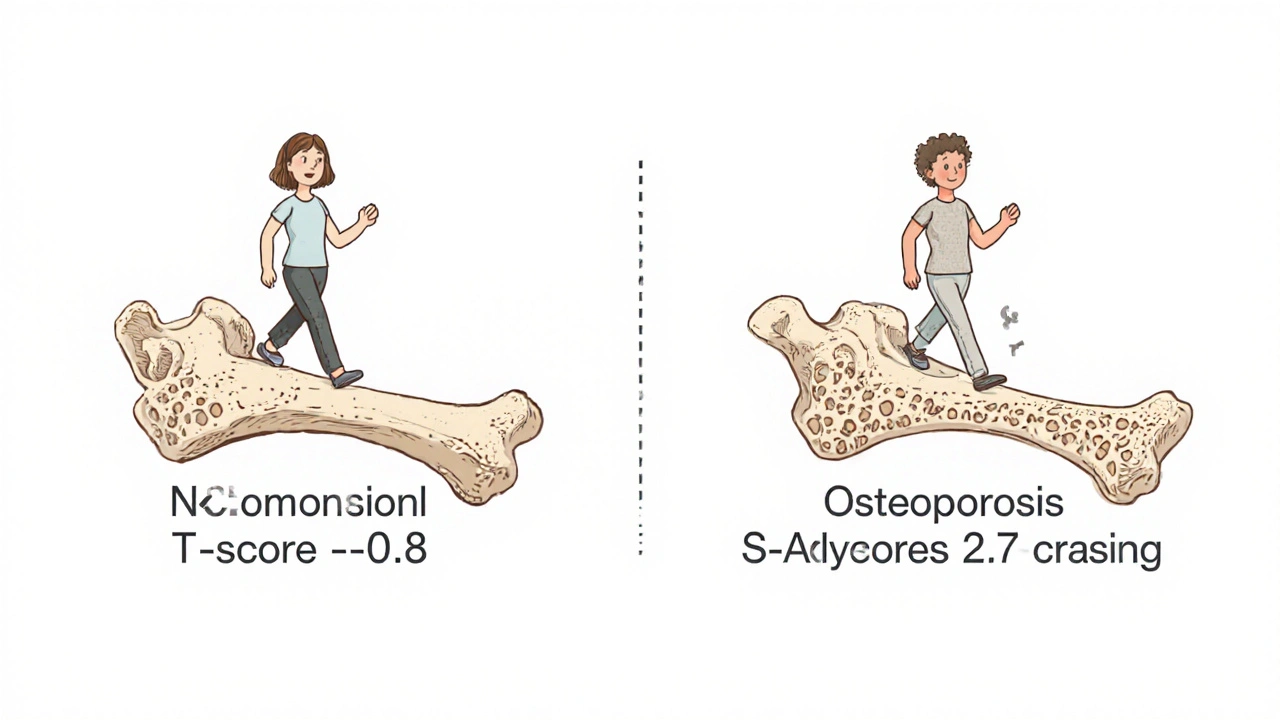
Your DEXA report gives you a number called a T-score. This tells you how your bone density compares to that of a healthy 30-year-old adult of the same sex and race. It’s measured in standard deviations.
- T-score of -1.0 or higher: Normal bone density. Your bones are strong.
- T-score between -1.0 and -2.5: Osteopenia. This means your bones are thinner than normal but not yet osteoporotic. It’s a red flag - not a diagnosis, but a call to act.
- T-score of -2.5 or lower: Osteoporosis. Your bones are significantly weakened, and your risk of breaking a bone rises sharply.
For example, a T-score of -2.7 means your bone density is 2.7 standard deviations below the peak level of a young adult. That’s not just low - it’s in the danger zone. A woman in her late 60s with this score has a 20% or higher chance of breaking a bone within 10 years - even if she’s never had a fall.
Don’t confuse T-score with Z-score. The Z-score compares your bone density to others your own age. It’s useful for younger people or those with unusual medical conditions, but for most adults over 50, the T-score is what guides treatment.
Fracture Risk Isn’t Just About Bone Density
Here’s the catch: a low T-score doesn’t always mean you’ll break a bone. And some people with normal bone density still fracture. Why? Because bone strength isn’t just about how dense it is - it’s about how it’s structured.
That’s why doctors use FRAX, a free online tool developed by the World Health Organization. FRAX doesn’t just look at your T-score. It adds in your age, sex, weight, history of fractures, smoking, steroid use, and whether you have rheumatoid arthritis or a parent who broke a hip. Together, these factors give a more complete picture of your 10-year fracture risk.
Studies show that when FRAX includes your DEXA result, it predicts fractures 15-22% better than using bone density alone. For someone with a T-score of -2.0 and a history of falls, FRAX might show a 25% risk of major fracture - enough to justify medication. For someone with the same T-score but no other risk factors, lifestyle changes might be enough.
What DEXA Can’t Tell You
DEXA is excellent, but it’s not perfect. It gives you a 2D picture of 3D bone. It can’t tell the difference between thick cortical bone (the hard outer shell) and spongy trabecular bone (the inner network that’s more vulnerable to loss). It also can’t detect microcracks or poor bone quality - only how much mineral is there.
It also struggles in people with severe arthritis, spinal fusion, or metal implants. If you’ve had a hip replacement or a lot of spinal degeneration, the scan might give a falsely high reading. That’s why your doctor needs to know your full medical history - including past surgeries or injuries.
Some newer tools are starting to fill these gaps. Trabecular Bone Score (TBS) is now being added to many DEXA reports. TBS looks at the texture of the bone on the scan image - a rougher texture means weaker structure. Studies show TBS improves fracture prediction by 12-18% beyond T-score alone. AI-powered software is also being used to automatically spot tiny spine fractures that even radiologists might miss.
Who Should Get a DEXA Scan?
Medicare and most insurers cover a DEXA scan every two years for:
- Women 65 and older
- Men 70 and older
- Anyone who’s broken a bone after age 50
- Postmenopausal women under 65 with risk factors (low body weight, smoking, steroid use, family history)
- Men 50-69 with risk factors
- People on long-term steroid therapy (like prednisone for more than 3 months)
But coverage isn’t universal. Many people under 65 with early menopause, celiac disease, or hyperthyroidism are at risk but don’t get screened because their doctors don’t think to order it. If you have any of these conditions, ask. Don’t wait for symptoms.
What Happens After Your Scan?
If your T-score is normal? Keep doing what you’re doing: get enough calcium and vitamin D, do weight-bearing exercise, avoid smoking, and limit alcohol.
If you have osteopenia? You’re not doomed. Many people reverse bone loss with lifestyle changes alone. Resistance training - even lifting light weights twice a week - can increase bone density by 1-3% per year. Vitamin D levels below 30 ng/mL are linked to faster bone loss. Getting your blood tested and supplementing if needed can make a big difference.
If you have osteoporosis? Medication is often recommended. Bisphosphonates like alendronate (Fosamax) or denosumab (Prolia) can reduce fracture risk by up to 70% over three years. But they’re not for everyone. Your doctor will weigh your risk of side effects - like rare jaw bone issues or atypical femur fractures - against your fracture risk.
Some patients worry about radiation. One DEXA scan is about 0.001 to 0.03 mSv. A chest X-ray is 0.1 mSv. A cross-country flight is 0.03 mSv. The risk from the scan is negligible compared to the risk of a broken hip.

Real-World Impact: A Case That Changed Everything
A 68-year-old woman came in for a routine checkup. She had no pain. No history of fractures. Her doctor ordered a DEXA scan anyway because she was postmenopausal and underweight. Her T-score was -2.7 - osteoporosis. She started treatment with a weekly pill and a daily walking routine. Six months later, she broke her wrist while gardening. No one was surprised - she’d been warned. But the next year, she had another scan. Her T-score had improved to -2.1. She didn’t just stop bone loss - she started rebuilding. She’s now 72 and still hiking.
This isn’t rare. It’s the norm for people who act early. Osteoporosis isn’t a death sentence. It’s a manageable condition - if you catch it in time.
Barriers to Screening - And How to Overcome Them
Despite how effective DEXA is, screening rates are still too low. In 2022, only 38% of eligible White women got screened. For Black women, it was 23%. For Hispanic women, just 18%. Why? Access, awareness, and bias. Many clinics don’t offer it. Some doctors assume older patients won’t benefit. Others don’t know how to interpret the results.
If you’re concerned, don’t wait for your doctor to bring it up. Print out the USPSTF guidelines. Ask for a referral. If insurance denies it, ask for a letter of medical necessity - especially if you have risk factors.
And if you get your results and don’t understand them? Ask for a copy. Ask for an explanation. Don’t let a confusing T-score be the reason you don’t take action.
What’s Next for Bone Health Screening?
The future of bone screening is smarter, not just faster. AI tools are now being trained to detect spine fractures on DEXA scans without extra imaging. Trabecular Bone Score is becoming standard in many centers. Newer machines can measure bone strength in the forearm - useful for people who can’t lie flat.
But the biggest breakthrough won’t be a new machine. It’ll be better use of existing tools. Combining DEXA with FRAX, lifestyle coaching, and patient education is what reduces fractures - not just the scan itself.
There’s no magic pill for strong bones. But there is a simple, safe, and proven way to find out if yours are at risk - and then do something about it.
How often should I get a DEXA scan?
If your first scan is normal, most people get another one every 2 years. If you have osteopenia or are on treatment, your doctor might repeat it every 1-2 years to track progress. If you’re over 70 with stable bone density and no new risk factors, you may not need another scan at all. Always follow your doctor’s advice based on your personal risk.
Can I get a DEXA scan without a doctor’s referral?
In most cases, no. Insurance requires a referral from a licensed provider. Some wellness centers offer direct-to-consumer scans, but these are often not covered and may not follow clinical standards. Always get your scan through a certified facility that follows ISCD guidelines.
Is a DEXA scan the same as a bone scan?
No. A bone scan uses radioactive tracer to detect areas of abnormal bone activity - like infection, cancer, or healing fractures. A DEXA scan measures bone density. They serve completely different purposes. One finds problems; the other prevents them.
What if my T-score is low but I’ve never broken a bone?
That’s exactly why DEXA is important. Osteoporosis is called a silent disease because you can have it for years without symptoms. A low T-score means your bones are weaker than they should be - even if you haven’t fallen yet. Starting prevention early - with exercise, nutrition, or medication - can stop fractures before they happen.
Can men get osteoporosis?
Yes. One in four men over 50 will break a bone due to osteoporosis. Men are less likely to get screened, but they’re just as vulnerable - especially if they’re on steroids, have low testosterone, smoke, or drink heavily. DEXA scans are just as important for men as they are for women.
Do I need to stop taking calcium or vitamins before the scan?
No. But if you take calcium supplements, don’t take them within 24 hours of the scan. Large amounts of calcium in your system right before the scan can interfere with accuracy. Otherwise, keep taking your vitamins as usual - your doctor needs to see your real-world bone health.

Shyamal Spadoni
November 15, 2025 AT 06:12so i read this whole thing and like... are we sure the machine isn't just measuring how much calcium you ate yesterday? like i got my scan done after a big dairy binge and my t-score went up 0.5 points. coincidence? i think not. the pharmaceutical companies own the dexas, the radiologists, and probably your toaster too. they want you scared so you keep buying pills that make your jaw fall off. also, why is everyone so obsessed with 30-year-olds? my bones arent supposed to be like a teenager's, bro. i'm 67, not a gym bro. #conspiracy #dexamindgames
Ogonna Igbo
November 17, 2025 AT 05:29in nigeria we dont have dexas everywhere but we know bone break easy when you old. we dont need fancy numbers to know if you weak. if you fall and hip break? you dead. no insurance, no pill, no scan. we just pray. this post sound like rich man talk. what about people who eat one meal a day and walk 10km to market? your bone density dont matter if you dont have food. the real problem is poverty not t-score. stop making us feel guilty for not having scan. we survive different.
BABA SABKA
November 18, 2025 AT 17:50let me cut through the medical jargon here - dexas are a proxy metric, not a diagnostic gold standard. the trabecular bone score is the real frontier, but it’s still algorithmically inferred from noise in the x-ray attenuation patterns. we’re quantifying mineralization density, not structural integrity, not microarchitectural resilience, not collagen cross-linking efficiency. the frax model is statistically robust but culturally biased - it’s calibrated on caucasian cohorts, yet applied globally. this is precision medicine with colonial DNA. if you’re black, hispanic, or asian, your risk profile is being interpolated from data that doesn’t reflect your biology. and don’t get me started on how bisphosphonates suppress remodeling and create brittle bones over time. we’re treating a symptom with a sledgehammer while ignoring the systemic inflammation, vitamin k2 deficiency, and gut dysbiosis driving bone loss. this isn’t healthcare. it’s pharmacological theater.
Chris Bryan
November 18, 2025 AT 22:49they’re lying to you. the whole bone density industry is a scam run by big pharma and the radiology cartel. dexas? they’re calibrated to make you look worse so you’ll take drugs. the real cause of osteoporosis? 5g radiation from cell towers. it disrupts calcium ion channels. the government knows. the FDA knows. they don’t tell you because pills make more money than warning people to unplug their wifi at night. also, why are women targeted more? because they’re easier to scare. men get prostate cancer, women get osteoporosis - both manufactured crises. i’ve never had a scan. i eat bone broth, lift heavy, and sleep on the floor. my bones are stronger than yours. #truth #dexamindgames
Jonathan Dobey
November 19, 2025 AT 10:34ah yes, the modern priesthood of bone mineral density - priests of the dual-energy x-ray altar, murmuring incantations of t-scores and z-scores like sacred mantras. we’ve reduced the sublime architecture of the human skeleton - a living, breathing, dynamically remodeled lattice forged by gravity, blood, and time - to a single, cold, decimal number. and we call this science? it’s numerology dressed in white coats. the body isn’t a spreadsheet. it’s a symphony of collagen, osteoblasts, and the quiet wisdom of centuries of human movement. we’ve forgotten that bones aren’t just calcium bricks - they’re the silent poets of our posture, our leaps, our falls, our survival. and now we outsource our vitality to algorithms trained on white 30-year-olds who’ve never carried a sack of grain or climbed a mountain. the real fracture? our surrender to quantification. the real osteoporosis? the loss of wonder.
ASHISH TURAN
November 19, 2025 AT 21:17good breakdown. i’m 58 and got my first dexam after my dad broke his hip. t-score was -2.3. started walking daily, took vitamin d3+k2, and did resistance bands twice a week. 18 months later, back to -1.9. no meds. just consistency. also, if you’re under 65 and have celiac or thyroid issues - get tested. doctors forget. i had to ask twice. no shame in asking. your bones don’t care how loud you are.
Ryan Airey
November 21, 2025 AT 17:19stop with the feel-good nonsense. osteopenia isn’t a ‘red flag’ - it’s a clinical diagnosis of bone fragility. if your t-score is below -1.0, you’re already at elevated fracture risk. no amount of yoga or bone broth changes that. the data is clear: pharmacological intervention reduces hip fractures by 50% in high-risk patients. if you’re avoiding meds because you ‘trust your body,’ you’re gambling with your independence. and yes, the radiation is negligible. if you’re scared of 0.01 mSv, you’re scared of sunlight. get the scan. take the pill. live longer. this isn’t philosophy - it’s epidemiology.
Hollis Hollywood
November 21, 2025 AT 19:50i just want to say thank you for writing this. my mom had a dexam last year - t-score -2.8 - and she was so scared she stopped leaving the house. i showed her the part about how 20% fracture risk isn’t a death sentence, and how people rebuild bone. she started walking with me every morning. now she’s gardening again. she even got a puppy. it’s not just about the numbers. it’s about giving people hope, not fear. the fact that you included the case study with the 68-year-old woman? that’s the kind of thing that changes lives. i wish more doctors wrote like this. you didn’t just explain the scan - you explained the person behind it.
Aidan McCord-Amasis
November 23, 2025 AT 18:29scan = good. meds = maybe. walking = always. 🚶♂️💪