When you're nursing, every pill you take feels like a gamble. You want relief from allergies or a headache, but you’re terrified of harming your baby. The good news? Most common antihistamines and pain relievers are safe - if you know which ones to pick. The bad news? Many over-the-counter products hide dangerous ingredients in plain sight. This isn’t about avoiding meds entirely. It’s about choosing wisely.
Not All Antihistamines Are Created Equal
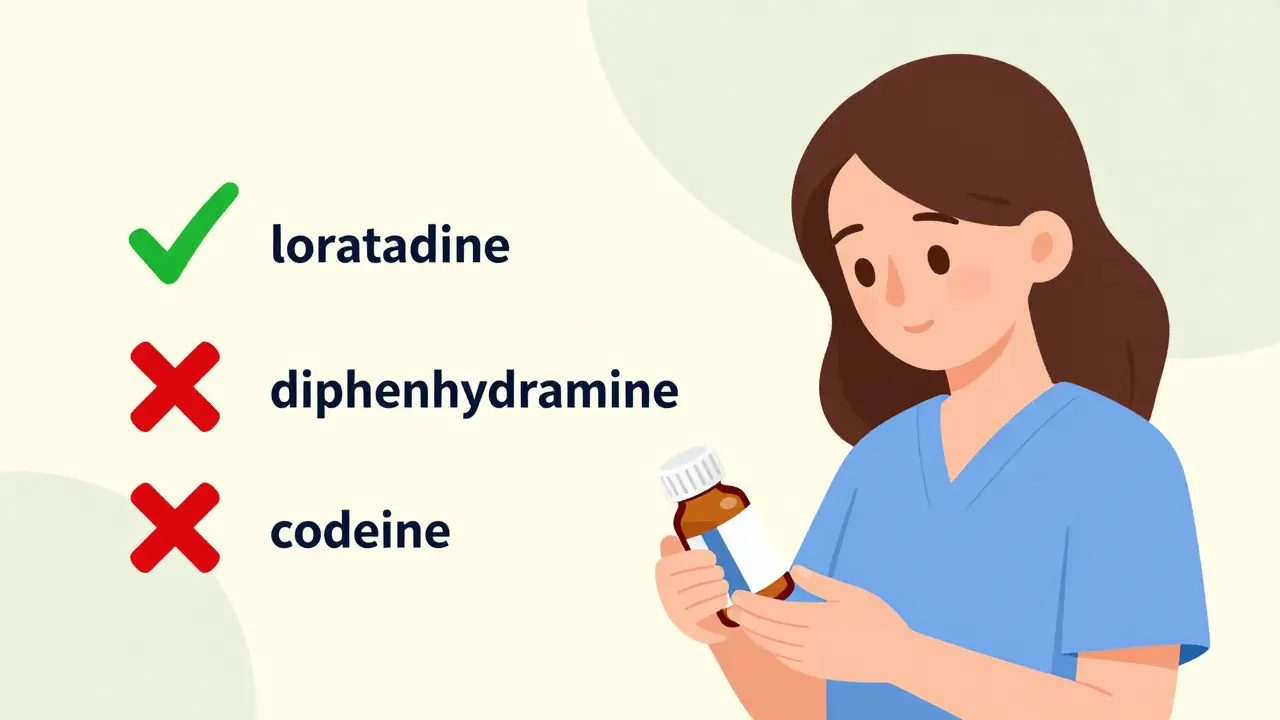
First-generation antihistamines like diphenhydramine (Benadryl), chlorpheniramine, and promethazine used to be the go-to for allergies. But they’re a bad fit for nursing moms. These drugs cross into breast milk easily and can make your baby drowsy, sluggish, or even refuse to feed. In rare cases, long-term use has been linked to poor weight gain and feeding problems. One mother in Sydney reported her 3-month-old became unusually sleepy after she took Benadryl for hay fever - she didn’t realize it was the medication until she stopped it and the baby bounced back within 24 hours. Second-generation antihistamines are the clear winners. Loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) barely make it into breast milk. Studies show less than 0.05% of the mother’s dose reaches the baby. That’s like sipping a teaspoon of water from a swimming pool. The American Academy of Family Physicians and Mayo Clinic both list these as preferred options. They don’t cause drowsiness in moms or babies, and there’s no evidence of side effects in infants, even with daily use.Pain Relievers: The Safe Trio
For pain or fever, acetaminophen (Tylenol) and ibuprofen (Advil, Motrin) are your safest bets. Acetaminophen transfers into milk at just 1-2% of the maternal dose. Ibuprofen is even lower - around 0.6-0.8%. Both are cleared from your system quickly, so there’s almost nothing left by the time your baby feeds again. Ibuprofen has an extra advantage: it’s been studied in thousands of nursing mothers. No link to reduced milk supply. No reports of infant bleeding, diarrhea, or fussiness. In fact, the World Health Organization includes ibuprofen in its list of essential medicines for breastfeeding women. Avoid naproxen (Aleve). It sticks around in your body for 12-17 hours. That means more of it ends up in your milk. There are documented cases of infants developing anemia, vomiting, or bleeding issues after prolonged exposure. The AAFP specifically warns against long-term use. If you need something for chronic pain, stick with ibuprofen or acetaminophen and talk to your doctor before switching.What About Codeine, Oxycodone, or Tramadol?
These are prescription painkillers - and they’re risky. Codeine is metabolized into morphine in your body. Some women metabolize it faster than others, leading to dangerously high levels in breast milk. There have been infant deaths linked to codeine use while nursing. The FDA and WHO both advise against it. Oxycodone and tramadol carry similar warnings. Even morphine, while sometimes used in hospitals after delivery, should only be given in low doses and for short periods. If you’re in severe pain after birth and your doctor suggests one of these, ask for alternatives. Most of the time, you don’t need them. Acetaminophen and ibuprofen work just fine for most postpartum pain.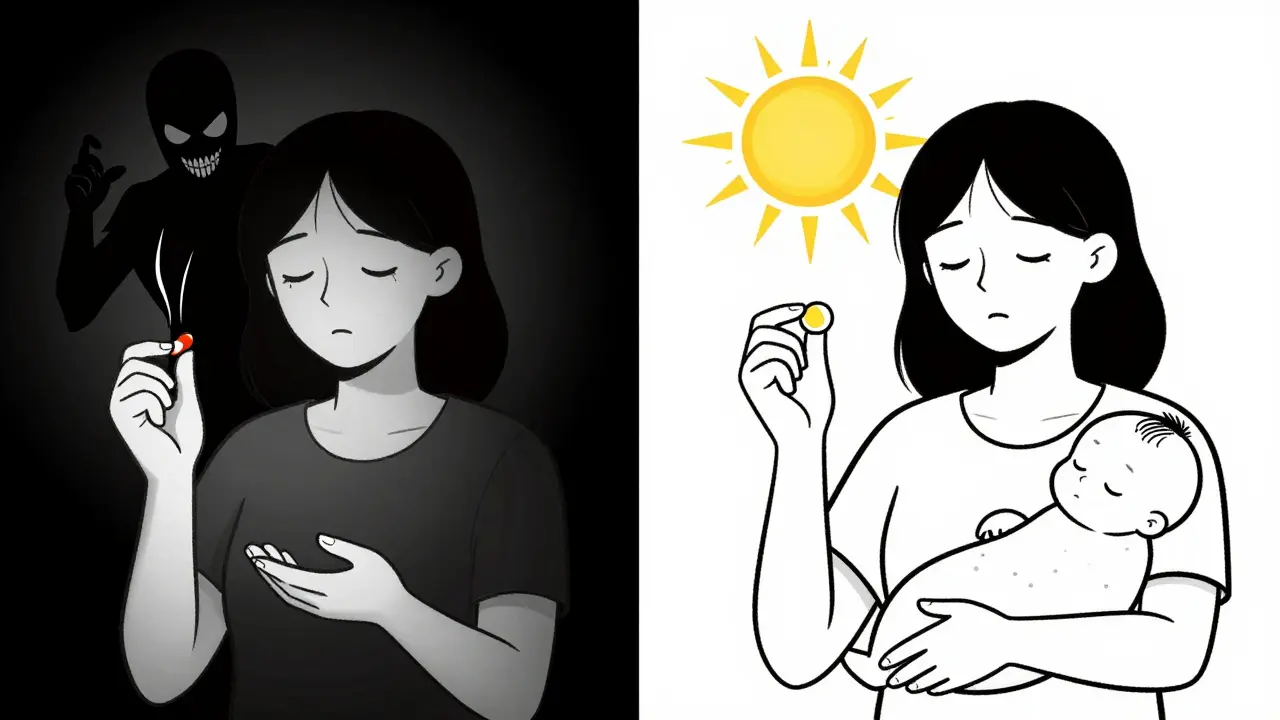
Hidden Antihistamines in Cold and Flu Meds
This is where most moms get tripped up. You grab a cold tablet because you’ve got a runny nose and a sore throat. But that “one-a-day” pill? It might contain diphenhydramine or chlorpheniramine. Same with nighttime allergy pills, sleep aids, and even some cough syrups. Check the label. Look for these ingredients:- Diphenhydramine
- Chlorpheniramine
- Promethazine
- Doxylamine
- Hydroxyzine
How to Use These Meds Safely
Even safe meds need smart use. Here’s how to minimize any risk:- Take the lowest effective dose. You don’t need 800 mg of ibuprofen for a mild headache.
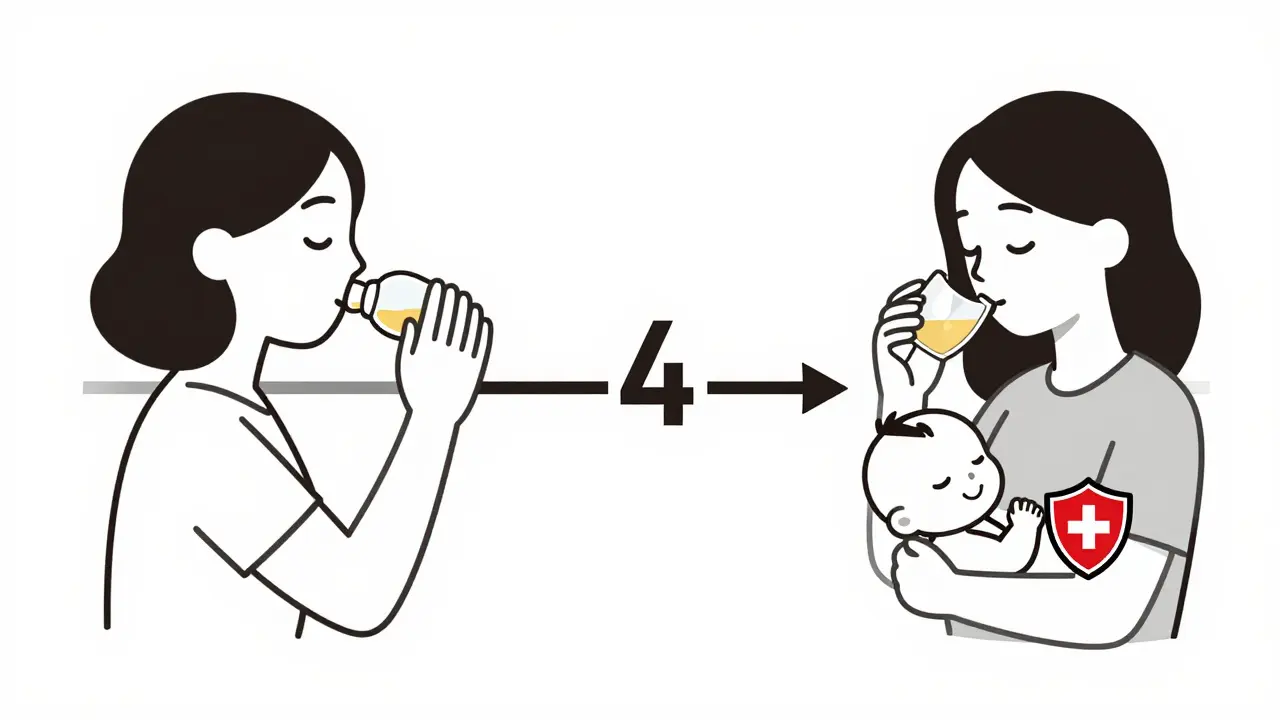
- Time your doses. Take your medication right after a feeding, so levels are lowest when your baby nurses again.
- Watch your baby. Look for changes in feeding, sleepiness, irritability, or rash. If something seems off, stop the med and call your doctor.
- Don’t mix with alcohol or sedatives. Even if the med is safe, combining it with other depressants can amplify effects.
- Use a pill organizer. It helps you avoid double-dosing, especially if you’re using multiple OTC products.
When to Call Your Doctor
You don’t need to panic over every little change. But call your pediatrician or lactation consultant if:- Your baby becomes unusually sleepy or hard to wake for feeds
- Your baby refuses to eat for more than one or two feeds
- You notice unusual bruising, bleeding, or yellowing of the skin
- Your milk supply drops suddenly
- You’re taking more than one medication at a time
What About Natural Alternatives?
Some moms turn to herbal teas, steam inhalation, or honey for allergies or pain. Honey is safe for you - but never give it to babies under 12 months. Herbal remedies like chamomile or peppermint tea are generally low-risk in small amounts, but they’re not regulated. There’s no proof they work better than proven meds, and some herbs can reduce milk supply. Stick to what’s been tested. If you’re curious about an herb, ask your pharmacist. They know what’s safe and what’s just folklore.The Bottom Line
You can take antihistamines and pain relievers while nursing - safely. Just choose the right ones. Loratadine, cetirizine, and fexofenadine for allergies. Acetaminophen and ibuprofen for pain. Avoid anything with diphenhydramine, naproxen, or codeine. Read labels like your baby’s life depends on it - because it does. Most OTC products are fine, but the ones that aren’t? They’re hiding in plain sight.There’s no need to suffer through allergies or headaches. With the right info, you can take care of yourself without putting your baby at risk. The science is clear. The guidelines are consistent. You’ve got this.
Can I take Zyrtec while breastfeeding?
Yes, cetirizine (Zyrtec) is considered safe for breastfeeding mothers. Studies show less than 0.1% of the maternal dose transfers into breast milk, and no adverse effects have been reported in nursing infants. It’s one of the top-recommended second-generation antihistamines for use while nursing.
Is Benadryl safe for nursing moms?
Diphenhydramine (Benadryl) is not recommended for regular use while breastfeeding. It can cause drowsiness in both mother and baby, and may lead to poor feeding or reduced milk supply. If you need a quick fix for a severe allergic reaction, a single dose may be okay - but avoid daily use and always monitor your baby for signs of sleepiness or fussiness.
Can I take ibuprofen while breastfeeding?
Yes, ibuprofen is one of the safest pain relievers for nursing mothers. It transfers into breast milk in very small amounts (less than 1% of the maternal dose) and is cleared quickly from your system. There’s no evidence it affects milk supply or harms the baby when used at standard doses.
Is Tylenol safe for breastfeeding?
Yes, acetaminophen (Tylenol) is safe for breastfeeding. Only 1-2% of the dose enters breast milk, and no negative effects on infants have been documented. It’s often the first choice for pain or fever in nursing mothers because of its long safety record.
What cold medicines are safe while breastfeeding?
Avoid combination cold medicines. Instead, use single-ingredient products: acetaminophen for pain/fever, loratadine or cetirizine for runny nose, and saline nasal spray for congestion. Check labels for hidden antihistamines like diphenhydramine or chlorpheniramine - they’re common in nighttime formulas and can make your baby sleepy.
Can antihistamines reduce my milk supply?
First-generation antihistamines like diphenhydramine may reduce milk supply in some women, especially with frequent use. Second-generation antihistamines like loratadine and cetirizine do not affect milk production. If you notice your supply dropping after starting a new medication, switch to a safer option and monitor for improvement.
How long should I wait after taking medicine before breastfeeding?
For most safe medications like ibuprofen or loratadine, you don’t need to wait. But if you’re taking something with a longer half-life or are unsure, take it right after a feeding. This gives your body time to clear the drug before the next feed. For example, take your dose after the nighttime feed so levels are lowest during morning feeds.
Are there any antihistamines I should avoid completely while breastfeeding?
Yes. Avoid first-generation antihistamines like diphenhydramine, chlorpheniramine, promethazine, and doxylamine for regular use. These can cause drowsiness, feeding problems, and even failure to thrive in infants. Prescription antihistamines like hydroxyzine should also be avoided unless specifically approved by your doctor.

Manish Kumar
January 8, 2026 AT 09:23Look, I get it-we’re all just trying to survive parenthood while pretending we’re not one coffee away from a nervous breakdown. But here’s the thing: medicine isn’t magic. It’s chemistry. And your baby’s liver? It’s still learning how to do its job. So yeah, Zyrtec’s fine. Tylenol’s fine. But if you’re popping Benadryl like it’s candy because you ‘can’t sleep,’ you’re not being brave-you’re being careless. We’ve got data. We’ve got guidelines. Stop guessing. Start reading labels like your kid’s life depends on it-because it does.
And don’t even get me started on those ‘natural remedies.’ Chamomile tea won’t cure your allergies, and honey won’t stop your sinuses from exploding. It’s not 1820 anymore. We have science. Use it.
Also, if you’re taking something with ‘PM’ in the name? Put it down. That’s just diphenhydramine in a fancy costume.
Stop romanticizing suffering. Take the right pill. Sleep. Be present. Your baby deserves a functional mom, not a martyr.
And yes-I’ve been there. I took Benadryl once. My daughter stared at me like I was a ghost for three hours. Never again.
Aubrey Mallory
January 9, 2026 AT 06:31Let me just say this: if you’re still using Benadryl while nursing, you’re not being cautious-you’re being negligent. The science is settled. The AAP, WHO, Mayo Clinic-they’re not conspiracy theorists. They’re doctors. And they’ve seen what happens when moms self-medicate with first-gen antihistamines. Babies become lethargic. Feeding drops. Weight stalls. And then the guilt sets in. You didn’t mean to harm your kid. But you did. And now you’re scrolling Reddit looking for permission to keep doing it.
Stop. Just stop.
Loratadine. Cetirizine. Ibuprofen. Acetaminophen. That’s it. That’s the whole list. You don’t need more. You don’t need ‘natural.’ You don’t need ‘one more pill.’ You need clarity. And you’ve got it right here. Use it.
If you’re still unsure? Call your lactation consultant. Don’t trust a random post. Don’t trust your cousin’s friend’s sister. Trust the evidence. Your baby’s life isn’t a gamble. It’s a responsibility.
Prakash Sharma
January 10, 2026 AT 04:49India has been breastfeeding for centuries without these fancy American labels. My mom took aspirin, turmeric, and chai while nursing me-and I turned out fine. Now you’re telling me I can’t take a simple cold tablet because it has diphenhydramine? What next? Are we going to ban tea? Ban sleep? Ban motherhood?
You think your ‘science’ is better than tradition? We don’t have access to every pill you Americans hoard in your pharmacies. We use what works. And what works? Heat, rest, and patience. Not a pharmacy aisle.
This post reads like a corporate ad for Big Pharma. ‘Use Zyrtec!’ ‘Avoid Benadryl!’ Who profits from this? The same companies that sold you the idea that your body can’t handle natural stress.
Stop over-medicalizing motherhood. We’ve been doing this since before you were born.
Lois Li
January 10, 2026 AT 09:18Thank you for this. I’ve been so scared to take anything since my daughter was born. I had a migraine last week and just cried because I didn’t know if Tylenol was okay. I read the label twice. Triple-checked. Then I took one. And I felt like a criminal.
This post made me feel seen. Not judged. Not scared. Just… informed.
Also, I didn’t know about the hidden antihistamines in cold meds. I’ve been taking that ‘one-a-day’ thing for weeks. I’m throwing it out today. I’m so glad I found this.
For anyone else feeling like I did-you’re not alone. And you’re not failing. You’re just trying to be a good mom in a world that makes it feel impossible.
Joanna Brancewicz
January 10, 2026 AT 13:57Acetaminophen: 1-2% transfer. Ibuprofen: 0.6-0.8%. Half-life <4h. No significant pharmacokinetic interaction with breastfeeding physiology. FDA L1/L2 classification. No documented adverse infant outcomes in meta-analyses. First-gen antihistamines: CNS depression risk, anticholinergic effects, potential galactagogue suppression. Second-gen: negligible milk transfer. Label scrutiny mandatory. Combination products: high-risk. Single-agent dosing: gold standard.
Evan Smith
January 10, 2026 AT 14:43So… let me get this straight. I can take Tylenol, but not the ‘NyQuil’ that says ‘for colds and allergies’? But I can take Zyrtec, but not the ‘Zyrtec-D’? So the ‘D’ is the bad part? And I’m supposed to know that because… I read the tiny print? On a bottle I’m holding while holding a screaming baby?
Bro. I’m exhausted. I’m not a pharmacist. I’m a mom who just wants to sleep through the night without my head splitting open.
Can we just make a list? Like, ‘Safe’ and ‘Not Safe’? With pictures? Maybe emojis? 🟢 Tylenol. 🔴 Benadryl. 🟡 Only if you have a PhD in label reading?
I love you for writing this. But also, I need a cheat sheet. Send it to my DMs.
Annette Robinson
January 12, 2026 AT 05:17I’m a nurse and a mom of three. I’ve seen what happens when mothers don’t know what’s safe. I’ve held babies who couldn’t feed because their mom took Benadryl for a cold. I’ve watched moms cry because they thought they were failing.
This isn’t about fear. It’s about empowerment. You don’t have to suffer. You don’t have to choose between your health and your baby’s. You just need to know which tools to use.
Take the ibuprofen. Take the Zyrtec. Take the Tylenol. Time it after a feed. Watch your baby. Trust your gut.
And if you’re still unsure? Ask. Don’t Google. Don’t ask Reddit. Ask your OB, your pediatrician, your lactation consultant. They’re there to help. Not to judge.
You’re doing better than you think.
Luke Crump
January 13, 2026 AT 08:41Let’s be real-this entire post is a corporate marketing campaign disguised as ‘science.’
Who benefits from you avoiding Benadryl? The companies selling Zyrtec and Allegra. Who profits from you buying single-ingredient pills? The same ones who sold you the idea that ‘natural’ is dangerous.
For centuries, mothers used willow bark, honey, steam, and rest. Now? We’re told to buy a $40 bottle of cetirizine because ‘studies show.’
What studies? Who funded them? Did the same people who made Benadryl also fund the ‘safe’ alternatives?
And why is it so taboo to say, ‘I don’t know, but I’ll wait it out’?
We’ve turned motherhood into a pharmaceutical subscription service. And you’re paying for it.
Just breathe. Your baby will be fine.
Dave Old-Wolf
January 14, 2026 AT 20:40My wife took ibuprofen for three weeks after our son was born. No issues. No drop in milk. He slept fine. Ate fine. Grew fine.
Then she tried one Benadryl for a bug bite. He slept for 10 hours straight. Didn’t wake for a feed. We panicked. Called the pediatrician. They said, ‘That’s why we don’t recommend it.’
She hasn’t taken it since. And honestly? I’m glad we didn’t just ‘wing it.’
This post saved us. Thanks.
Donny Airlangga
January 15, 2026 AT 06:48Just wanted to say-this is the kind of info I wish I had when I was new. I took a cold pill with chlorpheniramine because ‘it was just one.’ My daughter was so sleepy she missed two feeds. I felt awful.
Now I keep a printed list on my fridge: Safe / Not Safe. I even showed my mom. She said, ‘Back in my day, we just toughed it out.’
But we’re not back in her day. We have better tools. Let’s use them.
Molly Silvernale
January 15, 2026 AT 22:04It’s funny… we live in a world where we can track our ovulation with an app, but we’re terrified to take a pill that’s been studied in over 500 nursing mothers… because… what? Because it’s ‘chemical’? Because it’s ‘synthetic’? Because it doesn’t smell like lavender?
Let me ask you this: if your baby had a fever, would you wait for the moon to be in the right phase before giving Tylenol? Or would you do what works?
Science isn’t the enemy of motherhood. Ignorance is.
And the real tragedy? The moms who don’t take meds because they’re scared… and then suffer in silence. That’s the real cost.
Take the Zyrtec. Take the ibuprofen. Breathe. You’re not poisoning your baby. You’re taking care of yourself. And that’s the most loving thing you can do.
Kristina Felixita
January 16, 2026 AT 07:31I’m from Indonesia and we have this thing called ‘jamu’-herbal drinks for everything. My mom drank it while nursing me. Now I’m in the US and everyone’s like, ‘Don’t take that!’
But I also read this post and realized-some things are legit. Like, Zyrtec? Safe. Benadryl? No.
So I made a little chart: jamu = okay in small amounts, Tylenol = okay, Benadryl = NOPE.
My baby’s fine. I’m fine. And I’m not ashamed to use science AND tradition.
Just… check the label. Always.
christy lianto
January 16, 2026 AT 15:38STOP. Just stop. You don’t need to suffer. You don’t need to feel guilty. You don’t need to be a martyr. You’re not a bad mom for taking Tylenol. You’re a good mom for knowing what’s safe.
I used to think ‘natural’ meant better. Then I spent three days in the ER because I didn’t take ibuprofen for a migraine and ended up screaming through my baby’s first bath.
Good health isn’t about purity. It’s about function.
Take the meds. Feed your baby. Sleep. Repeat.
You’ve got this. I believe in you.
Ken Porter
January 16, 2026 AT 20:50TL;DR: Use Zyrtec. Don’t use Benadryl. Ibuprofen good. Naproxen bad. Read labels. Done.
swati Thounaojam
January 17, 2026 AT 22:19Thanks for this! I took a cold med with diphenhydramine and didn’t realize it till my baby was super sleepy. I felt so bad. Now I always check the ingredients. I’m learning!
Manish Kumar
January 18, 2026 AT 18:16That’s exactly what happened to me. I thought ‘it’s just one pill.’ Turns out, one pill was enough to turn my 4-month-old into a zombie. He didn’t cry. Didn’t feed. Just stared. I panicked. Called the pediatrician. They said, ‘You just gave him a sedative.’
Turns out, the label said ‘PM’ and I didn’t know what that meant.
Now I keep a printed list on my fridge. And I never, ever take anything with ‘PM’ or ‘Night’ in the name again.
It’s not about being perfect. It’s about being informed.
Thanks for the reminder.